The A1C is a blood test that gives us an estimated average of what your blood sugar has been over the past 2-3 months. The A1c goes by several different names, such as Hemoglobin A1C, HbA1C, Hb1C, A1C, glycated hemoglobin, glycohemoglobin and estimated glucose average.
What is Hemoglobin?
Hemoglobin is a protein in your blood cells that carries oxygen. When sugar is in the blood, and it hangs around for a while, it starts to attach to the red blood cells. The A1C test is a measurement of how many red blood cells have sugar attached. So, if your A1C result is 7%, that means that 7% of your red blood cells have sugar attached to them.
What are the Symptoms of a High A1C Test Level?
Sometimes there are NO symptoms! That is probably one of the scariest things about diabetes, your sugar can be high for a while and you may not even know it. When your blood sugar goes high and stays high for longer periods of time you may notice the following:
- tired, low energy, particularly after meals
- feel very thirsty
- you may be peeing more than normal, waking a lot in the middle of the night to go
- dry, itchy skin
- unexplained weight loss
- crave sugar, hungrier than normal
- blurred vision, may feel like you need new glasses
- tingling in feet or hands
- cuts or sores take a long time to heal or don’t heal well at all
- frequent infections (urinary tract, yeast infections, etc.)
When your blood sugar is high, this means the energy that you are giving your body isn’t getting into the cells. Think about a car that has a gas leak. You put gas in, but if the gas can’t get to the engine, the car will not go. When you eat, some of the food is broken down into sugar and goes into your bloodstream. If your body can’t get the sugar to the cells, then your body can’t “go.” Some of the sugar that is building up in the blood, you end up peeing out. When you pee out some of your sugar, you will see dehydration, increased risk of infection, and weight loss. Ultimately, your cells don’t get the energy they need and your body starts to breakdown. Medication and/or lifestyle changes can help to get your body up and running properly again.
How Often Do You Measure A1C?
Your doctor will want to see what your A1C results is 2-4 times a year, and will typically order this lab with other important labs when it’s time for your blood draw. You can buy at home A1c test kits at your local pharmacy for approximately $20-$40. The kits in this price range usually include 2 tests and you can see the results in about 5 minutes. It is possible to see a significant change in your A1C in a one month time period, but the test typically isn’t done too often because red blood cells only turnover about every 120 days. On the plus side, if you have made some changes in the month prior to going to visit your doctor, those positive changes in the last 30 days are going to make more of an impact on your result than what you did 2 months ago.
What is My Goal?
It’s important to talk to your doctor about what your individual A1c goal should be. Typically the younger and healthier you are, the lower your A1c should be. For example, if you are 25yr old and have Type 1 diabetes and you are healthy, your doctor might recommend an A1C in the range of 6-6.5%. On the other hand, if you are 75 yr old with Type 2 diabetes, with a history of a heart attack and a stroke, your doctor might recommend an A1c of 7.5-8%. Your doctor will take into account your age, your general health, your risk of hypoglycemia, other health conditions/complications and your ability to care for yourself, when it comes to choosing the right A1C goal for you. Young children with Type 1 diabetes have a different set of goals due to the dangers and risk of hypoglycemia.
If your A1c is at the target goal that you and your doctor have agreed upon, and you are at low risk for complications, your doctor may only check your A1C every 6 months. If you have Type 1 diabetes, a more complicated treatment regimen or if you have recently had higher blood sugar than normal, your doctor may choose to get your A1C checked at least every 3 months.
American Diabetes Association Goals
| Age | ADA A1C goal |
| 19 yr and under | 7.5% |
| *Adults | 7% |
- A1C should be individualized based on age, how long they have had diabetes, complications present, risk of hypoglycemia, quality of life, life expectancy
How Accurate is the A1C Test?
The A1C test has been standardized by the National Glycohemoglobin Standardization Program (NGSP). In the past, the A1C test was not used to diagnosis diabetes because there were many different types of A1C tests and the results could vary. The A1C is now standardized, and the acceptable variance can be up to 0.5% from what your actual result is. So if you result is 6.5% your actual reading could be anywhere from 6-7%. The A1c test is only one measure of your overall blood sugar control. You will also have a good idea of how well your diabetes is controlled by your daily blood sugar checks and how consistent you are with your medications and lifestyle interventions.
I suggest also reading these articles:
There are some health conditions that could effect the accuracy of the A1c:
- Iron deficiency anemia may cause your A1C result to be falsely high.
- Blood loss from surgery, heavy menstrual cycles, other types of anemia may cause your A1C to be falsely low.
- Sickle cell anemia or thalasemmia may cause your A1C to be abnormal.
- Liver disease may cause your A1C to be abnormal.
- Kidney Failure may cause your A1C to be abnormal.
Talk to your doctor if you have any of these conditions.
Paying for A1C Test
Insurance typically covers your A1c test 2-3 times per year. Every plan is different so if there is any question, you should check with your insurance company directly. Be sure to check if they have a specified amount of time between the tests. If you want to have the A1c test done more often and your insurance says they won’t pay, you could always do the at home test and get similar results.
Preparing for the A1C Test
An A1c test alone does not require you to be fasting, but your provider is likely drawing other labs at the same time and some of those may require you to be fasting. You should always check with your doctor to see if the labs they are drawing require you to be fasting or not. If so, you are better off scheduling your lab draw shortly after you wake up so that you don’t have to go too long without eating, especially if you take any diabetes medications that could cause a low blood sugar reaction. Once your blood has been drawn, the results can come back as soon as an hour or as long as several days. How quickly the results come back depends on the lab and if they process it in house or if it has to be sent out. Steroids can cause high blood sugars and depending on the dosage and duration of use, they could effect your A1C result. Drinking plenty of water before a blood draw is also important.
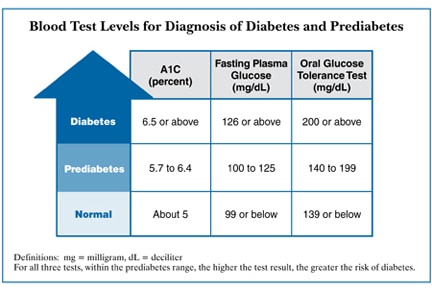
Diagnosing with and Interpreting the A1C
The A1C test is one way to diagnose diabetes. A fasting plasma glucose, oral glucose tolerance and a random blood glucose >than 200 with signs and symptoms of diabetes are all acceptable ways to diagnose diabetes. The important thing to remember is that each test must be repeated and there needs to be 2 abnormal lab results for a diagnosis. For instance, if someone had an A1c of 6.6% and a FPG of 135, that would be considered a diagnosis of diabetes. Or if a person had two subsequent A1C’s at 6.5% or above, that would also be a diagnosis.
Once you have been diagnosed, you and your doctor will want to know your A1C is on a regular basis. The test is an indicator of your risk for complications and gives your provider feedback on how well the treatment plan is working. Diabetes is a progressive disease and what works now for treatment, may not be the same thing that works 2 or 3 years from now. Knowing your numbers can help you stay on top of your treatment and possibly prevent complications.
Making Sense of the Numbers
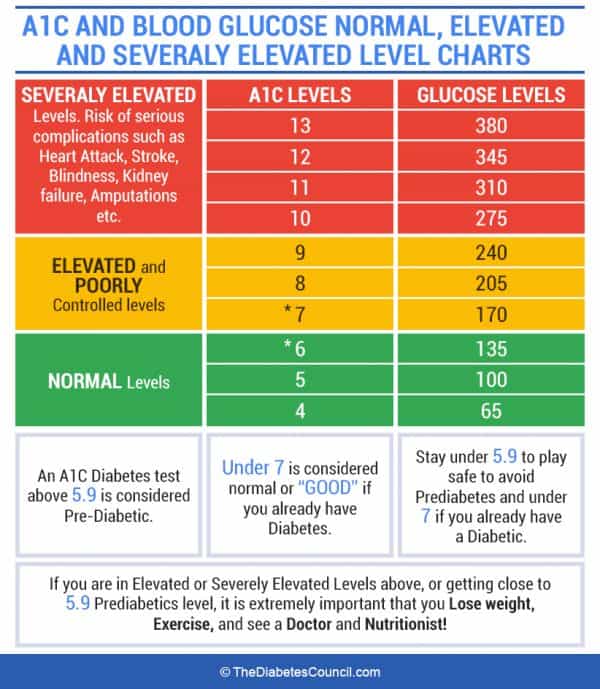
There are charts available that tell you your estimated average glucose (eAG) value, based on your A1c test result. For instance, if your A1c comes back at 8%, that may not mean a whole lot to you. The eAG translates the A1C into what our average glucose would read on our monitor if we checked blood sugar all day, every day, for the previous 2-3 months. So, and 8% A1C is an estimated blood glucose average of 183mg/dl. Milligrams per deciliter (Mg/dl) is the unit of measurement used in our blood sugar monitor. One thing that the A1C test does not account for is daily variability. For example, Bob’s blood sugar could range from 50-300 on a regular basis and Mary’s blood sugar could range from 120-250 on a regular basis, but they both could actually end up with the same A1C. That wide variability is being studied in more detail because many health experts wonder if variability in your daily blood sugars matter just as much, or more, than what your estimated average blood sugar is. Regardless, studies have shown us that if your A1c is 7% or lower, you’re risk for certain complications related to diabetes is lower.
| A1C Test Result % | Estimated Average Glucose (eAG) mg/dl |
| 6 | 126 |
| 7 | 154 |
| 8 | 183 |
| 9 | 212 |
| 10 | 240 |
| 11 | 269 |
| 12 | 298 |
| 13 | 326 |
Source: Adapted from American Diabetes Association. Standards of medical
care in diabetes—2014. Diabetes Care. 2014;37(Supp 1):S14–S80, table 8.
An A1c less than 7% means your a in a healthy range. When your result is between 7-9%, this is a time your should be cautious and start troubleshooting your elevated readings. Once your A1c is 9% and higher, immediate action should be taken to get your sugars down because you are in a dangerous zone. When A1c is higher, think of your blood as a thicker substance like syrup. When “syrup” travels through your blood vessels, it can do some damage, especially if your blood sugar goes high and stays high for long periods of time. Your tiny blood vessels were designed to carry blood that is more like water, than sticky syrup. When your heart has to pump to pump thick, sticky blood through the blood vessels over and over, damage can occur. This makes your heart work harder and your blood vessels were not designed to carry this thick sticky substance. High blood sugar can impact every part of your body. The only way to really know if your A1C is elevated is to get it checked regularly. Make sure you always ask what your actual result is. You are the best person to manage your diabetes and you need to make sure you have all the information available to you. Plus, it’s nice to see when your hard work pays off! Any decrease in A1C should be celebrated. So if your last test result was 10%, and this time it’s 9.3%, give yourself a pat on the back, it’s moving in the right direction.
If you didn’t have a chart to show the conversion from A1c to estimated average glucose (eAG), you could use the following calculation: 28.7 x HbA1c — 46.7 = eAG (in mg/dl). But, my guess is that you won’t commit that calculation to memory, so the next time you are wondering what a 7.2% A1C equates to, you can easily find many conversion charts on the internet.
Managing My Numbers
Staying on top of your diabetes can seem like another part of full-time job. There are some routine things that you can do to reach and maintain your blood sugar goal:
- Get your A1C checked 2-4 times per year AND always ask what your number is.
- Make sure to stay hydrated before your lab tests. Being dehydrated can affect many lab results related to diabetes, so to prevent yourself from having to get your blood re drawn, keep yourself hydrated.
- Take your medications as prescribed. Talk to your pharmacist, doctor or diabetes educator about any issues related to taking your medication. Whether it be a side effect or just forgetfulness about taking it, your team can help you troubleshoot and come up with a better plan.
- Choosing foods close to nature and closest to their natural form can help keep your diabetes under control. For example, choose to eat an orange, rather than drinking orange juice, brown rice instead of white rice, and choose salmon or chicken rather than bologna or hot dogs. By lowering your overall calories, this will help lower your blood sugar. So if you have always wanted to try a vegetarian, paleo, Mediterranean diet (or whatever), go for it. The key to diet is to finding something that can work for the long haul, not something you feel forced to do that can only last a week or two. Check in with your dietitian to create a long term plan that will work for you!
- Move your body, especially after a meal. Taking a walk after you eat can do wonders for how your body processes your sugar and how well your medicine works. Regular exercise, spread throughout the week, totaling at least 150 minutes is one of the best natural treatments for diabetes.
Getting Back on Track
If your A1C slipped away from you and you got a number you didn’t like on your last A1c test.
Start an investigation.
Let’s look at the evidence:
- Blood Glucose (BG)Checks
- How often have you been checking blood sugars?
- What kind of patterns do you see? Highs? Lows?
- What time of day do you notice patterns of highs or lows? Can you identify the cause?
- Medication check
- Has anything kept you from being consistent with your meds?
- Any side effects?
- How long have you been taking these same meds?
- Have any medications been added for infections or inflammation (can cause high BG)?
- Where have your medications been stored?
- Food Check
- Has anything changed with your diet? (visitors, traveling, finances, holidays, etc)
- Have you felt hungrier lately?
- How many times a week do you eat out?
- Are your portions larger than normal?
- Do you eat while doing other things, like watching TV or while on the computer?
- Exercise Check
- Have you been exercising less or not at all?
- Have you changed the type or intensity of exercise?
- Did you have an injury that prevented you from exercising?
- Stress Check
- Have you been under more stress than usual?
- How do you relieve the stress?
Once your have investigated and looked at the evidence, you may be able to pick 1 or 2 things to work on. Little changes can often translate into big results over time!
Frequently Asked Questions:
Can my A1C levels be too low?
Yes, especially if you are on diabetes medications and have had symptoms of hypoglycemia (low blood sugar). If you have a really low A1c, less than 6% and are experiencing hypoglycemia, then your doctor may want to adjust your medications. On the other hand, if you are not on diabetes medications and have not been having symptoms of hypoglycemia and your A1C is low, then that is great.
How can I lower my A1C levels while pregnant?
Staying active, choosing healthy foods, taking medicine if prescribed, avoiding sugary drinks/junk food, are the best way to keep your blood sugars in target while pregnant. It’s also important to gain the right amount of weight. “Eating for two” is a myth. The baby is so small, that during the first trimester no additional calories are needed and by the second and third trimester the amount of extra calories needed would equal 1c of milk and ½ a sandwich. Talk to your doctor about a healthy weight gain goal.
What medication can reduce the A1C levels?
All classes of diabetes medications were designed to lower blood sugars and A1C. Some medications will lower your A1C more than others. If you are already on one medication but your A1C is not at target, your doctor may consider adding an additional medication to help. It is common to be on more than one diabetes medication at a time.
What do I do if my A1C levels are slightly elevated?
If your blood sugars are only slightly elevated, you may just increase your exercise or tweak your diet by adding more vegetables, maybe you just got off track. It can be helpful to do more blood sugar checks during this time as well so you know what time of day your blood sugar is the highest and work on a plan to target those specific times.
What is the A1C limit for Department of Transportation (DOT)?
The DOT requires your A1C to be less than 10%, but there are also other restrictions regarding hypoglycemia, complications related to diabetes, and insulin. You can work with your doctor to make a plan to keep your commercial driver’s license (CDL). Addressing your diabetes early on is one step you can take to preserving your license.
Can the A1C test be used during pregnancy?
If you have Type 1 or Type 2 diabetes prior to pregnancy, the doctor will likely continue to check your A1C. It is uncommon to use an A1c test in gestational diabetes because it typically doesn’t show up until 24-28 weeks of the pregnancy. Since an A1c test measures up to the last 120 days, this test would not be as relevant in gestational diabetes. Remember, if you experience anemia in pregnancy, this could produce a false A1C result. Daily blood glucose checks tend to be more beneficial in managing blood sugar during pregnancy.
Can the A1C test result in a different diagnosis than the blood glucose tests?
Yes, that is why it’s required to have 2 lab tests showing abnormal values in order for a diagnosis to be made.
Are diabetes blood test results always accurate?
The tests that we have to diagnose diabetes are held to the high standards of lab tests that were used in landmark diabetes studies. With that said, labs can sometimes make errors. If you or your doctor question your results, consider having the labs re drawn.
Will vitamins help my A1C levels?
Vitamin D, Calcium, and Magnesium are all vitamins that may help to improve insulin resistance, which in return could improve your blood sugar control. You should talk to your doctor or dietitian before starting any vitamins or supplements to find out which ones would be best for you.
Can I drink alcohol if I have high A1C test results?
Alcohol is a tricky subject. Depending on the type you drink, could either increase drastically or lower your blood sugar. Sweet drinks like margaritas or anything mixed with soda is more likely to raise your blood sugar. Hard alcohol or some shots, could actually prevent your liver from being able to produce sugar and could cause a low blood sugar, especially if you take diabetes medications. Also, many medications in general are not indicated for use with alcohol. So, generally speaking, avoiding alcohol when you have diabetes and are on medications is best. If you prefer not to avoid alcohol, then have a talk with your doctor about how often and how much is appropriate for you.
Use the converter below to translate your A1C percentage into an eAG number, or vice versa.
Is there a perfect a1c level? The American Diabetes Association recommends the general population of people with diabetes maintain a blood sugar of 7% or less to reduce risk of complications. The American Association of Clinical Endocrinologists state that people with low risk of complications and no other major health issues should have an A1C of <6.5%. But the general consensus from all major health organizations setting A1C goals is that these guidelines should be adjusted based on each individual and their circumstances.
Bottomline
The A1C test is a very useful test in helping people with diabetes and their doctors gauge how well their treatment plan is working. It’s important for people with diabetes to understand this test result and be in charge of their diabetes management. With that said, there are also many other ways to decide if your treatment plan is working. The A1c is not the end all be all! On a day to day basis you may use your blood sugar monitor throughout the day to give you information about how your medications, exercise or eating plan is working. People also pay attention to how they feel and what their energy level and mood is like. Some people are actively striving for weight loss, so they are stepping on the scale weekly. The most important thing is to have small daily measures to help keep you on track, so when you get that A1C done every 3 months or so, you don’t get caught off guard.
Further reading:
My hope is that you have a better understanding of what an A1C test is and how it is used. If your have other questions or if you would like learn more about me and how I can help you, please write in the comments below. And also share this article with anyone who might need a diabetes guide.
Angela Manderfeld, MS, RD, LD, CDE
Registered Dietitian and Certified Diabetes Educator
Why you should trust us?
Angela Manderfeld, MS, RD, LD, CDE, is a highly esteemed Registered Dietitian and Certified Diabetes Educator. Her distinguished credentials testify to years of rigorous education, extensive hands-on experience, and a steadfast commitment to excellence in the field.
Angela adheres to strict evidence-based practices, meaning all advice and recommendations provided are backed by the most current and comprehensive research available. As a Certified Diabetes Educator, she brings an exceptional level of expertise to the often complex task of managing diabetes. Angela's integrity, dedication, and passionate pursuit of advancing health and wellbeing instill a high level of trust.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on June 2, 2023
References:
-
- https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis/a1c-test
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3632159/
- https://www.ncbi.nlm.nih.gov/pubmed/15345893
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4515445/
- https://www.ncbi.nlm.nih.gov/pubmed/19317814
- http://care.diabetesjournals.org/content/26/4/1147