At the clinic today, a patient came in for an initial assessment for Diabetes Self-Management Education. She was taking thyroid medication along with her diabetes and other medications. She was not the first patient that I have seen lately who is taking thyroid medication. I was aware of the link between diabetes and thyroid disease, and had some basic information. I thought it would be interesting to look into the dynamics a little further. After all, the pancreas and the thyroid both fall within the endocrine system. Now let’s take a look at why people with diabetes often seem to have thyroid disorder, and the reasons behind it.
Contents
What is thyroid disease?
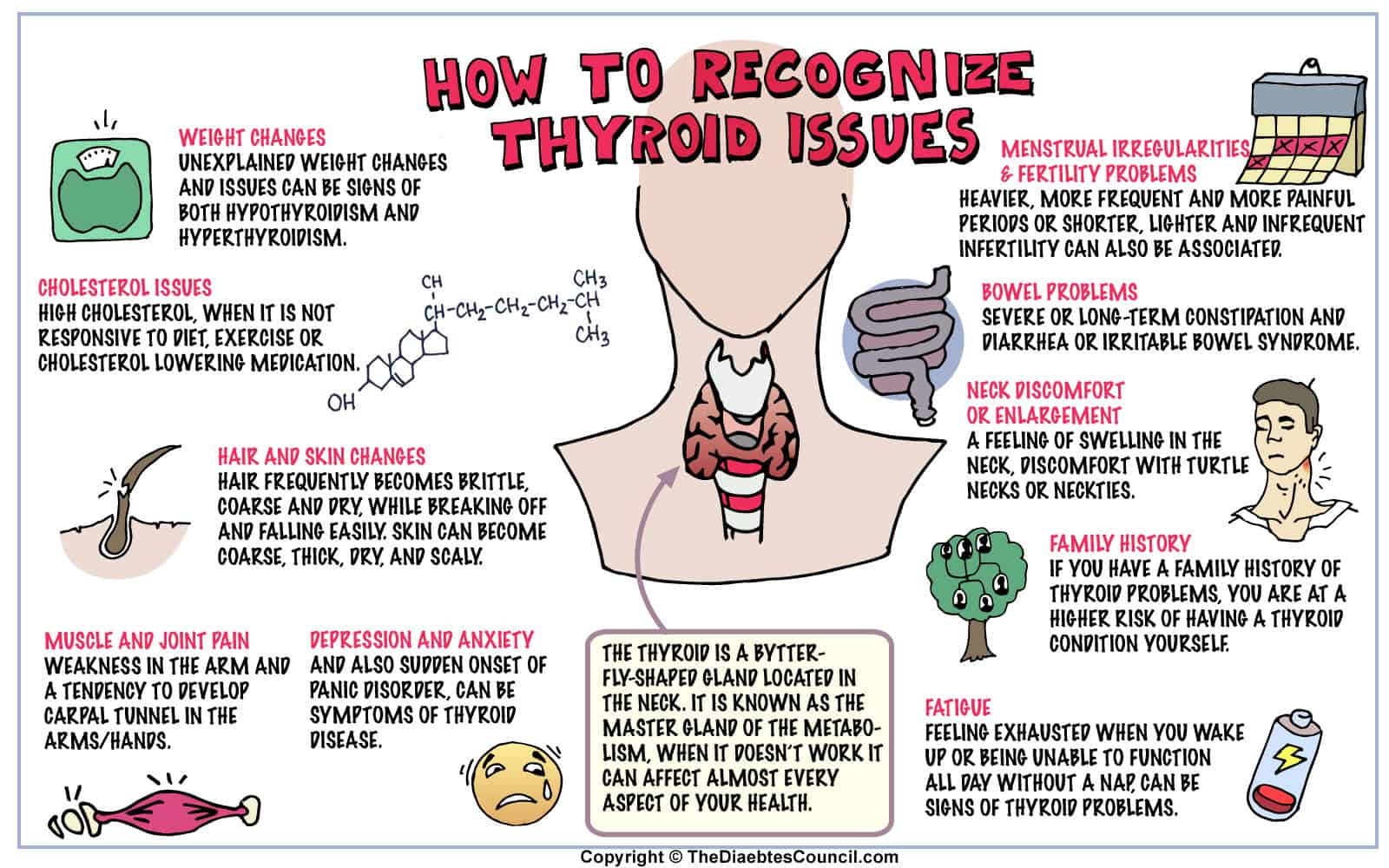
In order to understand the relationship between diabetes and thyroid disease, it is helpful to understand what thyroid disease is.
At the front of your neck, just under your Adam’s apple is where you will find the thyroid gland. Thyroid disease is a problem that happens when the thyroid gland either under produces or over produces the thyroid hormones. Thyroid hormones are responsible for regulating the body’s metabolism.
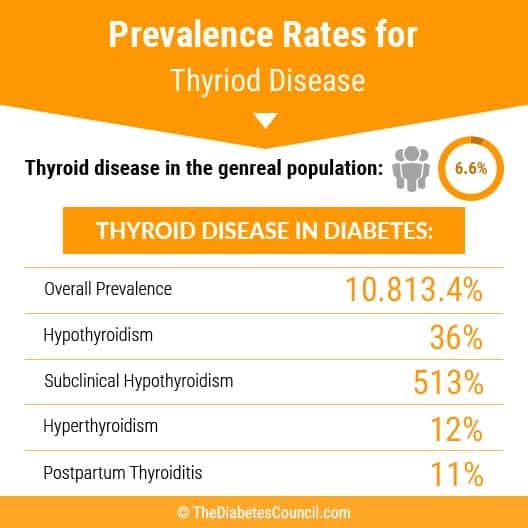
From research, the percent of the population that will develop thyroid disease is 7 percent. The percentage of people with diabetes who have thyroid disease is greater than the general population. We will dig in a little deeper to find the reasons why, and examine the link between the two.
Note from Kirk and Health Institute:
A high percentage of low thyroid is “Hashimoto’s”, which like Graves disease is an auto-immune in origin and most often creates low thyroid symptoms. To address Hashimoto's and Graves affectively you must focus on the immune system, medication can be supportive but does not address the cause. Autoimmune conditions are best managed by change in diet and reducing inflammation.
Types of thyroid disease
There are different types such as:
Hypothyroidism
Hypothyroidism happens when the thyroid gland under produces thyroid hormones. Symptoms often depend on the severity of the thyroid hormone deficiency. Most of the time, the symptoms develop slowly, and may include fatigue and weight gain. As metabolism slows down, symptoms tend to worsen, and become more obvious. At this point, people who generally attribute their fatigue and weight gain to simply getting older, may have to seek medical attention for their symptoms. Women develop thyroid disease more often than men.
Note from New Life:
For causes of thyroid disease – The number one cause of hypothyroidism in the US is an autoimmune disease called Hashimoto’s. About 80% of thyroid disease suffers have this, but most do not know about it because it is rarely tested.
The reason why people with Type 1 diabetes are more likely to have hypothyroidism is because type 1 diabetes is autoimmune and most of hypothyroidism is autoimmune as well (many people don’t know this). Once you have one type of autoimmunity, you’re more likely to have multiple autoimmune diseases.
Symptoms of Hypothyroidism
- Fatigue
- Sensitivity to cold
- Constipation
- Dry skin
- Weight gain
- Puffy face
- Hoarseness
- Muscle weakness
- Elevated cholesterol level
- Muscle aches, stiffness, and tenderness
- Pain, stiffness, swelling in joints
- Heavier and/or irregular menstrual periods
- Thinning hair
- Slowed heart rate
- Depression
- Impaired memory
If left untreated, hypothyroidism can result in a goiter, which is basically an enlarged thyroid gland. The goiter develops due to increased stimulation of the thyroid gland, causing it to produce too many hormones. Memory and depression symptoms may worsen as thyroid problems get worse.
I suggest reading the following articles:
Causes of hypothyroid disease
Too much treatment for an over active thyroid can send you into a hypothyroid state. Thyroid surgery, radiation therapy, autoimmune diseases, and certain medications can cause hypothyroid disease. Other less common causes of hypothyroid disease include congenital disease, or a disease that a person is born with, absence of thyroid or defective thyroid gland, pituitary disorders, pregnancy, and iodine deficiency.
Note from Stop the Thyroid Madness:
The two main causes that we as thyroid patients see in each other is Hashimoto's, the autoimmune version (which I think you need to specifically mention instead of just saying "autoimmune") and genetic thyroid mutations.
Advanced Hypothyroid disease, or Myxedema Coma
Myxedema is an advanced form of hypothyroidism, and can be deadly. Although rare, low blood pressure, low body temperature, and decreased breathing leads to unresponsiveness, coma, and even death. It usually occurs in the elderly when the thyroid has been compromised somehow, such as with a stroke or other life threatening medical event. Mentation may be decreased, and electrolytes can be off balance with severe hyponatremia. Myxedema also refers to a skin condition that occurs with hypothyroid disease, and sometimes with hyperthyroid disease. Myxedema coma, however, can occur with or without myxedema.
Hypothyroid disease in children
We generally think of thyroid problems occurring around middle age and beyond, with mostly women being affected by it. Hypothyroid disease can and does also occur in infants. When a baby is born without a thyroid gland, or when a baby’s thyroid gland doesn’t work properly, there will be few noticeable symptoms in the beginning. When symptoms do arise, they include:
- yellowing of the skin and eyes (jaundice)
- difficulty with choking
- large and protruding tongue
- edema or puffiness of the face
- failure to thrive
- poor muscle tone
- constipation
- sleepiness
- severe case – mental and/or physical retardation
When children and teens get hypothyroid disease, they have about the same symptoms as adults. In addition to symptoms, they may also experience:
- short stature and poor growth
- permanent teeth never develop
- late puberty
- Poor mental development
Note from Stop the Thyroid Madness:
Thyroid problems are starting for a huge body women in young adulthood, not middle age. Yes, it does occur mostly with menopause, too, but a large body of us see it in our 20's and 30's.
Should I see a doctor?
If you start feeling tired often, and there really isn’t any reason behind your lethargy, have dry skin, a puffy face, problems with constipation, or your voice is sounding hoarse, see your doctor. You may have hypothyroid disease. Your doctor will request tests to check the functioning of your thyroid gland. If your cholesterol is high, and you have tried measures to improve your diet, then it’s possible that an under active thyroid is the problem. Ask your doctor if it could be your thyroid.
What if I already have thyroid problems?
If you have had any surgery on your thyroid gland, been treated with any medications for thyroid, or had radioactive iodine treatments on your neck, head, or chest, you will need periodic testing to confirm thyroid function by your healthcare provider. After these treatments, and over time, your thyroid can fizzle out, so you need to have it checked regularly.
If you already take thyroid medication, your healthcare provider will let you know how often you will need check-ups. Medication doses may need to be changed as time goes on.
Untreated hypothyroid disease
Untreated hypothyroid disease can lead to a number of serious conditions, including:
- goiter
- heart disease
- mental health issues / depression
- peripheral neuropathy
- myxedema
- infertility
- birth defects
Risk factors for hypothyroid disease
If you are a female, and you are over the age of 60, you have an increased risk for thyroid disease. If you have an autoimmune disease such as lupus or rheumatoid arthritis, have a family history of thyroid disease, have been treated with radioactive iodine or anti-thyroid medicines, received radiation treatments to the head or neck area, or been pregnant or delivered a baby within the past 6 months, you may be at risk for thyroid disease.
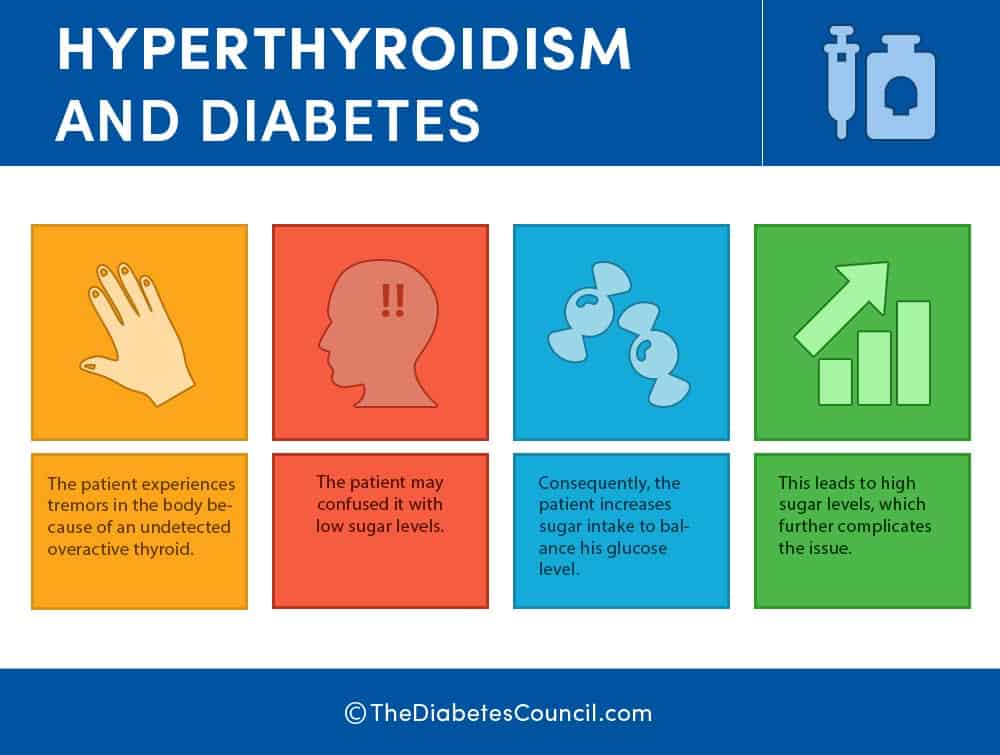
Hyperthyroidism
Hyperthyroid Disease occurs when the thyroid overproduces thyroid hormones, causing metabolism to speed up. The thyroid makes two specific hormones, T3 and T4 that are responsible for regulating the body’s metabolism and how a body cell uses energy. Weight loss, weakness, irregular heartbeat, and difficulty sleeping are some of the most common symptoms. Graves’ disease is an autoimmune disorder, and is also the cause of hyperthyroidism. It also occurs more often in women than in men. It is genetic, and you should let your doctor know if you have any body in your family who has Graves’ disease.
Note from Dr. Patty Powers:
- For hypothyroidism, nutrient deficiencies (zinc, selenium, iron, protein) can also cause hypothyroidism in addition to too little iodine.
- Stress and hypothalamic adrenal dysregulation (commonly known as adrenal fatigue) can cause abnormal thyroid function, and giving someone a thyroid hormone pill will not make them feel better if you don’t get to the underlying cause/s of thyroid hormone dysfunction.
- Graves is A cause of hyperthyroidism, not THE cause of hyperthyroidism.
How things work
Thyrotoxicosis
Anytime the three glands over produce hormones, there is a danger of thyrotoxicosis. This is a toxic condition. It can occur no matter what the cause of the hyperthyroidism. Grave’s disease is the most common form of thyrotoxicosis, and is the only hyperthyroidism condition that affects the eyes. We will discuss Grave’s opthalmopathy below.
Causes of hyperthyroidism
There are many different conditions that can cause hyperthyroidism. One of them is Graves’ disease. Toxic adenoma, Plummer’s disease (toxic multinodular goiter) and thyroiditis can all be causes of hyperthyroidism. Your thyroid gland is responsible for many functions that regulate metabolism. The hormones produced regulate fat and carbohydrate metabolism, and help maintain a steady body temperature. They also help to regulate your heart rate, and play a part in the regulation of proteins and calcium.
Symptoms of hyperthyroidism
Hyperthyroidism has a certain symptomatology despite the cause. Mild hyperthyroidism may produce no symptoms. For the elderly, symptoms may also be absent. Symptoms worsen based upon the degree of hyperthyroidism. Symptoms are related to the increased metabolism that all of the extra thyroid hormones cause. It’s tough to differentiate it from other problems sometimes. The symptoms of hyperthyroidism are:
- Despite eating a regular amount of calories or an increased amount of calories, the patient will experience weight loss in a short period of time
- Heart rate greater than 100 beats per minute (tachycardia), arrythmia or irregular heartbeat, or palpitations (pounding heart beat)
- Increase in appetite
- Anxiety, irritability, nervousness
- Trembling of the fingers and hands (tremor)
- Sweating
- Changes in menstrual period, irregular periods
- Increased sensitivity to heat
- More frequent bowel movements, or changes in bowel movements
- Swelling in the neck (enlarged thyroid, or Goiter)
- Fatigue, muscle weakness
- Sleep disturbances
- Skin thinning
- Hair is brittle, thinning
The elderly may only exhibit symptoms that are subtle, such as increased heart rate, an intolerance to heat, and an increase in fatigue. Beta blockers for blood pressure can mask these symptoms in the older adult.
Graves' ophthalmopathy
Graves’ ophthalmopathy is uncommon, but may affect the eyes if you have hyperthyroidism, and especially if you smoke. This is the condition where the eyeballs protrude from the sockets of the eyes due to swelling in the tissues behind the eyes. The eyeballs can truly bop out of the orbits if the swelling gets bad enough. The eyeballs get dry from exposure. This condition seems to occur, and go away on its own without any treatment, but is part of the symptomatology of hyperthyroidism. Symptoms include:
- Eyeballs that protrude from the sockets
- Eyes that are red and swollen
- Discomfort and excessive tearing of the eyes
- Increased sensitivity to light, blurred or double vision, inflamed eye sockets with reduced eye movement
When to see a doctor
See your healthcare provider if you experience weight loss but are not trying to lose weight, a rapid heartbeat, sweating that is more than usual, swelling in the neck, or any other symptoms of hyperthyroidism that you experience. Talk with your healthcare provider about any other conditions that you may have. Other conditions mimic hyperthyroidism. If you are being treated for hyperthyroidism, see your healthcare provider as much as he or she recommends.
Now that you know most of what there is to know about thyroid disease, let’s talk about the link that exist between thyroid disease and diabetes. The pancreas and the thyroid are both in the endocrine system. The following is the prevalence of thyroid disease in people with diabetes, and breaks the numbers down by the type of thyroid disorder:
Thyroid disease in diabetes:
Overall prevalence: 10.813.4%
Hypothyroidism: 36%
Subclinical hypothyroidism: 513%
Hyperthyroidism: 12%
Postpartum thyroiditis: 11%
Can diabetes cause thyroid disease?
Although diabetes doesn’t cause thyroid disease, those who have an autoimmune condition, such as diabetes, are already at an increased risk for other endocrine disorders. Those with Type 2 diabetes are also at risk for thyroid disease, although the risk is not as great as that for a Type 1 diabetic. This is due to Type 1 diabetes being an autoimmune disease.
Can thyroid disease cause diabetes?
Thyroid disease does not cause diabetes no more than diabetes causes thyroid disease, but we will examine the link between the two in detail.
Thyroid disease and Type 1 diabetes
A study demonstrated an overall prevalence of 13.4% of thyroid diseases in people with diabetes with the highest prevalence in type 1 females with diabetes (31.4%). That is a 1 in 3 chance of having thyroid disorder if you have Type 1 diabetes, and are female. Researchers have found that because Type 1 diabetes is an autoimmune disease, and people with an autoimmune disease are more likely to have thyroid disease.
Thyroid disease and Type 2 diabetes
Those with Type 2 diabetes are also at risk for thyroid disease, although the risk is not as great as that for a Type 1. Of people with Type 2 diabetes, about 12 percent have thyroid disease. Researchers are not sure what the exact link between Type 2 diabetes and thyroid disease is, but they currently think that it may be due to the aging process.
How does the thyroid’s function affect diabetes?
Thyroid function has an effect on diabetes due to its role in regulating the body’s metabolism. Therefore, controlling your diabetes may be tough when the thyroid gland is out of whack. Also, thyroid disorder places a person with diabetes at an increased risk of diabetes complications, and can worsen many diabetic conditions, such as neuropathy.1
Blood glucose is affected by high thyroid levels or low thyroid levels. When thyroid levels that are too high, you will see an elevated blood glucose. This is because your body uses up your insulin faster. When there is hypothyroidism, the insulin is used up slower, so your blood glucose could drop low. Your thyroid does play an important role in maintaining regular blood glucose and insulin levels, so anytime it is out of whack, you could see a problem with your blood glucose, so you need to be aware of this is you have thyroid disease and diabetes.
Anytime your thyroid is low, you can have an increase in cholesterol, LDL, and even triglycerides. This on top of diabetes puts you more at risk for heart disease. You want to catch any problems with your thyroid quickly, and have them treated.
Due to the likelihood of problems from thyroid disease for people with diabetes, I feel that all people with diabetes should be screened for thyroid disorder, and treated promptly.2
Pregnancy, diabetes and the thyroid
What are the symptoms of thyroid disorder in pregnant women?
Pregnancy is a perfect time for thyroid issues to rear their symptoms. There are already hormonal changes going on, and that alone can trigger thyroid disease. Thyroid disease can endanger a developing fetus, so it is important for pregnant women with thyroid disease to get treatment. Treatments are considered safe for the developing fetus.
Medical professionals do not agree as to whether or not all women should be screened for thyroid disease. There is consensus where women with Type 1 diabetes are concerned, and healthcare professionals agree that all of these women should be screened for thyroid disease during their pregnancies. Since thyroid disease can pose a problem for the baby, women with thyroid disease who want to get pregnant should discuss the safety and monitoring that will be needed during pregnancy.
Gestational diabetes and thyroid
Since there is a link between Type 1 diabetes and thyroid disease, and a link between Type 2 diabetes and thyroid disease, then there must be a link between gestational diabetes and thyroid disease. Some researchers at the University Of Southern California Keck School Of Medicine in Los Angeles set out to find out.
Researchers are learning the difference in the incidence of gestational diabetes for patients with hypothyroidism and hyperthyroidism. They performed a chart review on women with clinical thyroid disease that were delivering babies at Johns Hopkins from 2005 to 2008.
Of the women with hypothyroidism, 14.3 developed Gestational Diabetes Mellitis. Comparatively, 5.8 percent of women with hyperthyroidism developed GDM. Patients with hypothyroid were more likely to have a caesarian section. Preterm delivery, hemorrhage postpartum or hypertensive pregnancy disorders showed no difference between the groups.
This would suggest that screening for GDM should begin early in those women with thyroid disease.3
Am I at risk? Should I get tested?

Blood tests for thyroid disease
Blood tests can determine if your body is producing antibodies in response to its own attack of the thyroid. You can find antibodies in the blood of people with an autoimmune type of thyroid disease sometimes, but they are not always present.
- TSH test – a low result (under 0.4 mlU/L) means hyperthyroidism, and a high result (over 0.4 mlU/L) means hypothyroidism. This is the most accurate test
- T4 test – gives more information, 4.5 to 11.2 mcg/dl is the normal range. A high level means hyperthyroidism, and a low level means hypothyroidism
- T3 test – helps in determining hyperthyroidism. Normal falls between 100 and 200 mg/dl. A high result means hyperthyroidism, and a low result means hypothyroidism5
Note from Dr. Miller at Anti Aging:
The diagnosis of diabetes is quite complex. As is the diagnosis of hypothyroidism. It is not simply by the numbers. If you are suffering from most the symptoms, then you make a clinical diagnosis and treat accordingly. The WHO definition is a FBS >125 mg or a 2 hr PP >200 mg. A HgA1c >6.5 is also consistent with a strict diagnosis. Improving thyroid status will improve metabolism. Not sure that lowers insulin levels thereby increasing glucose.
What thyroid treatment options are right for me?
Some treatment options available:
Hypothyroidism treatment
Hypothyroidism is treated with a daily pill, simple as that. Alternatively, there is a medication that replaces thyroxine in our body, which is a synthetic form of T4 hormone.
Hyperthyroidism treatment
The treatments for hyperthyroidism are more complicated than the treatments for hypothyroidism. There are anti-thyroid medications given to help combat high thyroid hormone levels in the body. It’s possible to get to remission of the disease with medications, but only about a third of patients actually do go into remission in the US.
When a person doesn’t respond to anti-thyroid medications, they are given radioactive iodine to reduce the excess thyroid hormone production. That often swings them in the other direction, and they end up having to take medication for hypothyroid. No matter how intimidating radioactive iodine sounds, it is considered safe and effective. There are also not many side effects, on a positive note. You should not become pregnant while taking iodine treatments.
Are thyroid and diabetes medication compatible?
Synthetic thyroid hormone can mix adversely with food and medications. Patients need to know that their thyroid medication will not mix well with soy, calcium, or iron supplements.
In addition, certain medications impair the absorption of thyroid medications, especially if they coat the stomach. Carafate is one culprit. Medications such as warfarin (coumadin) and other anticoagulants that thin the blood may need to have dosage adjustments because they alter thyroid hormone levels. Your healthcare provider or pharmacist can help you with any possible interactions by taking a look at the medications and supplements you are taking.
Further reading:
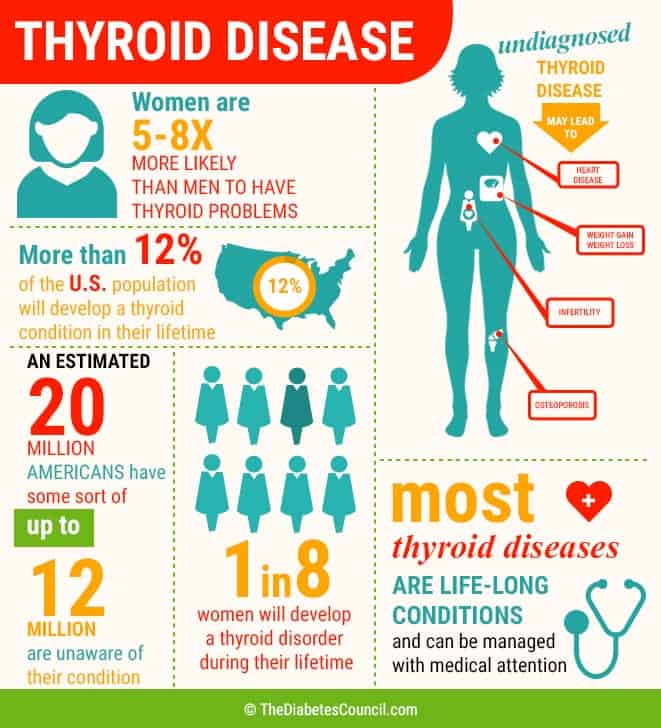
Thyroid disease facts from the American Thyroid Association
- More than 12 percent of the U.S. population will develop a thyroid condition
- An estimated 20 million Americans have some form of thyroid disease.
- Up to 60 percent (12 million) of those with thyroid disease are unaware of their condition.
- Women are five to eight times more likely than men to have thyroid problems.
- One in eight women will develop a thyroid disorder during her lifetime.
- Undiagnosed thyroid disease may put patients at risk for certain serious conditions, such as cardiovascular diseases, osteoporosis and infertility.
- Most thyroid diseases are life-long conditions that can be managed with medical attention.
For more information, visit the American Thyroid Association website at: www.thyroid.org .
Thyroid disease and diabetes research
In one study, the researchers found a tie between hypothyroidism and Type 2 diabetes. Even in the low normal range, low thyroid levels raise the risk of developing Type 2 diabetes. This was especially true in those people who already had pre-diabetes. The study included nearly 8,500 people. Adults with thyroid levels in the lower 33.33 percent had a 1.4 times higher risk of developing Type 2 diabetes than those with thyroid levels in the upper 33.33 percent.
Statin use for high cholesterol didn’t seem to make any difference in the risk. Those with pre-diabetes had a 40 percent higher risk of developing Type 2 diabetes if they also had thyroid disease.
Note from Loren Cordain from the Paleo Diet:
The most common of all autoimmune diseases, by far, is Hashimoto's thyroiditis. Recently, Alessio Fasano and his group at the University of Maryland have shown a strong link between type 1 diabetes and wheat consumption. Additionally, the link between wheat consumption and Hashimoto's thyroiditis has frequently been demonstrated in the medical literature. Clearly, causality has not yet been demonstrated between either type 1 diabetes, Hashimoto's thyroiditis and wheat consumption.
Over to you
We hope that you have learned something from this article about diabetes and the link to thyroid disease. January is National Thyroid Awareness Month, so we thought it would be a great time to do a comprehensive article. Please let us know your thoughts in the comments section below.
References:
- https://www.diabetesselfmanagement.com/about-diabetes/general-diabetes-information/thyroid-disorders-and-diabetes/
- http://www.healthline.com/diabetesmine/the-411-on-diabetes-thyroid-disease#3
- https://www.ncbi.nlm.nih.gov/pubmed/23461673
- http://www.diabetesforecast.org/2011/mar/detecting-thyroid-disease.html
- http://www.diabetesincontrol.com/hypothyroidism-tied-to-type-2-diabetes/
TheDiabetesCouncil Article | Reviewed by Dr. Jerry Ramos MD on June 01, 2020