If you’ve ever had a cut or sore that won’t heal, it could be an important sign of something wrong. If it’s taking several weeks for a wound to heal, it could have an infection in it from poor blood circulation and high blood sugars related to diabetes.
Many times, wounds that won’t heal properly are a sign of an underlying condition known as diabetes. If a person with diabetes has a wound that’s stubborn to heal, it can progress rapidly from infection to gangrene, requiring Amputation.
Contents
Causes of slow healing due to diabetes
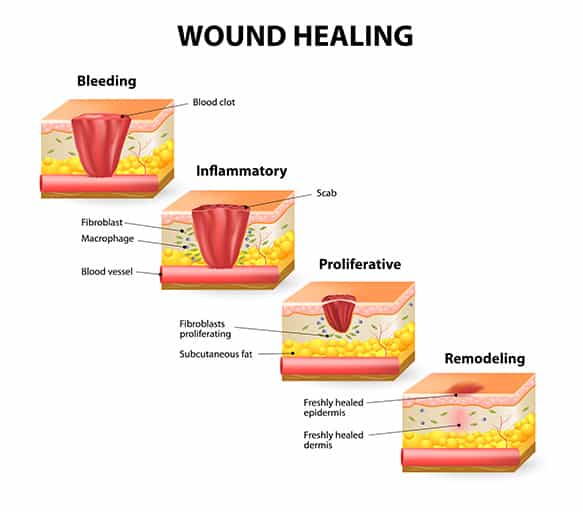
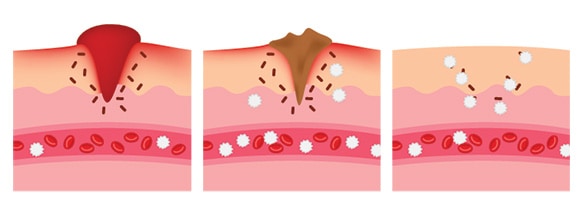
Once we get a cut or a scrape, our body starts to heal the injury right away. Our immune responses kick in, sending bacteria fighting cells that cause an inflammatory response that helps to prevent the wound bed from becoming infected. A scab begins to cover the wound and eventually, the wound heals in an optimal situation.
Factors such as the person’s health, the degree of injury and level of skin thickness that the injury entails, and the state of your disease states can affect the rate of healing. One disease state that particularly causes slow wound healing is diabetes. If it’s not controlled and blood sugars are high, wounds may fester and develop infections that can quickly lead to loss of limbs.
How is it a symptom of diabetes?
Several factors affect the healing of wounds in a person with diabetes.
High blood sugars
High blood sugars also affect nerve pathways causing nerve damage, or neuropathy. This further complicates poor circulation. It’s much more difficult for blood to get to the area and start the healing process.
High blood sugars affect the immune response in your body. They cause inflammation in body cells by preventing needed oxygen, nutrients and cells involved in repair of tissues from getting to where they need to go. This slows the entire process of healing down at the cellular level.
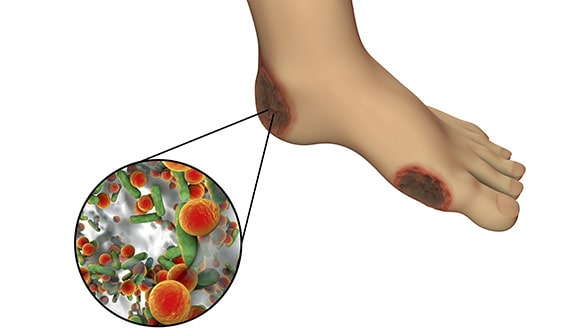
On top of bacterial infections, there can also be fungal infections and gangrene. Gangrene is when tissues in the wound bed die off, creating necrotic tissue (dead tissue). This tissue and the affected limb must be amputated to prevent infection in the blood and eventually death.
Nerve damage
Neuropathy caused by diabetes can occur in the periphery, in your arms and legs. This is also due to high blood sugars over time when nerve pathways are injured.
The result is feet and hands that can feel numb or have a “pins and needles” feeling. If you step on a sharp object or get one in your shoe that you don’t feel, it can result in a wound that can be difficult to heal, become infected and even progress to amputation of the affected limb.
Poor circulation
Vascular disease can occur in people without diabetes, but it’s particularly prevalent in this population. Blood thickens from high blood sugars, veins and arteries narrow and blood can’t get to your arms and legs like it used to.
This further complicates any wound healing that needs to occur in the extremities. In the arms and legs, when vascular systems are not delivering needed blood flow and oxygen and blood is thick, it’s referred to as Peripheral Vascular Disease, or PVD.
Other factors that affect wound healing with diabetes
One factor that affects wound healing is how well your immune system response reacts to sending bacteria fighting cells to clear the wound of debris and make way for healing. Another is the infection.
For Type 1
T1D is an immune attack on the pancreatic beta cells that destroys them, resulting in T1D with an absence of insulin production. Since the immune system is “off” in T1D, other immune responses can be slow or absent.
This includes the ability to fight infection in wound beds that develop, and the inability of the body to send enough bacteria fighting cells in there. Think of it as an army with not enough soldiers. They can’t get the job done to protect things.
High blood sugars in T1D can be severe if not managed appropriately, so this further complicates wound beds and healing processes in the person with T1D.
For Type 2
People with T2D also can develop severely high blood sugars if uncontrolled. They can have the same problems healing as those with T1D. They may not have as much of a problem with the immune response as T1D, but they are certainly at risk for non-healing ulcers and amputation.
People with T2D also need to check their feet daily and manage their blood sugars in their target range.
I suggest reading the following articles as well:
- Carbs vs Smoking: Which One is Worse And Which One is Easier To Give Up?
- How Do Others Live With Diabetes?
- What Diabetes Supplies Do I Take With Me When I Leave The House?
- How To Prevent Hospitalization As A Result Of My Diabetes Part 1
- 10 Things Diabetics Do To Better Self-Manage
- Diabetes Meal Delivery Programs & Services
Recognizing signs of slow healing
If you have a wound that seems to be difficult to heal, then it could be a sign of another chronic condition, such as diabetes. If you have diabetes, you will want to check your feet daily, check your shoes for sharp objects daily before putting them on and perform appropriate foot care.
Preventing wounds and infections in your extremities should be a high priority for you. Amputation carries with it a five-year death rate, and a much-decreased quality of life. You will want to protect your limbs from diabetic ulcers and treat any cuts or scrapes that you have. You will want to keep an eye on them, and consult your doctor if they don’t appear to be healing, or if they show any of the following signs and symptoms of infection:
- Redness
- Swelling
- Fever over 101 degrees (F)
- Drainage from the wound that is excessive, has an unusual color or a foul odor
- Increased pain at or around the wound site (pain can radiate to other places, ex: toe pain can radiate up the lower leg)
- The skin around the wound feels warm or hot
- Feeling tired or worn out 1
When should I contact my doctor?
Notify your doctor when you have a sore or wound that seems stubborn to heal. With wounds on your extremities (feet, legs, hands, arms), it’s a good idea to have the doctor evaluate it even before infection sets in if you have diabetes. If you have a podiatrist or foot specialist, they would be a good provider to evaluate any foot issues.
The reason for quick consultation of any wounds when you have diabetes is to prevent amputation. Even a small blister can fester into an infected wound that progresses to gangrene and amputation.
Prevention and promoting long-term healing
There are several things that you can do to prevent wounds that won’t heal if you have diabetes. If you have a wound, there are things that you can do to it, but if you have diabetes it’s best to see a doctor.
Keeping blood sugars and A1C in target range
Striving to keep blood sugars in a target range and A1C below 7% will help you to make sure that any blisters, cuts, scrapes or ulcers heal in the future. Practicing daily foot checks and foot care to identify any areas that may become a problem is important when you have diabetes.
People with diabetes have a 15% chance of developing a foot ulcer at some time during their chronic illness. It’s one of the most common problems to develop, and you won’t want it to lead to an amputation.
If you don’t have diabetes, keep in mind that a non-healing ulcer could be a sign of diabetes. Speak with your healthcare provider to have your wound checked and get any needed screening for diabetes or other issues that might delay wound healing. 2
Eating healthy
To heal, your body needs nutrients, including vitamins and minerals that you get from a healthy diet. You will also need protein in your diet to heal properly.
You should be eating from all food groups, including eating healthy carbohydrates in the right amounts based on what your health care provider or diabetes educator has told you. Vitamin C is also an important vitamin for wound healing.
If you are having difficulty getting your blood sugars and A1C in your target ranges, see a Certified Diabetes Educator or a Registered Dietician to help you get on track.
Check your wound
Check on it. Look for the signs and symptoms of infection listed above, and report these to your healthcare provider. Be aware if you have diabetic neuropathy that you may not feel increased pain. Make sure that your shoes fit properly and check them for foreign objects.
I once had a patient whose grandson dropped a set of keys in his boots. He walked on them all day and didn’t feel the injury that was occurring to his foot throughout the day. Once he got home, his wife noticed his wound. He had a nasty ulcer by then, and it took a long time for it to heal.
Keep pressure off your wound
To help your wound heal, you will want to make sure that no undue pressure is placed on it that would compromise its healing.
Keep your wound elevated to heart level
As much as possible, especially with wounds on the extremities, you will need to elevate it to heart level. If it’s on your foot, lay down as much as possible with your foot up on pillows. This will aid in circulation and help it to heal better.
If possible, get plenty of exercises
With wounds on your feet or legs, it may not be possible to exercise enough to get your heart rate up for what would be considered “aerobic” exercise. If you are unable to exercise, do chair exercises or range of motion exercises to increase your blood circulation. Exercise keeps your blood flowing, and you want as much circulation to get to the wound as is possible for your situation.
Don’t smoke or use nicotine containing products
Smoking or using nicotine-containing products displaces oxygen from your wound bed. Nicotine binds with receptors on body cells, keeping needed oxygen from binding with cell receptors. You need the oxygen to your wound more than you need the nicotine.
If you have diabetes, it is even more important to quit smoking or using tobacco products. It’s a double-whammy on your circulation to have diabetes and smoke. Call the quitline for your state and speak with your doctor about the best ways to become nicotine free. 3
Provide first aid to the wound daily
For a wound to heal properly, you need to keep it clean and dry to keep it from getting infected. Use wound dressings that are sterile. Cleanse the wound with warm water daily and apply antibiotic ointments if your doctor prescribes them. 4
Long-term risks of not treating wounds
The long-term risks of failing to treat diabetic ulcers or wounds that won’t heal for one reason or another is that the infection in the wound can travel into the bloodstream, causing sepsis and even death. When there is not enough oxygen in the wound bed for healing to occur, the wound bed becomes anaerobic.
This anaerobic environment leads to gangrene, which thrives in this environment. Once a limb is gangrenous, it must be amputated before it causes the person to become septic.
Are there any other causes of slow healing other than diabetes?
There are some other conditions that can cause slow wound healing. They are:
- Human Growth Hormone deficiencies
- Diseases of the vessels (vascular and arterial)
- Rheumatoid arthritis
- Deficiency of the mineral Zinc
- Stress
- Jaundice
- Taking corticosteroids
- Taking non-steroidal anti-inflammatory medications (ibuprofen, naproxen, aspirin)
Diabetic wounds in research
Research had demonstrated that people with diabetes take longer to heal following surgery and experience more complications of surgeries than the general population. The combined factors of age, being overweight or obese, malnourished or having problems with large or small vessel circulation can increase the likelihood that wounds will become infected. These factors can also keep the wound from healing properly.
As blood sugar and A1C values rise in the person with T2D, decreased insulin levels can decrease chances of a wound healing properly. In a facility, following surgical procedures, blood sugars must be kept in target ranges to promote healing from surgery. Rapid response to infection with antibiotics, strict management of diabetes and good nutrition can help post-operatively in the healing process. 5
In one study, the researchers noted that there were one hundred different factors that can contribute to a failure of wounds to heal in the person with diabetes. They have a lack of growth factor, decreased granulation tissue production for scab formation, decreased migration of cells needed to complete the immune response. People with diabetes were found to lack the intense migration of cells that would mitigate the immune response.
Therefore, debridement of wounds is necessary to bring healthy tissue to the surface and help enhance healing of the wound bed.
Further reading:
Over to you
Have you had a wound that was stubborn to heal due to diabetes or another factor or condition? Tell us the steps you took to get it to heal. We hope this article is helpful to you anytime you have a wound that is giving you trouble. Remember to see your doctor if you have diabetes. We would love to have your comments on this subject. Let us know your thoughts in the comments box below. Thanks for your support as usual!
TheDiabetesCouncil Article | Reviewed by Dr. Jerry Ramos MD on June 01, 2020