What is nerve damage from diabetes?
Diabetic neuropathies are nerve damage caused by diabetes. Neuropathy is one of the most common long term complications of diabetes. It can occur anywhere in the body, and in any organ.
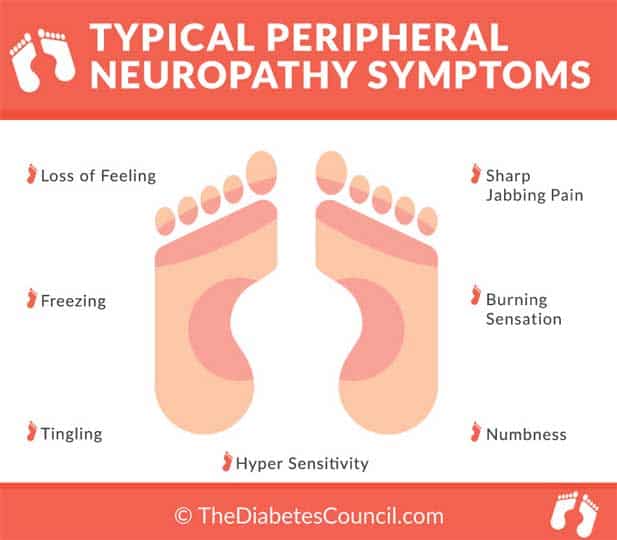
Symptoms such as numbness, tingling, and loss of protective sensation can be found in the hands, arms, fingers, feet, legs, toes, and lips. You may also have symptoms of nerve damage in the digestive system (gastroparesis), in the heart, or in sexual organs (erectile dysfunction, or vaginal dryness).
In this article, we will be mainly looking at peripheral neuropathy in the feet, also commonly known as sensitive feet.
Contents
What are sensitive feet?
Patients complain about numbness and tingling in their feet and toes, or elsewhere, with a frequency that is more often than in similar reports of other diabetes complications they experience. It’s no wonder these patients with diabetes have complaints of neuropathy symptoms.
Other than the tingling sensation or the numbness usually associated with neuropathy, those who have it complain about how much it hurts to put their socks and shoes on. The skin is sensitive to touch, to a point where one can’t even brush up against anything.
It is likened to an over-sensitivity and mild pain that is uncomfortable. If it goes on day in and day out, it can be frustrating. Sometimes, a person with diabetes may also get other related foot problems, such as plantar fasciitis. This condition affects the heel of the foot, and can be extremely painful. You will find it too sore to walk with plantar fasciitis. Even without heel problems, the generalized foot pain and soreness can become severe.
For more health related issues regarding diabetes read the following:
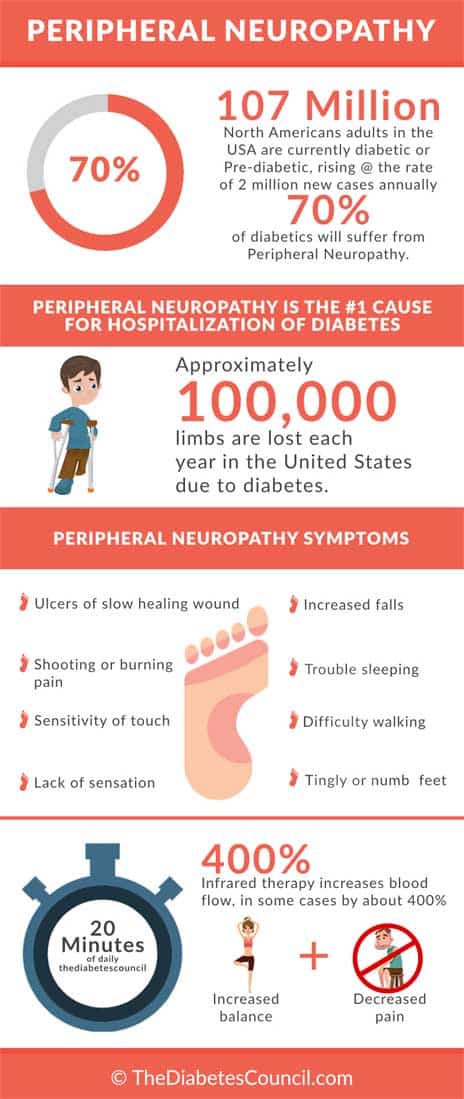
It has been found that as many as 60 to 70% of people with diabetes have neuropathy somewhere in their body. The longer you have diabetes, the more likely you will experience symptoms of neuropathy somewhere in your body. Your risk of neuropathies also increases with age. High rates of neuropathy occur in older people who have had diabetes for several decades.
Which people with diabetes have more neuropathies, and more sensitive feet?
- People who have difficulty managing their diabetes
- People who have high LDL, or “bad” cholesterol, and/or high triglycerides
- People with high blood pressure
- People who are overweight
What are the signs and symptoms of diabetic neuropathies in your feet?
Some nerve damage is so severe that there are not any noticeable symptoms. Most likely, if you do have neuropathies from diabetes, you have sensitive feet. Your feet may feel numb at times, get “pins and needles” feelings, feel unusually tired and achy, or cause you mild to severe pain.
Due to the likelihood that it may take a number of years before symptoms are severe enough for a patient to seek treatment, nerve damage may have become severe by the time a patient does seek help. Remember, while symptoms may not always be visible, be wary of feeling numb and weak in your feet.
What are the causes of feet sensitivity (diabetic neuropathy)?
The causes of foot sensitivity from diabetic neuropathies are all related to high blood glucose, in one way or another. Still, it’s a combination of many things that leads to neuropathies. Research is currently looking at how blood glucose plays a part, specifically, high blood glucose when it comes to neuropathy.
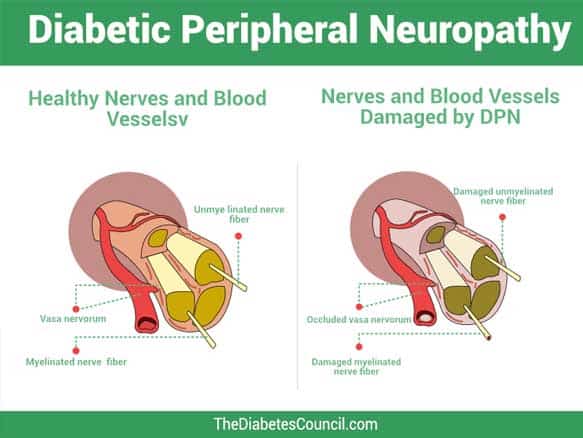
Neuropathies can happen anywhere in the human body. If you have had diabetes for decades, and have high “bad” blood cholesterol numbers, your chances of having neuropathies will be high. Other factors that are the root causes of neuropathies include low insulin levels, damaged veins and arteries that feed the nerves, and inflammation in nerve pathways.
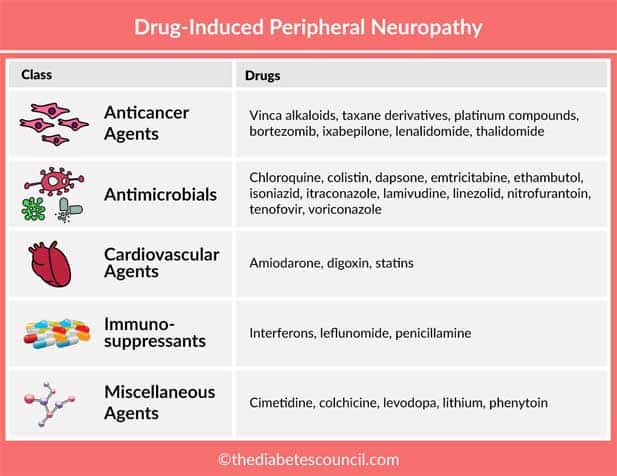
An injury to nerves in the wrist area can also cause neuropathy. Inherited nerve diseases, smoking, and alcohol use can also play a part in the development of neuropathies. All of these things, combined with decades of Type 2 Diabetes, high blood pressure, high LDL or “bad” cholesterol, lead to an increased incidence of neuropathies in the diabetic population.
Are there different types of diabetic neuropathies?
There are four different types of neuropathies:
- peripheral neuropathies (affects arms, hands, fingers/ legs, feet, toes)
- proximal neuropathies (affects thighs, buttocks, hips)
- autonomic neuropathies (nerves that innervate the regulation of blood pressure, blood glucose, digestion, respiration, urination, and other body functions)
- focal neuropathies (head, core, legs- sudden not gradual)
The type of neuropathy that causes sensitive feet is peripheral neuropathy. It is helpful to understand what kinds of neuropathy there are, because neuropathies don’t affect just the arm, hands, fingers, or just the legs, feet, toes of people with diabetes. People with diabetes can get the other types of neuropathy as well.
For the purposes of our article, we will focus on peripheral neuropathy.
What is peripheral diabetic neuropathy?
Peripheral neuropathy is neuropathy that affects the periphery - or in other words, your arms, hands, and fingers, or your legs, feet, and toes. Other names for peripheral neuropathy are distal symmetric neuropathy or sensorimotor neuropathy. There is numbness and pain associated with peripheral neuropathy.
Peripheral Neuropathy is the type of neuropathy that is most often found in people with diabetes. They will feel pain and numbness in their feet and legs before they start seeing the same symptoms in their hands or arms.
You may find that you have decreased sensation to pain. Perhaps you have burned your skin in bath water because the water was too hot but you failed to realize it before it was too late. It may be that you step on a tack and walk around on it for a few days before you notice it. You don’t feel the same pain which you would have otherwise felt due to a loss of protective sensation.
You may start to notice the “pins and needles” feelings in your feet and toes. Often these symptoms can be worse at night. You could be getting night cramps, or sharp pains in your legs, feet, or toes. There can be a marked loss of balance, as your feet can’t feel when they are touching the ground as well as they used to.
Muscle weakness develops, with loss of ankle reflexes. This loss of reflexes combined with muscle weakness can change the way you walk. If you aren’t walking correctly, then you become more at risk for collapse of the arch, or other ankle and foot deformities, such as hammertoe.
It’s likely that you may not notice a blister or sore that develops due to loss of feeling from this nerve damage. The nerves that tell your brain what your feet are up to are damaged. When infections occur in these situations (remember people with neuropathy are more likely to have uncontrolled diabetes), the likelihood of amputation increases.
Diabetic neuropathy and amputation
Amputation shortens your life about five years. Amputation can often be avoided with prompt attention to problems, daily foot checks and foot care, and of course good self-management of diabetes. Maintaining A1C of less than 7 percent, and blood glucose in a target range will go a long way to prevent neuropathies that lead to amputation.
People with diabetes and neuropathy pain often complain of pain upon even light touch to their feet and legs. This can make even putting the covers over their feet at night an uncomfortable situation. A sensitive foot situation can interrupt sleep, exercise, and quality of life.
Let’s take a look at a few case studies in sensitive feet.
John’s story
John came to me for diabetes education in his eighteenth year following the diagnosis of his diabetes. He had never taken any classes to learn about diabetes in depth. He was willing to set some great goals to get started, including learning to count his carbohydrates, and giving up his cola. He was a very humble and honest man, and he told me the truth.
“I’m not going to exercise,” he said. “I’ll just go ahead and tell you that right off the bat.”
“Why is it that you are not going to exercise?” I asked.
“My feet hurt,” John said. “I can hardly walk on them long. They hurt so much that I almost fall. It hurts to touch them, and at night, I toss and turn trying to get comfortable. That’s why I can’t exercise,” said John.
We were able to get John’s diabetic peripheral neuropathy diagnosed by his physician, and he started Neurontin. Learning to manage his diabetes, and bring his A1C from 9 percent to 6.8 percent, helped lessen the nerve pain. As advised, John began to keep a pattern management notebook. This way, he was able to keep his blood sugars in his target range at all times of the day, improving the overall management of his diabetes.
Although John still has some pain in his feet and legs, he doesn’t have severe problems related to his diabetic neuropathy any longer. He takes care of his feet, performing daily foot checks and foot care, and visiting his doctor every three months. He has managed to keep the pain in his feet and legs from returning to the severity that he once experienced. By better managing his diabetes, he has successfully prevented severe neuropathy pain.
What’s more, John started an exercise program. He joined the Silver Sneakers, and then a walking group. He has lessened his depression, improved his diabetes and related ailments, and has made new friends. He combines aerobic exercise with strength training, and gets about 200 minutes of physical activity a week. He argues that he has never felt better.
Mary’s story
Mary was constantly rubbing alcohol on her legs. Her legs were dry and scaly from all the alcohol rubbing. “My legs just ache all the time,” she said. Mary had an A1C of 10.6. She was having severe high blood sugars, but also some low blood sugars. On top of that, her blood pressure was high and her bad cholesterol was elevated at 130.
With Type 2 Diabetes for the last 20 years, she admittedly ate the same way she always has. She didn’t really check her blood sugars, and she skipped her insulin from time to time. She didn’t like needles. She knew of the complications that she could run into having had a grandmother who lost both legs to diabetes, and ended up on dialysis.
She said that she preferred not to think about her diabetes. It made her sad to think about it. Still, the symptoms that she experienced from day to day made it hard for her to forget that she had diabetes. She experienced a fair amount of fatigue. She didn’t feel like doing much. She was hungry often, so she ate.
She gained weight, and became more inactive. Her legs began to feel very heavy. She had a few falls, one of which landed her at the emergency room because of a bumped head. Every set back that Mary experienced just caused her symptoms to get worse.
We started working with her diet first. She had a daughter who came to class with her. The daughter did her cooking, and organized her meal planning. She lived next door. Mary was able to get more control over her diabetes by first working on her diet. She began to walk a little, just about 10-15 minutes a day, three days per week.
She then added in a few days of classes at the senior center. As Mary began to have better control of her diabetes, she came to a shocking revelation: she no longer had pain in her feet!
Mary didn’t even need to start on any oral medications for her neuropathy, or raise her insulin dose in order to get better control over her diabetes. She improved her diet and added exercise components to her lifesytle. In this way, she was greatly able to reduce her pain from neuropathy to the point where she didn’t even have an issue with it anymore.
She occasionally gets pains in her legs, but nothing like in the past, and she has stopped rubbing alcohol on her legs. She now uses alcohol-free lotion instead, and the skin on her legs is smooth and soft.
What do John and Mary’s stories tell us?
John and Mary both made progress, and were able to have less pain with sensitive feet. You can learn about how other people handle their diabetes by joining a diabetes support group, or an online diabetes community.
Always take the advice of your doctor over any individual, as they have more medical expertise. If you go online, be safe, and do not share your personal information!
Why do my feet hurt?
If you have Type 2 Diabetes, and your feet hurt, you are not alone. Many people with diabetes suffer from the pain of peripheral neuropathy. As it turns out, the high blood sugars over time damage the blood vessels. We then see that the vascular system is also interrelated with the nervous system. Imagine that you have tiny bits of plastic floating around in your blood stream, the effect is similar.
The tiny pieces of hard plastic beat up against the sides of your blood vessels and damage them. It’s not real plastic, but bits of bad fat floating in there. It hardens, much like the bad cholesterol from animal fats in our blood steam. People with diabetes have dyslipidemia, so they are more prone to have this bad fat floating around in the blood stream.
Once the blood vessels have some damaged areas inside them, that’s when you start to feel extra sensitive in your feet. The feet are innervated by the longest nerves that extend from our brain to our toes. This is why people with diabetes feel the pain of peripheral neuropathy in their feet first.
Symptoms are often profound at night, and can alternate from numbness to mild to severe pain. When our feet are numb, our feet can’t tell our brain that something is wrong. Therein lies the main problem with diabetic peripheral neuropathy.
How do I prevent diabetic peripheral neuropathy?
In a few words – good diabetes management. More specifically, through keeping your A1C below 7 percent, keeping your blood sugars in a target range, maintaining a healthy diet and keeping an active lifestyle. Getting the recommended amount of physical activity, and regular, daily foot care, also plays a factor in preventing diabetic peripheral neuropathy. Exercising helps for the blood to circulate better to areas which need it. By doing these things, you can prevent neuropathy, or decrease the symptoms.
The first line of defense is to maintain those blood glucose levels in target range, and keep the A1C low. This protects blood vessels from damage. This has been proven through research time and again. Lower amputation rates today are the direct result of better diabetes management, better foot care, and prompt attention to foot problems.
With better attention and care towards their diabetes, people are living longer. That’s more reason to take care of your feet if you have diabetes.
Feet: hygiene and care
Foot care and hygiene is one of the most important things that a person with diabetes and sensitive feet from neuropathy should do. People with diabetic neuropathy need to take special care of their feet.
The loss of feeling in the feet that can occur with diabetic neuropathy could mean that you walk around all day with a sharp object in your shoe without even feeling it. If you are not doing your daily foot checks, you could miss a festering infection, a blister, or even a foreign object sticking in your foot, such as a thumb tack.
It’s a lot easier to prevent an infection in your feet and legs than it is to heal it when you have diabetes. To reduce the incidence of amputations by 45 to 85 percent, there must be daily foot checks and care. This cannot be stressed enough. Six in ten amputations occur in relation to diabetes, not trauma. That is a lot of amputations due to diabetes.
A word about smoking
Anything that affects your general circulation can cause you to have more foot problems. With combined neuropathy and diabetes, it’s best to manage those things that you can change. If you smoke, take steps to quit once and for all. It is a double insult to your circulation when you have diabetes, and you smoke. Smoking will increase any risks for foot problems or amputations. Call 1-800- QUIT-NOW for help to quit smoking.
How do I perform diabetic foot care?
- Use warm water and a mild soap daily to wash your feet
- Do not soak your feet in Epson salts, or other foot soaks
- Dry your feet, making sure to get in between the toes
- Check your feet daily for any problems such as calluses, corns, warts, swelling, broken skin, or redness
- Use a mirror to check the bottom of your feet if you can’t see them – a telescoping mirror works great (pick up from your pharmacy)
- Apply alcohol-free lotion daily, but not between your toes
- Toenails should be cut straight across, and file gently with an emery board
- Thickened toenails should be cut by a podiatrist (foot doctor)
- Any calluses, corns, or warts should be treated by a podiatrist
- Do not use any over-the-counter corn or wart removers (they contain acid)
- Do not perform “bathroom surgery” on yourself (such as digging out ingrown toenails)
- Wear diabetic socks
- Have your shoes fitted to your right size
- Wear new shoes and socks for an hour at a time to break them in
- Check your shoes for any sharp or foreign objects daily prior to putting them on
- If you have a pedicure, tell the nail tech that you have diabetes, and to be gentle
See a podiatrist
You need a podiatrist to get a baseline related to the condition of your feet, circulation or lack of, and look for the presence or absence of neuropathy.
After you have seen the podiatrist for a baseline visit, you can then have a check-up once a year. The podiatrist will check the pulses in your feet, and check for blood flow with a Doppler machine, and perform a comprehensive foot exam.
What is a comprehensive foot exam?
During a comprehensive foot exam, the podiatrist has you lie back on the exam table with your eyes closed. The doctor will ask you to tell them where they are touching you on the foot with a 10 mm monofilament. The monofilament looks like a short fishing line, attached to a piece of paper. This exam does not hurt at all.
Take care of foot ulcers, infections
Sores, infections, funguses, ingrown toenails can cause major problems if you are not careful. The sensitive feet problem from neuropathy that makes your feet harder to touch without discomfort can also hide problems. You may not feel if your shoes are too tight, and are rubbing against a blister.
Some of my patients have even walked around on a thumb tack for days without noticing it. When an infection sets in with uncontrolled diabetes, it’s hard to get a handle on it. That is why prevention is key.
Have the doctor check your feet
During each regular doctor visit, take off your shoes and socks, and be ready for the provider to look at your feet.
Check your feet daily
Performing daily foot checks will prevent problems from your sensitive feet in the long run. It allows you to look for symptoms and signs right away before it is too late.
Make sure your shoes fit, or get diabetic shoes
To get properly fitted, it is recommended to visit the store at the end of the day when your feet have swollen. Try the shoes on. Walk around the store, and check for any pinching or grabbing. Remember, you have sensitive feet, so it may be harder to feel if your shoes are tight.
People with diabetes can be fitted for special shoes for diabetes if they have a prescription, and their insurance covers them. Patients can also pay out of pocket for shoes if they are not covered by insurance. Diabetic shoes are specially fitted, and designed to provide the right support, cushion, and fit for diabetic feet.
Exercise – it increases blood flow
Don’t forget how much exercise can improve your circulation and decrease diabetic nerve pain and sensitive feet. It causes vasodilation, and widens blood vessels so that more blood can circulate.
What kinds of treatments are there for sensitive feet?
Taking your medications on time and as prescribed
The first treatment is self-management. Once you have your A1C and blood glucose on target, then you want to recheck your symptoms. Do your feet still feel sensitive now that your diabetes is better managed? If not, you may want to continue with the healthy diet, exercise, and diabetes medications if needed to keep your feet feeling fine.
If your doctor has prescribed a medication for your sensitive feet, make sure that you take the medication on time. Try not to miss any doses. Medications used for diabetic neuropathy that are common are Lyrica, gabapentin, or Neurontin. *Please note that gabapentin and Neurontin are the same drugs. Lyrica is pregabalin.
These are oral medication and can come from several classes of medications, including:
- Antidepressants – ex: Elavil (Amitriptyline)
- Anticonvulsants- ex: gabapentin, Lamictal (Lamotrigine)
- Opioids-like medications – ex: Ultram/tramadol
If you still are having sensitive feet that are interfering with your quality of life after you have brought your A1C and blood sugars into your target range, it’s time to have a talk with your doctor about starting on one of these medications. There is no reason for you to suffer when you could get some relief.
Antidepressants may work for neuropathy. Even if you are not depressed, the medication works on improving nerve pathways. It is not really recommended to purchase over-the-counter medications such as ibuprofen (Advil, Motrin), or acetaminophen (Tylenol). These medications don’t work very well for neuropathy pain.
Creams
There are some creams that may help with neuropathy pain. Ask your doctor or pharmacist before using any over-the-counter products for your sensitive feet. You can use the patches for your feet, or sprays for your sensitive feet. Some natural oils can also help foot discomfort.
The pharmacist may have recommendations about the products that may work for you. Don’t forget to also consult with your healthcare provider about the available creams.
Other treatments
When feet are sensitive to a point that you can’t stand the touch of the sheets on the top of your toes, there are a few alternative treatments that you could try using:
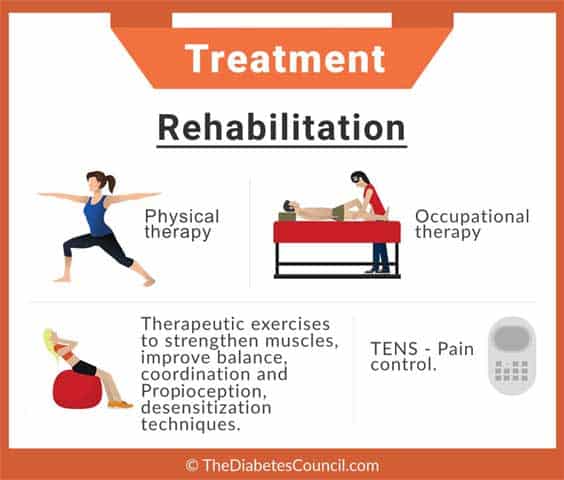
- Physical therapy
- Acupuncture
- Biofeedback
- Electrical nerve stimulation
- Magnetic therapy
- Laser therapy
- Light therapy
Physical therapy and exercise are sure to help. The other methods listed have been known to help some people’s pain from their sensitive feet. Some need to be further evaluated for effectiveness for use with diabetic neuropathy and sensitive feet.
However, if your doctor feels that it’s ok for you to try the treatment, you may try them. None of the treatments listed above would cause you harm, but it’s always a good idea to speak with a healthcare professional before starting on any new treatments.
Additional reading material:
Over to you
I hope that we have been able to answer your questions about sensitive feet. If you have any comments, or need something clarified, please let us know in the comment section below and share the article with those who need it.. We would also like to hear from our readers who have or have had neuropathy to share tips or about medications that helped them with their symptoms.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on June 01, 2020
References
- https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-problems/nerve-damage-diabetic-neuropathies
- https://www.diabetesdaily.com/forum/neuropathy/43428-skin-sensitivity-peripheral-neuropathy/
- http://www.diabetes.org/living-with-diabetes/complications/neuropathy/peripheral-neuropathy
- https://www.health.harvard.edu/blog/diabetic-neuropathy%E2%80%94the-agony-of-da-feet-201111143797