You may take rapid acting or fast acting insulin (also known as insulin analogues) for your diabetes, either through injections prior to your meals, or in your insulin pump. You may use it alone, or in combination with other insulins and diabetes medications, including injections and pills.
In a person without diabetes, the pancreas puts out small amounts of insulin, continuously bringing down blood sugars to a normal level with no difficulty. When a person has diabetes, they may not make any insulin, as occurs in Type 1 Diabetes. They may make some insulin, but it’s not working well, and it’s just not enough to bring blood sugars into a normal range, as occurs in Type 2 Diabetes.
When there is no insulin, or not enough insulin, the goal is to try to simulate what the body normally does to bring down blood sugars through injections of insulin, inhaled insulin, or via an insulin pump. To do this, rapid or fast acting insulin must be taken in relation to food that is eaten in many cases. Not everyone with diabetes must take insulin to control their blood sugars, though.
Let’s learn how Christie uses rapid acting insulin…
Contents
Christie’s story

Christie has had Type 1 Diabetes for 24 years. She uses a Medtronic insulin pump. Every day, Christie’s pump gives her fast or rapid acting insulin. This is all that insulin pumps need to control blood sugar.
For Christie, she uses Humalog lispro insulin. She gets a little bit of this rapid or fast acting insulin continually through her pump via a basal. She also gets some of this insulin through her pump, in a bolus dose every time she eats a meal. In a pump, the same insulin is used all the time, and it is always rapid insulin.
Christie also has a new Continuous Glucose Monitor, CGM. She has found with this new technology, she must check her blood sugars earlier than when she is ready to eat.
With the CGM, she found that if her blood sugar was 120 mg/dL or less, she had to wait about 15 minutes or so. If her blood sugar was over 120 mg/dL, she had to wait about 30 minutes before giving her bolus does of rapid insulin. At any rate, Christie now has her post-meal blood sugars fine-tuned with her Rapid insulin in a bolus dose.
Christie is testimony that insulin reacts differently in different people. While some people need to take their rapid insulin 15 minutes before a meal, others seem to need to wait longer, even taking bolus doses of insulin after eating.
What is rapid or fast-acting insulin?
Rapid-acting, or fast-acting insulin is insulin that is generally taken before or after you eat a meal. When your pancreas doesn’t produce enough insulin, you may have post-meal blood sugar spikes that keep you from good management of your diabetes.
When you take rapid or fast-acting insulin, you bring down the blood sugar after a meal. This way, your graphs on your meter don’t look like a roller coaster, and you have a nice straight line without spikes in your blood sugar across your meter graph.
That’s nice to see, and a great A1C level, and a nice-looking blood sugar log, should coincide with that. That’s when you know you are winning the diabetes game. Rapid or fast acting insulin can help you do just that.
People with Type 1 and Type 2 Diabetes can take rapid insulin. People with Type 1 Diabetes may take a longer acting insulin for their basal dose in an injection to keep their blood sugars in line between their meals and while they sleep. This helps to better control blood sugar, also.
Those with Type 2 Diabetes may take rapid and long acting insulins, and they may also take oral diabetes medications as well. Diabetes is complicated, and sometimes it takes several different medications to control it, along with healthy eating habits and an activity plan.
Those that use an insulin pump to control their diabetes, like Christie, shouldn’t mix their rapid insulin with anything else. Your insulin pump is manufactured to take one kind and brand of insulin only. In addition to being delivered by insulin pumps, rapid insulins can be delivered by insulin pens, insulin vials and needles, and nasal inhalation devices (Afrezza).
I recommend reading the following articles:
What are the side effects of rapid insulin?
Though there are many side effects of rapid or fast acting insulin, the main one is obvious when you know a little bit about insulin.
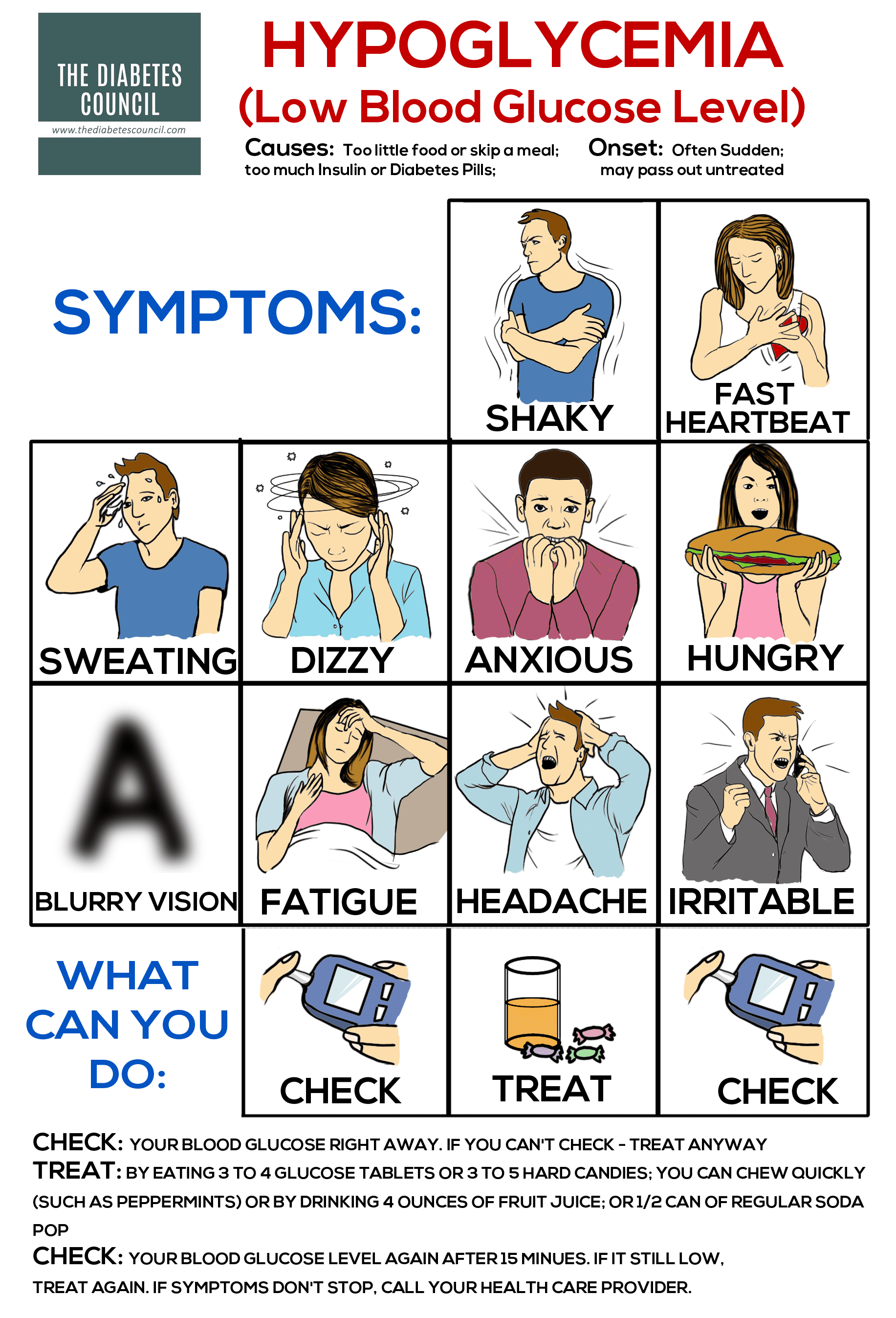
Hypoglycemia, or low blood sugar
The most common side effect of rapid acting insulins by far is low blood sugar, or hypoglycemia. With rapid insulin, blood sugars drop quickly, so low blood sugar could be life threatening, and include unconsciousness, seizure, or even death. To avoid a low blood sugar while taking rapid insulin, you should always check your blood sugars as frequently as your healthcare provider advises you to.
Make sure to talk with your provider if you experience any episodes of low blood sugar while you are taking rapid insulin. Low blood sugar is the most dangerous acute complication of diabetes, and even one or two low blood sugars is not safe, and increases your risk of death. You should always strive to prevent low blood sugars while taking blood sugar lowering medications, such as rapid insulins.
Other side effects of rapid insulin:
Anaphylaxis has been reported, with other side effects of rapid insulin, which are basically signs of a low blood sugar, signs of local site of injection reactions, signs of an allergic reaction, or signs of anaphylactic shock, and they include:
- Anxiety
- Feeling “drunk”
- Blurred vision
- Sweating
- Confusion/ impaired thinking
- Seizures
- Increased depression
- Dizziness
- Sleepiness
- Hunger
- Fast heartbeat (tachycardia)
- Irritability
- Headache
- Unusual behaviors
- Increase in nightmares
- Restlessness during sleep
- Shaky
- Speech that is slurred
- Tingling of hands, lips, tongue, feet
- Dimpled injection site
- Dry mouth
- Weak, thready pulse
- Injection site infection (pressure, itching, redness, soreness, swelling, tingling, stinging feelings at injection site)
- Thirst
- Feeling of skipped heart-beat, or irregular heart rate (arrhythmias)
- Anorexia, or loss of appetite
- Moodiness
- Mental changes
- Muscle cramps
- Muscle pain
- Nausea
- Vomiting
- Stomach pain
- Itching
- Rash
- Hives
- Thickened skin at injection sites (lipodystrophy)
- Difficulty breathing
- wheezing
- Tiredness, weakness, fatigue
- Low blood pressure (hypotension)
- Weight gain
- Chest pain
- Peripheral edema
- Worsening of diabetic retinopathy at the beginning of drug therapy (reversible ophthalmologic refraction disorder)
- Worsening of diabetic neuropathy at the beginning of drug therapy (transitory, reversible acute painful peripheral neuropathy
- Urinary Tract Infection (UTI)1
Rapid (fast) vs short acting, intermediate acting, mixed, and long acting insulins
Rapid or fast acting insulins have an onset of anywhere from 10-30 minutes, as you can see in the chart below. They will peak at anywhere from 30 to 90 minutes, and they have a duration of about 1 to 5 hours, depending on whether it’s Lispro, Aspart, or Glulisine. The way that you can differentiate the types of insulin available are to look at the onset, peak, and the duration of the particular insulin.
| Rapid-Acting (Fast) Insulin | ||||
| Generic name,
(brand name) |
Onset | Peak | Duration | Indications |
| Lispro (Humalog) | 15-30 min. | 30-90 min | 3-5 hours | Rapid-acting insulin covers insulin needs for meals eaten at the same time as the injection. This type of insulin is often used with longer-acting insulin. |
| Aspart (Novolog) | 10-20 min. | 40-50 min. | 3-5 hours | |
| Glulisine (Apidra) | 20-30 min. | 30-90 min. | 1-2 ½ hours | |
Onset is how long it takes for the insulin to get into your body, and first start to lower your blood sugar. The peak is how much time it takes for the insulin to reach maximum effects in your body, or when it is exerting its greatest effects. The duration of insulin refers to how long it continues to lower blood glucose before it is out of your system.
How does rapid acting insulin compare with short acting insulin?
Short acting insulin is also considered a mealtime insulin, but it doesn’t get in and out of your system quite as fast as rapid insulin does. It takes a little longer, so if you are taking short acting insulin, you will have to take it about 30 minutes before you eat a meal. It takes about 30 minutes to one hour before it gets going, and it will peak in about two to four hours. It stays in your system anywhere from five to eight hours.
Short acting insulin is not given with rapid acting insulin. The two are similar, so you wouldn’t mix them. The brand names for short acting insulins available on the market are Humulin R and Novolin R. Short acting insulins are also sometimes referred to as regular insulins. Since it lasts a little longer, it’s possible to get good blood sugar control with a shot at breakfast and a shot at supper, while skipping a shot at lunch.
How does rapid acting insulin compare with intermediate acting insulin?
Intermediate acting insulin is meant to cover your blood sugar between meals, and at nighttime. After injection of this insulin, you won’t see it working for another 2-4 hours. It’s usually taken in two split doses per day to cover a 24-hour period. Intermediate and rapid insulin can be given together to get better blood sugar control, and providing a basal/bolus dose needed.
Name brands are Humulin N (NPH), and Novolin N (NPH), and they can control blood sugars for up to 12 hours. They can be combined with rapid or short acting insulins for better control. They take a while to get in your system at one to four hours, and peak in your system between four and 12 hours. These insulins can be used for background, or basal insulin dose.
How does rapid acting insulin compare with long acting insulin?
Long acting insulin, like intermediate acting insulin, is also meant to cover blood sugars between meals and at night. It’s taken once daily, and it can be taken with rapid acting insulins to give the basal/bolus doses of insulin needed to control blood sugars.
The two main types used are Lantus (Glargine), and Levemir (Detemir). They start to work in about one hour, and they stay in your system for about 20 to 26 hours. Long acting insulins are basal or background insulins, and they don’t have a peak.
These insulins are meant to provide coverage over a full 24-hours. They are often taken at bedtime. Many people with Type 2 Diabetes take long acting insulin as their only insulin shot in a day, and along with their oral medications for Type 2 Diabetes, they can achieve excellent control.
How does rapid insulin compare with mixed insulins?
There are different mixes of insulins that are available on the market.
Some of the name brands are:
- Humulin 70/30
- Novolin 70/30
- Novolog 70/30
- Humalin 50/50
- Humalog mix 25/75
- Humalog mix 50/50
These mixes combine rapid or short acting insulin with intermediate acting insulins. They are taken twice daily, anywhere from 10 to 30 minutes before a meal. Depending on the mixture, they take affect within five minutes to one hour. Peaks vary also by mixture, and they last for anywhere from 10 to 16 hours before they are out of your system.2
How many types of rapid insulins are there?
There are three main types of rapid or fast acting insulin. They are listed in the chart above, and they are Lispro (Humalog), Aspart (Novolog), and Glulisine (Apidra). There are a few other versions of rapid acting insulin, which we will discuss.
Other versions of rapid acting insulin
There are several other types of rapid acting insulin that we should discuss here. They range from ultra-concentrated rapid insulin, to inhaled rapid insulin, to faster Aspart insulin.
Humulog U-200
One very concentrated fast acting insulin that is available is Humalog U-200. It has double the concentration of Humalog U-100. There are 200 units/mL instead of the usual 100 units/mL of insulin. It acts the same as rapid U-100 insulin. It is for people with diabetes who require more mealtime insulin than U-100 provides, and is a way to concentrate the dose, so that less units are given.
Humulin U-500
When a person with diabetes needs even more concentrated rapid acting insulin, there is Humulin U-500. Again, this insulin allows for larger doses to be given in a smaller amount of units to control post-meal blood sugar spikes.
Inhaled insulin (Afrezza)
One rapid acting insulin that has come on the market recently is inhaled insulin. This insulin, marketed under the name Afrezza, is approved for use in both Type 1 and Type 2 Diabetes. You get a quick peak with the drug, in about 15-20 minutes, and it’s out of your body within two to three hours.
People with Type 1 Diabetes must use it with another basal injected insulin in order to achieve good blood sugar control.
New version of faster insulin Aspart
You may have heard of a newer, even faster acting version of insulin Aspart. It has an even more rapid action than its sister, Novolog. In phase three clinical trials, the new insulin approved by the FDA, marketed under the name Fiasp, reduced A1C levels, improving post-meal blood sugars better than Novolog did. It is insulin Aspart, super-charged, and its recommended for Type 1 and Type 2 Diabetes.
The new Aspart combines a vitamin and amino acid that increases the rate of absorption sooner and more rapidly than regular insulin Aspart. The insulin was formulated to increase blood flow at the injection site, which helps it to perform faster. It only takes two minutes before the insulin gets into your system.
It’s so fast, that it can be taken a full 20 minutes following a meal. The other three types of rapid insulin take 10-20 minutes before they will start to work in your body to begin to lower blood sugar. The maximum blood sugar lowering ability is reached peak between one and three hours after the medication is injected, and lasts up to three to five hours before effects wear off.
The new insulin is a breakthrough for those who have trouble with spikes following meals, and who aren’t getting into their target range with regular insulin Aspart. As expected, the most common adverse event that was reported in clinical trials with the new Aspart insulin was low blood sugar. The rate and severity of low blood sugars remained about the same as regular Aspart, so that’s encouraging.
Some other common side effects that can occur when taking Fiasp insulin Aspart are:
- Stuffy nose
- Upper Respiratory Infection (URI)
- Back pain
- Headache
- Diarrhea
- Nausea
- Urinary Tract Infection (UTI)
Fiasp is encouraging for the prospect of better diabetes self-management because it more closely imitates the way the human body releases insulin when the pancreas is healthy. A healthy pancreas will keep a person’s blood sugar between 70 mg/dL and 140 mg/dL, regardless of what they eat, how much stress they are under, or other factors. If insulin needs rise, the pancreas just kicks in with more insulin production. It’s a well-oiled machine, the healthy working human pancreas.
That could set Fiasp up for being used in the new Bionic or Artificial Pancreas. The closer that it mimics what our own pancreas does, the more likely that it will be useful in the Artificial Pancreas realm.
It may be the only super fast insulin on the market now, but two other companies, are trying to develop similar insulins, one being Eli Lilly. There is also a French company, Adocia, that is in the end phases of clinical trials for a similar insulin.3,4,5,
Does age, gender, and other factors taken into consideration when rapid insulin is prescribed?
Children by weight, are given less rapid insulin through an insulin pump, or through injections, administered and supervised by parents until the child can assume their own diabetes management. An elderly person who lives alone, and is prone to falls, might not be a good candidate for rapid insulin. The risk of low blood sugar may be too great. Cost and insurance coverage must be weighed out, as insulin is expensive.
Can I take rapid insulin if I am pregnant?
All types of insulin are used during pregnancy to control blood sugar in the mother, and to help the fetus to grow. Insulin is the first drug of choice during pregnancy. It doesn’t get past the placenta, and so the fetus doesn’t get it. If blood sugars are not in good control for the mother, then excess glucose does get to the fetus, and can cause problems at birth, such as high birth weight and low blood sugars following birth, among others.
When you are pregnant and taking rapid insulin, you have to track your blood sugars frequently. Your insulin dosage will fluctuate during your pregnancy, so you need to keep in close contact with your high-risk pregnancy clinic to avoid the pregnancy complications that can occur with diabetes.
Treating and controlling your diabetes prior to becoming pregnant is important. Poor control can affect fertility level in both women and men.
What about breastfeeding? Is it safe with rapid insulin?
Yes, rapid insulin is safe to use while you are breastfeeding your baby. In research, mothers who were treated with insulin during their pregnancy had infants who had a decreased risk for developing Type 1 Diabetes. Insulin has a long history of use during pregnancy and breastfeeding. Other medications do not have such a history, so there is more risk with taking other diabetes medications during pregnancy.6
What are the best times to take rapid insulin?
Rapid insulin is best taken up to 15 minutes before meals, or up to 15 minutes after meals. Learning from people with diabetes who have years of experience with taking their insulin with relation to their food intake reveals that insulin is used uniquely by the human body. Whereas one person may reach peak action at one time, another person with diabetes may take longer to reach peak action.
Not only can insulin onset and action be different from person to person, different factors play into how our body metabolizes insulin. Interestingly, choice of injection site for rapid insulin doesn’t seem to make a difference, as it does with longer acting insulins.
Increased activity, stress, illness, thickness of skin at injection site, temperature, circulation, and many other factors can affect the utilization of insulin in the body. Smoking can slow absorption of insulin, and large doses are harder to metabolize than smaller doses of rapid insulin.
Peak time ranges are always given in averages, so some people will peak before others with relation to insulin action, and others will take longer. It could be that you don’t see your insulin peaking until about 45-90 minutes after you take it.
Knowing and understanding how your body reacts to insulin can affect when you decide to give your insulin with relation to meals. Some researchers believe the maximum effect of rapid insulin doesn’t occur until a full 2 hours after taking it in some people where insulin is not absorbed well.
When you first get started, it takes some practice to get your doses fine-tuned. Always keep your glucose handy, in case you make a mistake to avoid a low blood sugar. Work closely with your doctor and healthcare team to fine tune when you give your bolus with your meals.
Counting carbohydrates is important
Counting carbohydrates that are contained in your meals and snacks, so that you bolus enough insulin before or with your meal will make a difference. It’s better to correct a blood sugar before it gets high, than to try to shoot darts of insulin at it after it has already risen too high. This way you prevent high blood sugars, rather than react to them. As it turns out, once blood sugar gets high, it’s tough to bring it back down.
What about the glycemic index?
How quickly foods will raise blood sugar indicates their glycemic index. Due to some people being more resistant to insulin in the morning hours, you can use the glycemic index to help with diabetes at breakfast. Eat low glycemic index foods for breakfast, such as a serving of oatmeal and fruit, or protein-containing yogurt and fruit. You want your breakfast power-packed with high fiber and protein, and healthy fats.
These types of foods will help raise blood sugar slowly. If certain foods cause a spike in blood sugars following your meal, then you can adjust the portion size, or omit the food, or increase your bolus dose of rapid insulin to cover it. Speak with your doctor before dose changes.6
Where do you get rapid insulin? Is it available over-the-counter?
Your doctor will give you a prescription for your insulin. If it is a name brand insulin, such as Humalog, Novolog, or Apidra, it is not available over-the-counter. You will have to get it from your pharmacy. You need a prescription for your insurance to pay for it.
Over-the-counter rapid insulin is available in off-brands, such as the Walmart brand, ReliOn. These insulins get recommended for my patients with no insurance coverage, or who find themselves in emergency situations, where they are unable to get their regular brand of insulin. These are the older generation insulins in regular short-acting insulin, and there is an intermediate acting insulin that is given twice daily that is available.
The action is different for these older types of insulins, so they may not work quite like your name brand insulins, and they may require adjustments in dose. It’s important to note that rapid insulin is currently not available over the counter. Only it’s slightly longer-acting cousin, short-acting regular insulin, is available over-the-counter in the US.
Even though Walmart has $25 insulin vials, it will take a great deal of adjustment to switch to two injections per day for a basal dose, and regular, short-acting insulin at meals with a longer onset, peak, and duration. It can make diabetes tougher to manage, so before you think about swapping out your rapid for cheaper, short-acting insulin, please talk these things over with your healthcare provider first.7
How effective are they?
There is some debate related to the safety and effectiveness of rapid acting insulins. There have been studies to review and compare treatment with rapid versus regular insulins, and also with pre-mixed insulins for both Type 1 and Type 2 Diabetes. Data was gathered from 13 different studies, and analyzed the data for A1Cs in these patients.
The findings were that rapid insulin does result in lower A1Cs than taking regular, short acting insulin. Rapid insulin was preferable over short insulin for bringing down blood sugars post-meal than was regular, short acting insulin.
Safety studies showed that there was less nocturnal hypoglycemia at night with relation to taking rapid insulin, but there was a minor increase in the number of low blood sugar incidents when compared with short insulins. Rapid insulin also lowered post-meal blood sugar slightly more than short insulin. Researchers concluded that rapid insulin gave better control over diabetes versus short, regular insulin.
Further reading:
Things to consider when taking rapid insulin
The timing of your dose is important with relation to meals. You may not always be able to count carbohydrates, so there will be times when you really don’t know how much you are consuming. This could happen over the holidays, at a friend’s house for dinner, or when you are out to eat when no nutritional information is available.
In some cases, the food may dictate the insulin, and not the other way around. For example, if your blood sugar is high right before your meal, you can use your insulin sensitivity factor. This is the amount that your blood sugar will go down with one unit of insulin.
Calculate what your dose is for coverage of the high blood sugar. Wait until you start trending down, then eat your meal. This works well for most insulin pumpers.
For those folks with diabetes who inject insulin, even if you use vials, it could be helpful to have an insulin pen around, which is more portable than vials of insulin. If your blood sugar is between 140 mg/dL and 180 mg/dL pre-meal, then take rapid insulin, and wait 30 minutes before you eat. If it’s higher, say between 180 mg/dL to 200 mg/dL, then waiting 45 minutes before eating may be warranted. If greater than 200 mg/dL, waiting an entire hour before eating may be warranted.
In some cases, it can take up to two hours before blood sugars that were high pre-meal to start coming down to target range. You could limit your intake to protein, and non-starchy vegetables, but Christie found that she had to eat something. If she starved herself, then she couldn’t get her high blood sugars to come down. She did better with good carbohydrates from vegetables, and some protein, then her high blood sugars would start to come down.
If you can check your blood sugar about an hour before your meal, you can do a correction dose of insulin an hour before your meal if your blood sugar is too high. That was, you will be trending a lower blood sugar when it’s time to eat your meal.
Conversely, if your blood sugar is too low before you eat your meal, then you may need to delay taking your rapid insulin. The trick here is to give your food about 15 minutes to start raising your blood sugar before you take your rapid insulin. When eating low glycemic meals, you want to wait until you are about to start to eat to take your rapid insulin.
If you are not sure how many carbohydrates are contained in the meal you are about to eat, try splitting your dose of rapid insulin. Take half prior to eating, to cover the carbohydrates that you are thinking you will be eating. Then if it’s a very large and long meal with multiple courses, you can take more rapid insulin if you need to. This tip works great if you are an insulin pumper.
Pumpers can also use their pump’s functions for bolus delivery when they are eating larger meals over a longer period. You can use the function that allows you to give the bolus dose over a longer time. Current insulin pumps allow you to give some at the beginning, and then the rest over a couple of hours. One idea is to take half at the beginning, and the other half about one or two hours after eating.
Similarly, for larger meals that take longer to digest, and can cause a late rise in blood sugars hours after a meal, dividing the dose of rapid insulin can also be helpful.
Generally, for snack time, you want to take some rapid insulin with anything that is over about 10 grams of carbohydrates. This amount typically raises blood glucose about 30 mg/dL.
One caution is to never give rapid acting insulin less than four to five hours apart. This amounts to stacking of insulin, and it’s dangerous. Before the last dose of insulin gets out of your body, if you give yourself another one, you are that much more prone to a low blood sugar.
You can figure on using about 20% of your rapid insulin up per hour, and so you should try to figure out how much insulin is on board that has not yet been used. This is the amount of active rapid insulin in your system from previous injections or boluses from your pump. This insulin will continue to lower your blood sugar until it is completely out of your system. Always keep this in mind to avoid low blood sugars.
New insulin pumps have a great feature that keep you alerted of this issue, and lets you know if you still have insulin on board that could cause you a low blood sugar.
One tip is to check your blood sugars after meals, at one hour, two hours, and three hours past the meal to see when your blood sugar starts to come back down following a meal.
Writing down your blood sugar reaction to the carbohydrates you eat can be very helpful. By keeping a log, you will be able to look back over it, spot your trends, and make appropriate adjustments.8
Cost
Rapid insulin sales are big business for pharmaceutical companies, with Novolog third in line as a best-seller. Third place represents $3.3 billion in sales. Humalog didn’t do half bad globally, and came in as the fourth highest in global sales in 2005.
That said, one month of Apidra costs around $400 for the pre-filled insulin pens. Afrezza inhaled insulin is around $355 per month, and insulin Lispro comes in around a whopping $530 per month for the pre-filled cartridges. Novolog is anywhere from $420 to $550 for pre-filled pens.
FAQ
Is a rapid or fast-acting insulin harmful?
Fast acting insulin can certainly be harmful if you have a severe low blood sugar while taking it. If you accidentally inject too much, or you give yourself too much of rapid insulin via your insulin pump, then you could end up in the emergency room with a low blood sugar that is hard to bring back up.
Always carry quick-acting carbohydrates with you, glucose gel, or a glucagon pen if ordered with you when you are taking rapid acting insulin. The best thing for a low blood sugar is prevention, because even a few are dangerous.
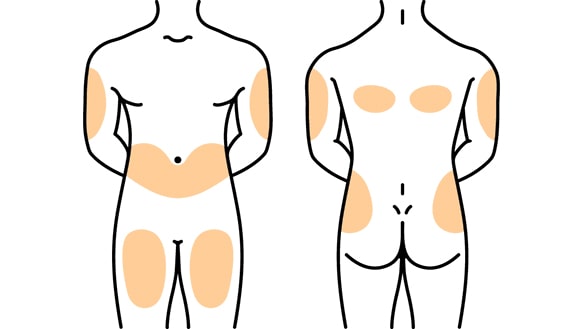
Are there specific injection sites for rapid (fast) insulin?
Rapid or fast acting insulin is given in the subcutaneous layer of fat. Subcutaneous means “just under the skin.” Rapid insulin injections are given in the same areas as are other insulin injections.
Rapid insulin can be given in the abdomen. You want to avoid about a two-inch section of skin around your belly button or navel. It can also be given in the top and on the outer part of the thighs. Here, you want to avoid boney prominences around the knee area. The outer and upper arms where there is some fat to pinch up is also a good area to administer rapid insulin injections. You want to rotate your sites, so that you don’t get lipodystrophy.
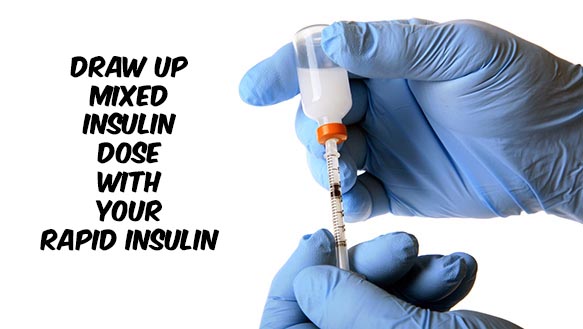
Is rapid insulin drawn up first from a vial for a mixed insulin dose?
When you are mixing insulins in a syringe, you want to draw up the rapid insulin (which is clear in color) up first, and then draw up the cloudy long-acting insulin after that. The following are the steps to drawing up a mixed insulin dose with rapid insulin:
- Roll the bottles of cloudy and clear insulins gently in your hands to mix them (don’t shake the insulin up, be gentle).
- Clean the top of the vial stoppers with alcohol.
- Get your syringe, and draw up the amount of the cloudy or long-acting insulin dose up in air, then inject the air into the cloudy insulin (to make room for drawing out the dose in the vial).
- Remove the needle, and draw the amount of the rapid insulin dose up in air, then push the needle into the stopper for the rapid insulin, and draw up the correct dose of rapid insulin.
- Next, draw up the dose of cloudy, long-acting insulin. You are now ready to administer your mixed insulin injection.
Can you take rapid and slow acting insulin at the same time?
Yes, many people take rapid acting insulin along with other types of insulin, including intermediate and long acting insulins. There are also mixed insulins available that contain rapid acting insulin and intermediate acting insulins in a certain percentage combination. You may have seen these as: Novolog 70/30 contains rapid insulin Aspart and a long acting insulin. Humulog 75/25 and 50/50 mixed insulins contain rapid acting and long acting insulins.
Does rapid insulin make you gain weight?
Unfortunately, insulin and weight gain go together. To keep from gaining weight while taking insulin, or to keep the amount of weight gain to a minimum, you should balance your activity with the foods that you eat, and follow a healthy diet. If you take enough insulin to cover the whole pound cake that you just ate, it’s safe to say, you will gain weight.
Keep special high fat, high sugar foods for special occasions, and stick to your plan most of the time to avoid the weight gain that can go along with taking insulin.9
Over to you
Increasing your understanding of rapid acting insulin can help you to get better control over your diabetes, by helping you to time your doses of rapid insulin correctly. What did you think about our article? We hope that you learned something from this comprehensive guide. Do you have any more tips to share with our readers? Your experience or comment may just help someone else who is in a similar situation.
TheDiabetesCouncil Article | Reviewed by Dr. Jerry Ramos MD on June 1, 2020
References:
- https://www.diabetesselfmanagement.com/managing-diabetes/treatment-approaches/fast-acting-insulin/
- http://www.diabetes.co.uk/insulin/rapid-acting-insulin.html
- https://www.drugs.com/sfx/insulin-aspart-side-effects.html
- http://www.health.com/health/gallery/0,,20402402,00.html#long-acting-insulin
- https://asweetlife.org/new-fast-acting-insulin-fiasp-against-krispy-kreme/
- https://asweetlife.org/eli-lillys-new-ultra-rapid-insulin-in-the-works/
- https://www.diabetesdaily.com/blog/a-newer-faster-acting-insulin-faster-than-novolog-280989/
- http://www.joslin.harvard.edu/info/insulin_a_to_z_a_guide_on_different_types_of_insulin.html
- https://www.babymed.com/medications/insulin-during-pregnancy-and-breastfeeding
- https://www.diabetesselfmanagement.com/managing-diabetes/treatment-approaches/fast-acting-insulin/
- https://www.ncbi.nlm.nih.gov/pubmed/21333580