No one likes to go to the hospital! I know, because I see patients hospitalized due to complications related only to their diabetes nearly every day. The vast majority of these hospitalizations could have been avoided with the proper training and prevention strategies beforehand. That is the good news. The great news is I am going to share all of these prevention techniques with you!
Following simple guidelines, you can stay out of the hospital as a result of your diabetes. Now I cannot promise you something else could crop up that may land you in the hospital…I am no miracle worker! However, I can teach you the Survival Skills for prevention and early treatment for the different types of diabetes emergencies.
In a series of two articles, we will be discussing the diabetes emergencies that affect people with both Type 1 Diabetes and Type 2 Diabetes. Since the emergencies affecting ladies who are pregnant with diabetes are so highly specialized, that is another article all in of itself! Feel free to check out Gestational Diabetes FAQ for answers to many of your questions related to gestational diabetes.
If you are now pregnant and have preexisting Type 1, Type 2 Diabetes or have Gestational Diabetes, please consult your Obstetrician for your guidelines very early in your pregnancy. They will normally refer you to an endocrinologist and a Certified Diabetes Educator to help you maintain very good blood glucose control throughout your entire pregnancy. Obstetricians recommend getting your blood glucose under good control even before conceiving for proper early development of the baby.
In this article, I will focus primarily on Hypoglycemia (also called Low Blood Glucose), but let’s also review some important points for everyone that has diabetes.
Contents
Safety Tips
Medical Id’s
I’m going to start out this article by letting you know the importance of having some sort of Medical Identification which will make rescuers and healthcare professionals aware of your diabetes in the event of an emergency. A necklace or bracelet is preferable because this is what they will see first. If you are in a car accident, there will not be time for them to search through your wallet…your wallet may be thrown 50 feet away I hate to say.
Unfortunately, the symptoms of many of the emergencies for people with diabetes mimic those of people on drugs or intoxicated with alcohol. If the first responders see your Medical ID, they will know to check your blood glucose immediately.
If you are having a low blood sugar, they will also know to treat it immediately.
I recommend reading the following articles:
Medication List
Keeping a current medication list with you at all times is very also very important. If you are in an accident or taken to a hospital and are unable to communicate with the physicians, they need to know exactly what medications you are taking, the exact doses and the times of day you take them. This is essential information for us to know when you are brought into the hospital so that we can keep you on these medications (if possible) while you are in the hospital. It also lets us know when you may have last taken those medications if you are unable to communicate that to us.
You can keep a medication list on your cell phone or a written list in your purse or wallet. We absolutely love to see when a patient pulls out a medication list! If we know exactly what medications the patient is taking, at what dose and at what time, it is much easier for us to solve the puzzle of what caused the emergency that led to a hospitalization.
Medical Supply Kit
Always having diabetes supplies on hand both at home and with you is so important. You can avert a diabetes emergency just by having your supplies! This sounds so simple, but it’s a tried and true fact my friends. My friend Elisabeth from TheDiabetesCouncil shares all her tips about which diabetes supplies to carry with you and when in this great article.
Hypoglycemia (Low Blood Glucose)
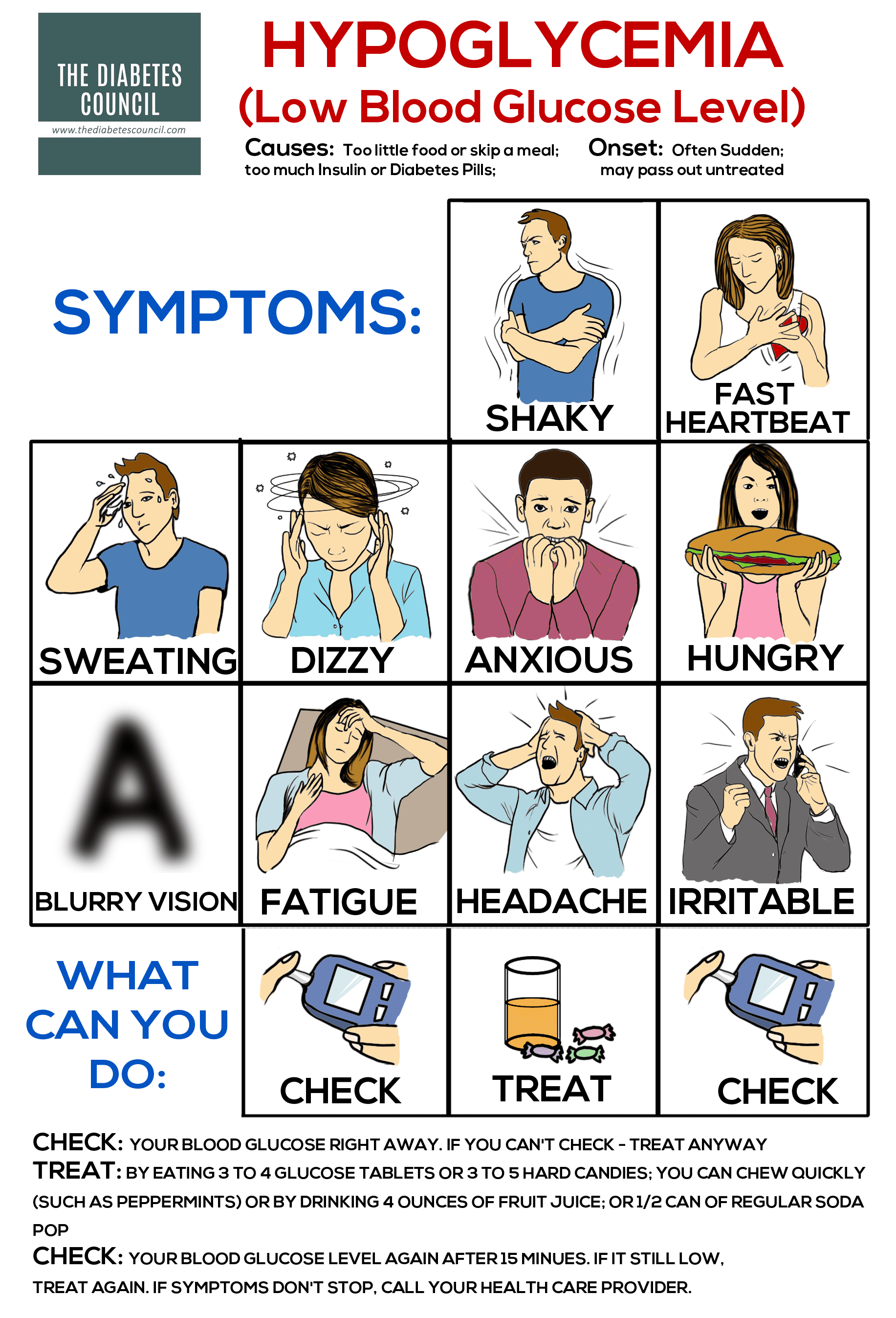
The first emergency related to diabetes we will be discussing is Hypoglycemia, also referred to as Low Blood Glucose. Hypoglycemia occurs when your blood sugar drops below 70 mg/dL.
Other conditions can cause hypoglycemia, but we will be focusing on prevention and treatment of hypoglycemia for people with diabetes for the purposes of this article.
As a RN, Certified Diabetes Educator, this is one of the most important skills we teach our patients to keep them safe. If you are taking any medications that lower your blood sugar such as insulin or even pills like glipizide, this can be a life threatening emergency so learning this skill is essential.
The Rule of 15
The treatment for hypoglycemia is called the Rule of 15; you need to consume 15 fast acting carbohydrates, then recheck your blood glucose in 15 minutes.
This seems very simple, but most people are not treating their low blood sugars correctly. I meet with patients everyday who are still treating their low blood sugars with food, so you are not alone! Let’s start at the beginning but reviewing the symptoms.
Symptoms of Hypoglycemia
- Shaking
- Sweating
- Hunger
- Dizziness
- Headache
- Fast heartbeat
- Blurred vision
- Mood changes, irritability, anger
- Seizures
- Unconsciousness
Symptoms occur quickly and can be very different with each episode. The symptoms of hypoglycemia are caused by the release of the hormone epinephrine (also known as adrenaline) which sends a signal to the liver to release more sugar quickly. That burst of adrenaline is what causes the symptoms of your low blood sugar.
So, have you ever been had a really close call, being cut off by a car in heavy traffic? Remember that feeling of shaking that you got right after? That’s a little burst of adrenaline…essentially the same feeling you will get early on with hypoglycemia.
70 mg/dL is the level that requires treatment, however, if you start experiencing symptoms at a higher level, you can give yourself a treatment to stop the symptoms. There are a couple of reasons you could be experiencing symptoms of hypoglycemia when your blood glucose is actually higher.
If your blood glucose is dropping rapidly, especially if you take insulin, this can cause the symptoms of a low blood glucose. Another instance is when your blood glucose has been high or uncontrolled for a period of time. Your body becomes accustomed to being “high” or uncontrolled, so when you go to your physician for your A1c check and find it is elevated, they make adjustments to your medications. Now your blood glucose levels begin to normalize, but your body has to readjust to feeling normal again. It will take a little time for this to happen, maybe a week or so.
I’ve had patients tell me, “Oh, I feel horrible if my blood sugars are below 150!” This makes me cringe because they just have never received the education as to what is going on in their bodies and why. If you feel low, check your blood sugar. If your meter says 150mg/dL, you can still treat the symptoms to make them stop without having to recheck. Now on to the treatment.
Treatment for Hypoglycemia
Rule of 15
Step 1: Always Check your Blood Glucose with your Meter First
Step 2: Treat Your Blood Low Blood Glucose if Below 70 mg/dL
You want to treat your low blood sugar with 15 carbohydrates of a rapid acting carbohydrate. Foods with fat will take much too long to raise your blood glucose, but a rapid acting carb will raise your blood sugar in 15 minutes flat! Here are some options:
- ½ cup (4 ounces) fruit juice orange, grape, apple, etc…just not diet!
- ½ cup (4 ounces) Regular soda
- 4 round glucose tablets (or 3 square ones)
- 1 tablespoon honey, sugar, jelly or syrup (not sugar free)
- ½ pack of Skittles or 15 jelly beans
- 1 cup of skim milk (the fat in other milk would slow down the treatment)
There are many fast acting carbohydrate choices, but always choose one that is fat free and is not food, like a candy bar.
*If you wear an insulin pump, remember to either disconnect from it or put your pump in stop mode immediately after you check that first blood sugar. Once your blood glucose has returned to normal, you can either resume your basal rate or reconnect to your insulin pump*
Step 3: Recheck Your Blood Glucose in 15 Minutes
If it hasn’t returned to normal (80-100 mg/dL), Repeat: Treat It Again, Wait 15 minutes and Recheck in 15 minutes Again.
Step 4: Once your blood glucose is above 80-100 mg/dL, eat at least 15 carbohydrates of food to keep it from dropping again until your next meal. These fast treatments will raise your blood glucose about 30-50 points in 15 minutes, but they will only last about 20-30 minutes. Carbs with fat and protein, such as ½ peanut butter sandwich, ½ tuna fish or chicken salad sandwich, or some cheese and fruit will keep your blood sugar stable until your next meal.
*If your blood glucose isn’t returning to normal and/or you think you have taken too much insulin or medication, call 911 immediately.
*If at any time, you or someone you know becomes unconscious, Call 911 immediately.
Glucagon
Glucagon is a hormone injection you can be given to raise your blood glucose fast if you have become unconscious. It does require a prescription and a family member or friend should be trained to use it. It is very simple to use; it comes in a kit with a prefilled syringe with sterile water and a vial. Since it does have to be mixed and injected, have your physician, Certified Diabetes Educator or Pharmacist teach your caretakers how to mix and administer it. Anyone who takes insulin should have a glucagon kit on hand in case of an emergency. Children should have a back-up glucagon kit kept at their school, for overnight stays or when they go away to camp.
I also suggest reading these articles:
Safety Concerns
Always check your blood glucose before you drive, especially if you take any medication that lowers your blood sugar. This could be insulin or pills. People do not see the danger in getting behind the wheel of a car and driving without knowing what their blood glucose level is. It is very serious and dangerous…you will be taking your life and in fact, the lives of everyone on the road in your hands.
Causes of Hypoglycemia and Prevention of Hypoglycemia
There can be many causes for hypoglycemia; here are some of the most common:
- Skipping meals or timing of meals
- Increase in activity, exercise, even a delayed effect of exercise
- Too much or timing of medication
Timing of Meals and Snacks
A very early symptom of hypoglycemia is actually hunger! It’s our body’s way of alerting us that it’s time for food! Our body is so smart; sometimes we just aren’t listening. A good rule of thumb is to not go longer than four to five hours without eating something, especially if you are taking medications that lower your blood sugar.
If your meals are more than 5 hours apart, you may need a snack between meals. So, if you like to sleep in (like I do) and eat breakfast later like at 8 or 9, then lunch is at noon, you may not need a snack between those meals. But then if dinner is at 6 or 7pm, you will definitely need a snack sometime during the afternoon.
Pay attention to your body; it will give you cues and alert you when you should eat. We all start getting hungry around 3pm…you know what I’m talking about, don’t you? It’s our body’s way of letting us know it’s time for a snack. If you eat a snack with carbohydrates, healthy fat and protein, the protein and healthy fat will fill you up but also act to tide you over better and stabilize your blood glucose until your next meal. Our body is a very smart and intricate life form…the most complex ever. Our brain is sending us signals all the time, we just don’t take the time to listen.
Also, if you eat dinner fairly early, then go to bed 4 to 5 hours later, you may need a bedtime snack. Remember, you will be fasting until you wake the next morning, so you could be at risk of an overnight episode of hypoglycemia.
Overnight lows due to prolonged fasting states do occur much more frequently than people realize. Yes, we have all woken up in the middle of the night in a cold sweat, but have you ever wondered if this is due to a low blood glucose? Unfortunately, most people do not realize this occurs, and often wake up with a high blood sugar the next morning as a result! How does this happen you ask? When your blood sugar drops at 3am, your liver should respond by releasing just enough sugar to keep your blood sugar stable…but unfortunately, in diabetes, this does not happen. It may release too much, causing a high blood sugar when you awaken. It is called rebound hyperglycemia or the Somogyi effect.
If you eat a bedtime snack, the hope is, you will prevent the overnight low blood glucose, so the liver does not need to respond at all, thereby preventing the early morning high blood glucose also. We call this a consistent carbohydrate diet because you are getting consistent amounts of carbohydrates, at consistent times throughout your waking hours to keep your blood sugar stable. It is used to help you live more like someone who doesn’t have diabetes.
Effects of Exercise on Blood Glucose
There are so many factors to consider when discussing exercise and its benefits for people with diabetes! But (there’s always a but, right?)…there are also some very important precautions to be aware of when exercising. I will hit the highlights here and save all the rest for a future article, so send me your questions in the comments below!
So, in regard to benefits to your blood glucose-exercise uses up the blood glucose in our cells as energy, (just as our car uses gas to run on) so exercise lowers our blood sugar! The important thing to remember here is, because of this, you will need to check your blood sugar both before, and after exercising, especially if you take any medications that lower your blood sugar. You may need to eat a snack of carbohydrates, protein and fat prior to, or after exercise to ensure you don’t go too low during that time as well.
Moderate to intense exercise can have the opposite effect on your blood glucose, causing an initial high blood sugar, then a later drop in your blood glucose. This is why it’s especially important to monitor your blood glucose using your blood glucose meter before and after exercise.
Exercise can also have delayed effects or a lag effect on your blood glucose for many hours, depending on how much exercise you have participated in. If you have taken a 100 mile bike ride, your muscles will continue to pull glucose out of your blood stream for a very long time; 24 hours would not be out of the question. This type of exercise requires much more frequent and longer monitoring of your blood glucose.
Insulin Pumps
If you wear an insulin pump, speak with your endocrinologist, Certified Diabetes Educator or Pump Trainer regarding whether you can either remove your pump for a short period of time or set a Temporary Basal Rate decrease while you exercise. Typically, if you opt for the Temporary Basal Rate decrease, we advise you set it for one hour prior to when you start exercising.
Do I need a Continuous Glucose Monitor?
Continuous Glucose Monitors (CGMs) can be obtained for people with all types of diabetes. You do not have to have an insulin pump to get a personal CGM. This device monitors your blood glucose 24 hours a day. If you are having a difficult time managing your blood sugars, discuss this option with your physician. You can also talk to your doctor about wearing a 3 day diagnostic CGM to determine blood glucose patterns and trends to see if you need a change in your medications.
One additional note about CGMs…if you already have one and have a low blood sugar, always confirm with a check on your blood glucose meter. I know we tell you this when we train you on your CGM, but just a reminder.
Adjustment or Timing of Medications
If your New Years’ resolution of diet and/or exercise is paying off, remember, you may need an adjustment to your medications! Whenever you lose weight, your insulin and/or oral medication requirement will likely need to be reduced. If you have more than two blood sugars under 70mg/dL in a week, contact your physician because they will want to make an adjustment with your medications. If you have a profound episode of hypoglycemia which would be categorized as under 50mg/dL, contact your physician right away because this will require an immediate adjustment to your medications.
Timing of medications is crucial; if you are taking medications that lower your blood glucose, you ALWAYS need to check your blood sugar before taking that medication. No excuses…I have heard them all too, the one I’ve heard the most is, “I don’t need to check, I can tell what my blood sugar is by how I feel.” I will address that in a moment, but, believe me, that is the biggest myth of all. If that were actually true, that would be the most profound medical breakthrough of all time.
The reason we tell you to always check your blood sugar before taking any drug that will lower your blood sugar is very simple…you could die very quickly from a low blood sugar if you do not.
The biggest risks of profound episodes of hypoglycemia are seizures, unconsciousness, and death. Sadly, people still are dying every day from low blood sugars everywhere in the world. I know this might be a review of information for a lot of you, but if one thing in this article saves one person through prevention, then it has certainly done its job.
Hypoglycemic Unawareness
The last condition I’ll discuss related to hypoglycemia is called Hypoglycemic Unawareness; it is a very serious complication. It is most likely caused when a person’s blood glucose goes low too often; their body starts to become less aware of the symptoms…leading to an autonomic failure. In other words, they will lose all awareness of symptoms. Their first and only symptom is a seizure or unconsciousness and their blood glucose is likely in the 20-30mg/dL (or even lower) range by then.
Anything we can do to prevent Hypoglycemic Unawareness is vital, because once this has occurred for a period of time, it is irreversible. The prevention for Hypoglycemic Unawareness is to prevent low blood sugars, period. As I said before, if you experience more than two blood glucose levels under 70mg/dL in a week, contact your physician for a medication adjustment. If you get one blood glucose level under 50mg/dL, contact your physician for a medication adjustment. Prevention is the key here because once this condition has occurred, it is very difficult to help manage. If you already have Hypoglycemic Unawareness, you absolutely need a continuous glucose monitor to alert you of low blood glucose levels.
Further reading:
- The Most Common Health Concerns For The Elderly And Seniors And How To Prevent Them
- Continuous Glucose Monitoring: Everything You Need to Know
- What is Rapid or Fast-Acting Insulin?
- Don't Take It Personal for What I Said When I was Low
- Medtronic Continuous Glucose Monitoring with the Elite Sensor Review
To Review…
- Get a Medical Alert Bracelet or Necklace
- Keep a current medication list with you at all times
- Carry your meter and some form of rapid acting carbohydrate with you at all times
- Know the Rule of 15
- Always check your blood sugar with a meter, do not rely on how you “feel”
- Always check your blood sugar before driving
- Eat a bedtime snack (if there are 4 hours between dinner and bedtime)
- Check your blood sugar before and after exercise
- Check with you physician regarding a 3 day diagnostic CGM or getting a personal CGM
- Speak up at your appointments!
Don’t be afraid to speak up at your appointments with your healthcare providers if you don’t believe your medication regimen is working correctly for you. Be honest with your physician if you’re not taking your medications as prescribed because of financial concerns, side effects, low blood sugars or even the fear of hypoglycemia. We need to make diabetes work around YOUR life, period. That’s what this is all about, making YOU healthy, happy and keeping you out of the hospital, right?
Like I tell my patients…they call diabetes education “diabetes self-management education” for a reason. Diabetes is a self-managed condition. Unfortunately, we cannot come home and help you manage your diabetes for you 24 hours a day, 7 days a week. That responsibility does fall on you, but we can provide you with the tools and teach you everything you need to know in order to do that.
With that said, if you haven’t been through a formal diabetes self-management program yet taught by Certified Diabetes Educators, I encourage you to do this. The information you will receive will be invaluable towards helping you manage your diabetes on a day-to-day basis.
Feel free to leave your comments about what tips and treatments work for your Hypoglycemia below and stay safe!
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on May 21, 2020
References
- https://www.thediabetescouncil.com/diabetes-supplies-take-leave-house/
- https://my.clevelandclinic.org/health/articles/11443-blood-sugar-what-causes-high-blood-sugar-levels-in-the-morning
- http://www.joslin.org/info/why_is_my_blood_glucose_sometimes_low_after_physical_activity.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499525/