Monika contacted TheDiabetesCouncil requesting information about diabetes management for patients who are in palliative care. Monika’s husband is in Memory Care for Alzheimer’s disease, and the staff was only checking his blood sugars two times per week for his Type 2 diabetes. They were not giving him his metformin anymore either, and they had started him on once daily injections of long acting insulin.
Monika wasn’t sure if the steps taken by the staff to manage his diabetes were enough. His blood sugars were going up to 200 mg/dl, and sometimes even higher. She did state that he wasn’t having any low blood sugars. This was comforting to her because he gets more confused when his blood sugar goes low.
They were also giving him desserts, and other unhealthy things, like fried chicken, on his tray. Was this ok, she asked?
We decided to look into this for Monika. We found that the guidelines are less stringent in palliative care, and it was not so important to avoid long term complications for her husband.
However, if Monika is uncomfortable with the palliative care, she should speak with the palliative care team at her husband’s Memory Care facility. They will usually work with the family to provide care that is more in line with what the family would want for the patient in palliative care.
We hope this article on palliative care for those with severe illness, and those who are terminally ill, will help family members and patients alike. Now let’s take a closer look at what to expect in palliative care if you or your family member has diabetes.
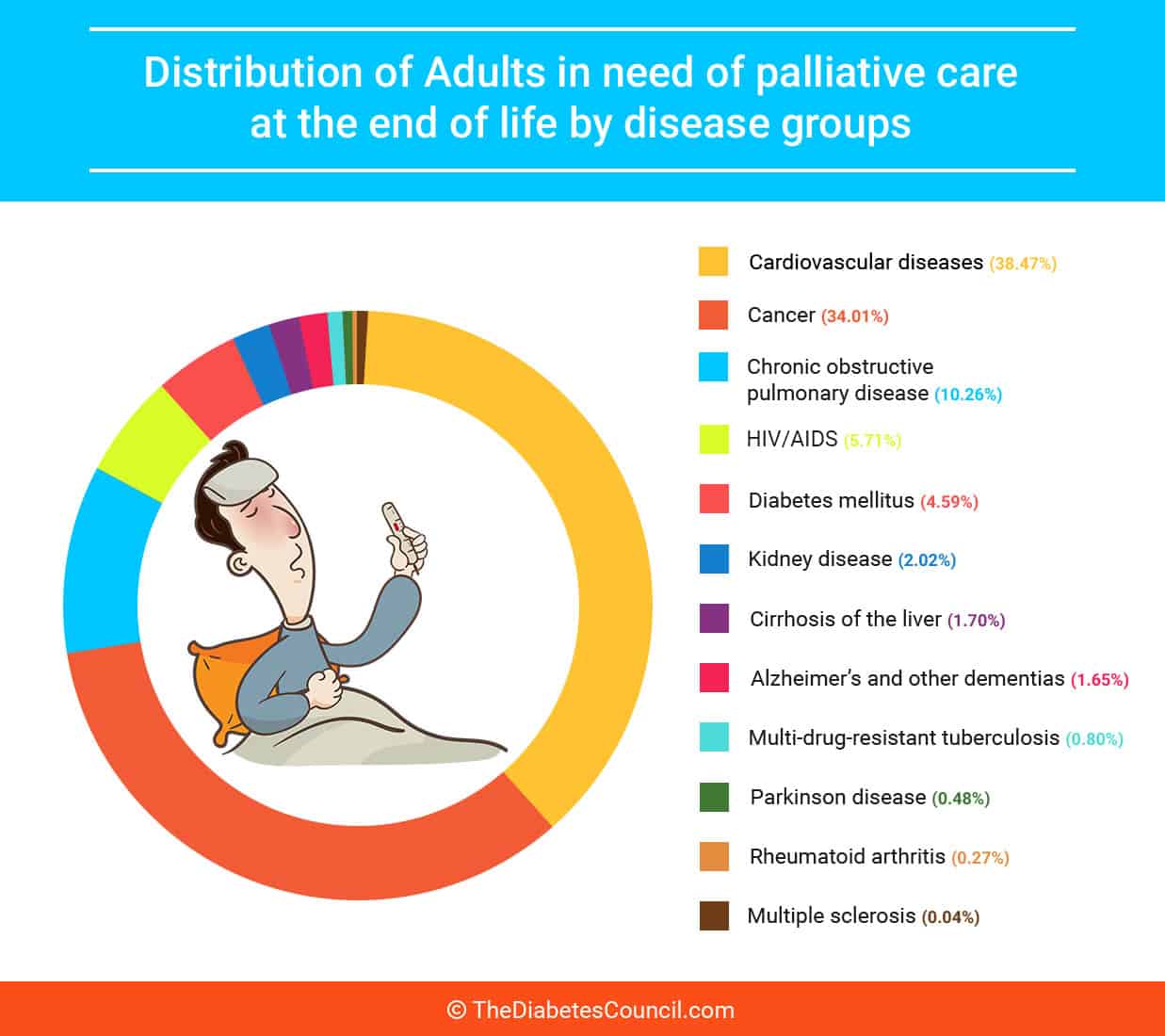
Distribution of Adults in need of palliative care
Contents
- The difference between palliative care and hospice
- Medically, physically, and ethically challenging care
- Factors that can cause low blood glucose
- Factors that can cause high blood glucose
- Management of diabetes during terminal illness
- Guidelines for terminal illness and end of life
- Research related to palliative care
- Over to you
The difference between palliative care and hospice
Unlike hospice, a person can receive palliative care at any age, and you do not need to be in the terminal phase of an illness. Another difference between palliative care and hospice care is that hospice is a Medicare covered benefit. It is for those with a terminal illness who have a specified number of months to live, according to their medical doctor.
If you are admitted to hospice, you have exhausted all other treatment options, and you along with your family have decided that comfort is of the utmost priority. Hospice may be administered in a facility, or inside one’s home. There is usually a team of hospice professionals, including social workers, nurses, clergy, and others.
Goal of palliative care
The goal of palliative care for patients with terminal illnesses is to improve the quality of life for the family unit, and to provide relief from symptoms related to end of life care for the patient. Diabetes care for the terminally ill has often been a subject surrounded by controversy, where few professionals agree on the level of specialized medical care that should be provided, and evidenced-based practices do not exist.
You can receive it if your chronic illness is causing you pain and stress, or other symptoms due to your illness. Palliative care can also be provided to patients with:
- cancer
- heart disease
- lung disease
- kidney failure
- AIDS
- Alzheimer’s disease
- amyotrophic lateral sclerosis (ALS)
- and multiple sclerosis (MS).
Palliative care team for symptom relief
Once you begin receiving palliative care, you are given a palliative care team of nurses, physical therapists, and social workers who work towards treating the “whole person.” Others involved may be massage therapists, nutritionists, and pharmacists. They are there to help provide you with relief from symptoms such as pain, shortness of breath, fatigue, nausea, constipation, difficulty sleeping and loss of appetite.
I advise reading the following articles:
You may receive a combination of medications, including pain medications, to relieve your symptoms. Massage and relaxation or meditation techniques may be used. The team follow a plan of care that they review often to make adjustments with you in mind. The palliative care team also works with your family to coordinate care and support them.
Does insurance cover palliative care?
Most insurance plans, including Medicare and Medicaid, do cover some portion of palliative care. If your healthcare provider refers you to palliative care, they can consult with you in relation to the insurance coverage, and other related out of pocket expenses.
Do I keep my primary doctor?
The palliative care team will work with your primary provider when coordinating your care. If you desire palliative care, you should discuss this with your primary care provider, and ask for a referral to palliative care that will best suit your needs. Your doctor can still order treatments and services that are curative in nature once you have entered palliative care.
Where is palliative care provided?
Many different palliative care options exist. Palliative care is available in hospitals, outpatient clinics, long-term-care facilities, or in a hospice. Many hospitals also offer outpatient palliative care in the home. 1
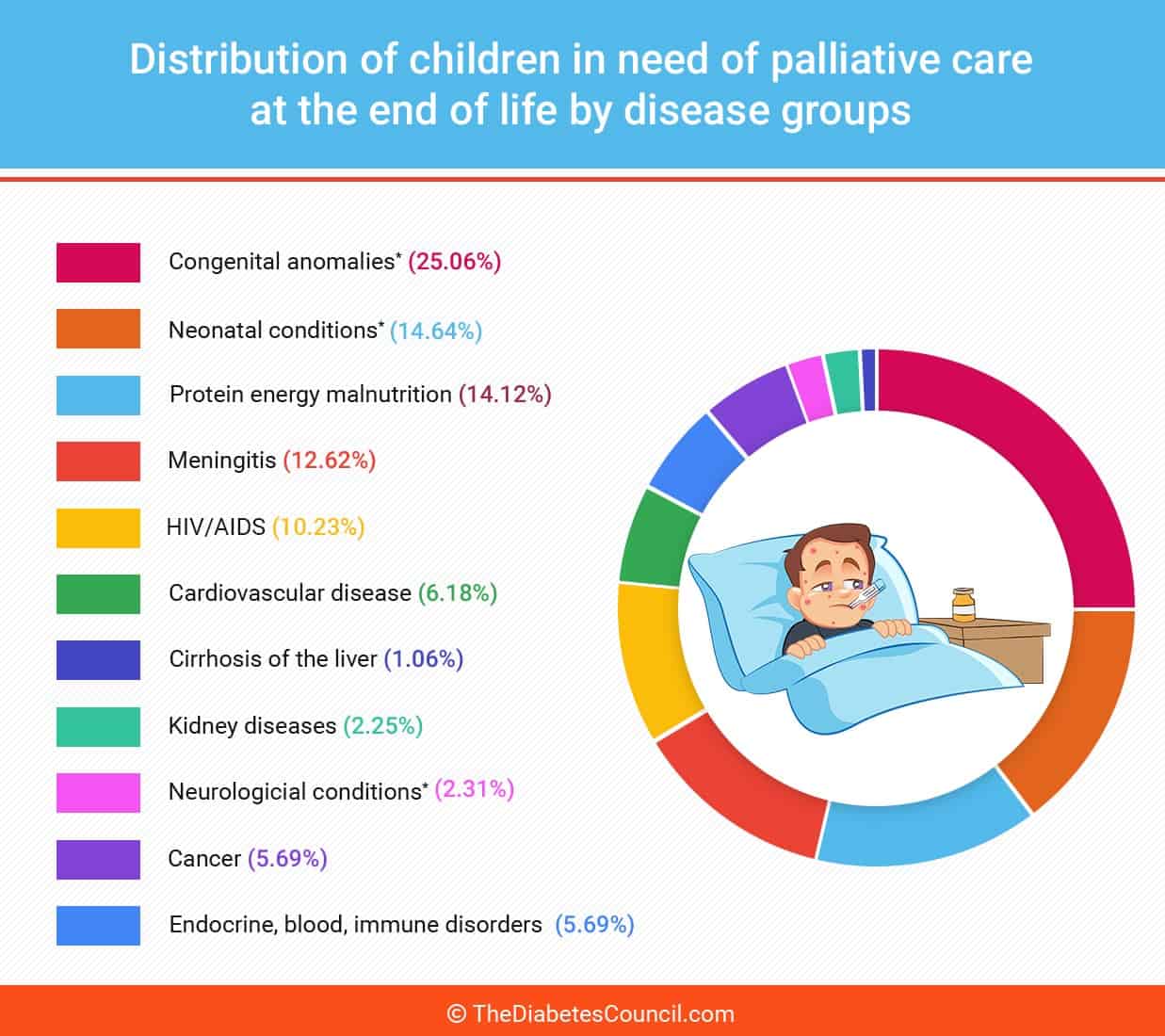
Distribution of Children in need of palliative care
Medically, physically, and ethically challenging care
Practitioners in a multidisciplinary team must look at patients with serious and often terminal illnesses medically, physically, and ethically. Issues that arise are complicated by malnutrition and cancer that spreads to the liver (liver metastasis).
Doctors and nurses alike disagree on the level of care that should be provided, how often blood glucose should be checked, and how often medication should be given. A push and pull exists between what patients and families desire, and what practitioners feel comfortable with in relation to palliative care.
Clearly, standards are more liberal when dealing with chronically and terminally ill patients. This poses problems ethically for the institution, and for the family, who understandably want the very best care for their loved one with diabetes.
In this article, we will discuss palliative care for patients with diabetes who have severe and often terminal illnesses. We will look at current practices and principles for the management of Type 1 and Type 2 patients who use insulin, and look at the use of medications in the elderly with diabetes who have severe and often terminal illness.
Factors that can cause low blood glucose
- Liver metastasis
Since many of the severely ill and terminally ill elderly patients that we speak of have a diagnosis of cancer, anorexia and subsequent weight loss, these present special challenges when caring for the elderly with cancer and diabetes. Metformin doesn’t normally cause hypoglycemia or low blood glucose, but in the elderly with liver metastasis, it can and does occur.
- Gastric malabsorption
The combination of oral hypoglycemic agents such as sulfonylureas and insulin with an alteration in gastric motility, and gastric malabsorption from large tumors, as well as decreased glycogen storage in the liver, which all add up to an increased risk of a low blood glucose.
- Tumor obstruction of bowels and opiate use
In addition, other factors that come into play when taking care of the elderly in palliative care are the presence of bowel obstruction from large tumors, and the use of opiates for pain relief. All these factors influence the metabolism of nutrients and medications for the elderly with diabetes in palliative care.
- Renal insufficiency
Terminal illness, including advanced cancer, is associated with renal insufficiency. Sulfonylureas and insulin have increased metabolism when the kidneys are not working properly. The patient with a severe or terminal illness is at increased risk of hypoglycemia also due to this decrease in kidney functioning.
Factors that can cause high blood glucose
- Steroid use
Corticosteroid use in the severely or terminally ill patients with diabetes is associated with high blood glucose. Steroids used to decrease symptoms of pain, decreased appetite, increased intracranial pressure or nausea with advanced malignant disease is associated with high blood glucose. It occurs in about 20 percent of the elderly who are using steroids in palliative care.
- Thiazide diuretic use
Thiazide diuretic use, such as the use of lasix or furosemide for fluid retention in congestive heart failure has also been associated with hyperglycemia.
Management of diabetes during terminal illness
Management during severe and terminal illness and palliative care for diabetes involves decreasing symptoms related to low and high blood glucose in the short term. Reducing macrovascular and microvascular complications over the long term is not as big of a concern as are the acute symptoms of hypoglycemia and hyperglycemia.
To check or not to check blood glucose – that is the question!
How often should a patient with diabetes and terminal illness in palliative care have their blood glucose monitored? This question has really not been answered by professionals, and answers range from once per day to once every three days.
One thing that the professionals do agree on is that if the patient is experiencing low or high blood glucose, they should receive more frequent blood sugar checks, at least until they get back in a safe range and remain there for a time period specified by their doctor.
Some professionals think that it is not necessary to do finger stick blood glucose on patients with Alzheimer’s, for example. They do not believe that the pain inflicted by it is worth it. However, other professionals feel that it is necessary, because a low or high blood glucose can have an effect on the patient’s mental status in this case.
ADM Position on Diabetes Management in LTC Facilities and SNFs
Patient and family wishes outweigh protocols sometimes
The patient and families’ wishes should weigh highly in the consideration of how often blood glucose levels should be checked. Still, it is controversial as to whether or not a patient with a severe or terminal illness in palliative care should have their blood sugars monitored up to and on the date of death.
As a palliative care patient becomes terminal, blood sugar checks may decrease in frequency, if not disappear altogether. However, much of this will depend on the families’ wishes.
Some families do not think that it is necessary, while others feel it would be neglectful not to monitor blood sugars. These families will express dissatisfaction with nurses and caregivers if monitoring of blood glucose is discontinued. The jury is still out as to whether or not it is necessary to monitor blood sugars when a patient is terminally ill, and near death.
Does management for Type 1 patients differ from management for Type 2 patients?
Type 1 diabetes patients are more difficult to manage when in palliative care because more frequent blood glucose monitoring is needed in order to manage the patient’s diabetes. They also require frequent insulin injections. Professionals do not agree on what the frequency of blood glucose testing should be, but they do agree that finger sticks should be kept to a minimum due to the patient’s comfort level.
For Type 2 diabetes patients, the current school of thought in absence of any real guidelines is that blood glucose monitoring should be discontinued during palliative care, especially during the later stages of a terminal illness. The family, however, may dictate what is to be done with respect to their loved one, and may request to continue regular blood glucose monitoring.
Guidelines for terminal illness and end of life
There are some pretty clear protocols that exist for managing patients with diabetes during the stages of a terminal illness. Still, all professionals in the field do not agree on the guidelines. Indeed, care for the terminally ill will likely always be surrounded with controversy, considering the emotional nature of the situation, and family members involved.
Algorithms seek to differentiate between those in the early stage of a terminal illness, and those in the late stages of terminal illness. Differentiation is made between patients with less than a month to live, for example, and those who may have six or more months to live.
Early phase of terminal illness
Relaxing the nutritional guidelines and dietary considerations in the early stages of terminal illness is considered permissible. This is considered acceptable practice for those with both Type 1 and Type 2 diabetes. Blood glucose monitoring can also be reduced to a minimum, although professionals disagree on what “a minimum” is, as well.
Sometimes patients with Type 1 diabetes are monitored two to three times per week, while those with Type 2 diabetes may only receive blood glucose monitoring one to two times per week. If the patient has episodes of low blood glucose, stops eating for a time, has nausea or vomiting, or is receiving a tube feeding, they will need more frequent monitoring. The same is true for the use of corticosteroids.
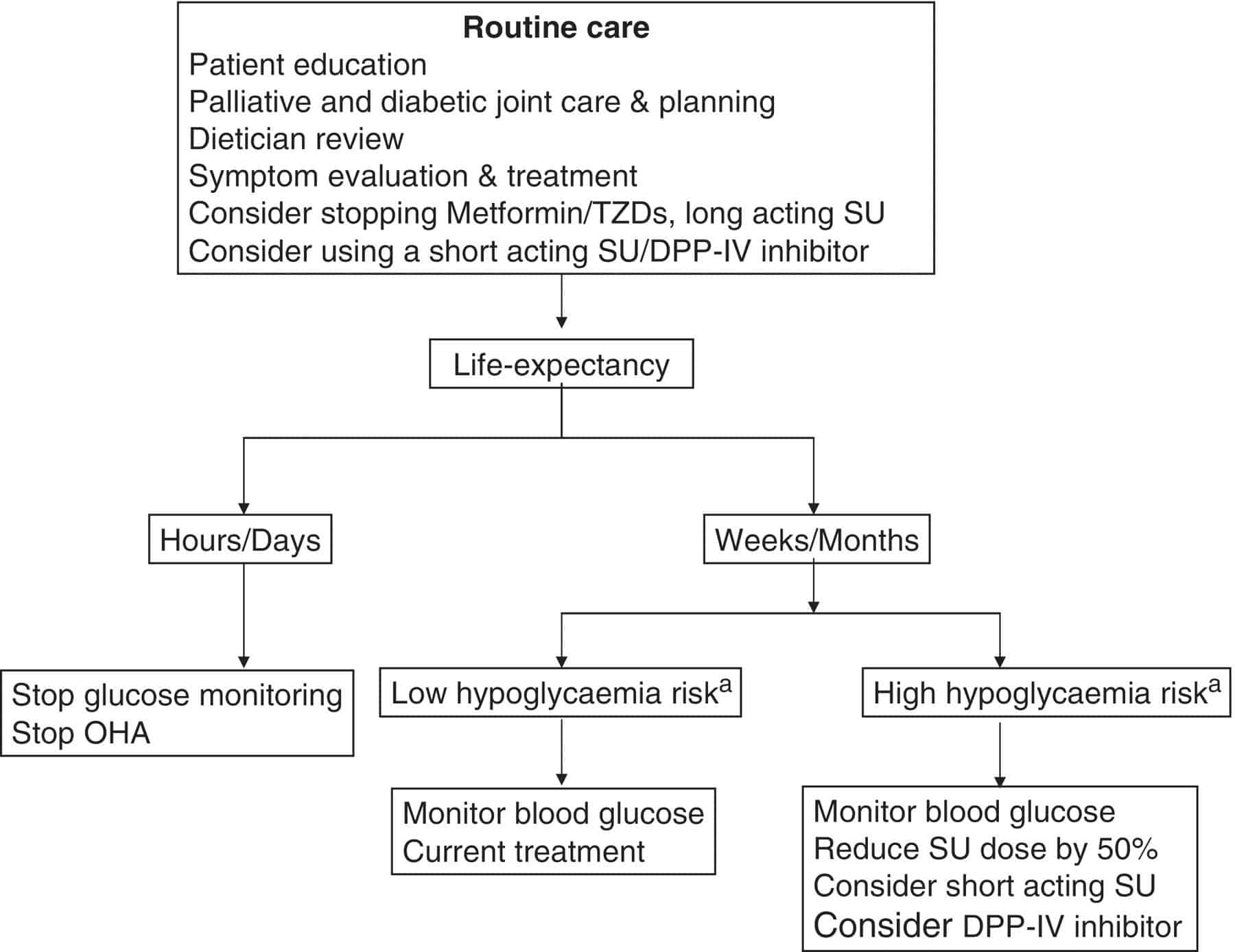
The following flow chart represents an example of a protocol for a Type 2 diabetes patient with a terminal illness:
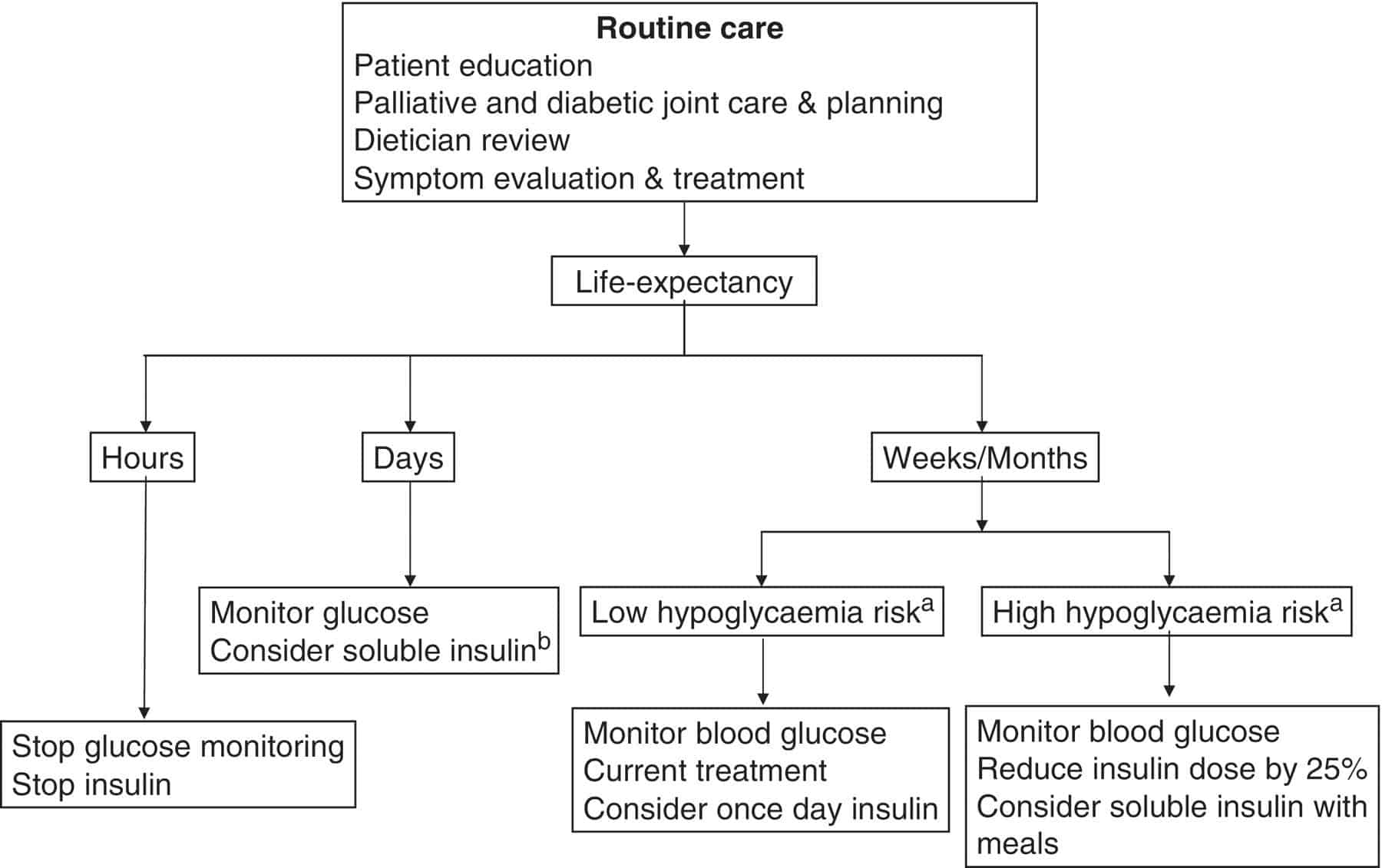
The following flow chart represents an example of a protocol for a Type 1 diabetes patient with a terminal illness:
These algorithms should be shared with patients and families, agreed upon, and then instituted. The care plan should be re-evaluated at regular intervals to ensure that the patient and family understand and agree to the treatment regimen during a terminal illness.2
In one research study done related to palliative care, patients with insulin requiring diabetes were given once daily blood glucose monitoring, and once daily injections of a long-acting basal insulin. The researchers concluded that dying with diabetes is not an easily managed clinical condition. Though we want to minimize discomfort and pain for the terminally ill patient, it’s important to decrease the acute symptoms that come along with low or high blood glucose.3
Special care is always taken to avoid low blood glucose due to safety reasons. However, high blood glucose is not considered as important to prevent, due to you are not worried about the long term complications of diabetes. It should be prevented when it affects a terminally ill patient’s level of thirst, including symptoms of dry mouth and dehydration.
In multiple research studies conducted across a wide variety of long term care populations, the prevalence of diabetes in palliative care comes out in between 25 and 34 percent. This has contributed to healthcare costs, with the palliative care costs of people with diabetes estimated at 19.6 billion in 2012.4
In one study in cancer patients, it was concluded that both low and high blood glucose excursions affect the quality of life for these dying patients. Wide blood sugar swings should therefore be avoided in these patients. Guidelines should be implemented to maintain glycemic control while minimizing interventions such as blood glucose monitoring and insulin injections.5
In the research there is not much that is said about targets for blood glucose in the palliative care realm. However, the guidelines are geared towards preventing the symptoms of high blood glucose, and avoiding low blood glucose.
Over to you
Let us know what you think about our article on palliative care for the severely ill and terminally ill patient with diabetes. If you have any experience related to having a family member with diabetes in palliative care, or have been in palliative care yourself, please share your experiences as well. We look forward to hearing from you.
References
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on May 24, 2020