It is widely believed that those with Type 2 diabetes may eventually need insulin if they have diabetes for long enough. However, only about 20-30 percent of people with Type 2 diabetes end up needing insulin injections. In this article, we will explore whether it is possible to manage your diabetes without insulin. If so, how can one do so and when they may eventually need insulin if other treatments do not work out? 1
Contents
Type 1 Diabetes disclaimer
This article is not for people with Type 1 diabetes because it is imperative that people with Type 1 diabetes require insulin every day without question. A person with Type 1 diabetes produces very little, or no insulin. Without insulin, you cannot convert food into usable energy. Simply put, without insulin, a person with Type 1 diabetes cannot survive. 2
When Robert contacted TheDiabetesCouncil, he was concerned that one day he would have to take insulin shots for his Type 2 diabetes. He had heard a few of his friends with diabetes at church talking about how they had to take insulin injections. Robert was “afraid of needles,” and the thought of giving himself a shot scared him.
Is Robert going to need to start taking insulin, or is there any way he can avoid it at this point? If he avoids it, what effects would this have on his health? Will he develop long term complications of diabetes if he doesn’t start giving himself shots of insulin?
I suggest also reading these:
At TheDiabetesCouncil, we decided to take a look at this particular question in depth, for Robert and for others with diabetes who might benefit from reading this information.
Insulin isn’t the “bad guy.”
Naturally, the fear of giving oneself an injection or “shot,” can increase anxiety and stress. But what if I told you that once you get past that initial fear of giving yourself an injection, insulin will help you manage your diabetes and live a longer, healthier life?
If your doctor tells you that you have to go on insulin injections, remember that there is a reason for it. Your doctor has your best interests in mind when he recommends insulin to you. Before getting to this point, you have probably already tried diet and exercise, several oral medications, and maybe even a GLP-1 weekly injection.
With time, your body has started making less and less of its own insulin, and as a result, more and more of your beta cells have died out. At this point, when the beta cells in the pancreas have stopped making insulin, it becomes inevitable that you need to take insulin injections to keep your A1C in a range that decreases the chances of future diabetes complications.
Not everyone will have to take insulin
This is the natural course of diabetes for 20—30 percent of people with Type 2 diabetes. 70-80 percent of folks with diabetes never have to take insulin injections. You may be one of those in the 20-30 percent group, or you may see a day when insulin is added to your diabetes regimen.
Is diet and exercise enough, or do I need metformin?

Metformin can lower A1C by 1-2 percent. It should be used in the treatment of Type 2 diabetes for this reason, along with its protective mechanism related to beta cells in the pancreas. Most people with diabetes will want to achieve an A1C of less than 7 percent in order to avoid the long term complications of diabetes.
Your healthcare provider will look at your A1C numbers, and determine the need for interventions, including diet, exercise, oral medications, non-insulin injectable medications for diabetes, or insulin. Generally, what happens is that a person with diabetes will do well on metformin for a number of years, and then they tend to start seeing their A1C creep up.
It becomes more difficult to keep the A1C below 7 percent with diet, exercise, and metformin. At this point, your healthcare provider may be looking at adding in a number of different oral medications for diabetes, or adding a GLP-1 injectable, and eventually insulin if A1C goal is not achieved by other means.
Generally, your healthcare providers will put you on a medication trail or treatment regimen for about three months. After that time, if you are still not getting desirable A1C results, then they may look at different trail medication. Eventually, you may get to insulin. On the other hand, it’s possible that you may never need it, and will do fine on other medications for diabetes.3
Some important factors that should be taken into consideration when picking a diabetes medication are:
- the costs,
- patient preference,
- side effects (including weight gain), and
- the risk of a low blood sugar.4
1st and foremost- diet and nutrition

Learning about what to eat, when to eat, and how much to eat is an important component of your diabetes management. You should learn how to count and limit carbohydrates in your diet. To do this, you need to learn about what foods contain carbohydrates.
For the most part, unless your healthcare provider says otherwise, you will want to limit carbohydrates to about 45 grams per meal, and about 15 grams per snack for women. Men will limit carbohydrates to about 60 grams per meal, and 15-30 grams per snack. You could have up to 3 snacks between meals.
Learn how to read labels, looking for portion sizes, and carbohydrate grams. Learn the plate method, and how to navigate sticky situations with food, like holiday meals and special occasions.
You can learn all of these things and more by finding a Certified Diabetes Educator in your area. See our article, Everything you need to know about Certified Diabetes Educators.
Exercise, physical activity, and weight loss
It’s important for people with Type 2 diabetes to be physically active. They should aim to get in at least 30 minutes of physical activity five days per week. If weight loss is desired, a modest goal for weight loss of five to seven percent of body weight will help decrease insulin resistance, and protect remaining beta cells in the pancreas.
Research in the United Kingdom has shown that just a small amount of weight loss around the pancreas (visceral fat) will greatly reduce insulin resistance. Overall weight loss can help reduce visceral fat.
Metformin
When you are diagnosed with Type 2 diabetes, or in some cases, pre-diabetes, your healthcare provider will prescribe metformin in most cases. This is a pill that you could take once or twice daily. They will increase your dosage gradually, since the main side effect is stomach pain and diarrhea.
If you don’t get your A1C down to less than 7 percent in 3 months with diet, exercise, and metformin, the healthcare provider should look at adding in another medication. It could be a multitude of available pills, from any of the classes of medications as listed below. It could be another injectable medication that is not insulin, such as a GLP-1. Bydureon, Byetta, and Victoza are some other examples of injectable medications for diabetes that are not insulin.
What comes after metformin:
- Sulfonylureas
- Meglitinides
- Thiazolidinediones
- Alpha-glucosidase inhibitors
- Incretin agents / GLP-1
- Non-insulin injectable drugs
- Insulin
Sulfonylureas
This class of oral diabetes medication has been around for a long time. It tends to cause low blood glucose, so it is not a first line medication. Weight gain is another unfortunate side effect. I always tell my patients that sulfonylureas “punch the pancreas,”- causing it to make more insulin. They are not used often in the elderly due to low blood sugars.
Meglitinides
This oral medication for diabetes is taken three times per day, before each meal. They have a short duration, and also signal the pancreas to make more insulin. They have an A1C lowering ability of about 1 percent, and they don’t cause a low blood sugar as frequently as sulfonylureas.
Thiazolidinediones
Often called TZDs for short, this oral diabetes medication has the ability to decrease insulin resistance. On average, you may see a 1.5 percent A1C reduction with this medication. It should be used with caution in people with congestive heart failure, or not be used at all. Weight gain is a usual side effect.
Alpha-glucosidase inhibitors
This oral medication for diabetes slows the rise in blood glucose by interfering with the breakdown of starches in the foods we eat as we digest. It is taken right before the first bite of food, and thereby slowing down the blood sugar spike post meal. They have not shown to work as well as some other oral diabetes medicines, and common adverse effects are diarrhea and bloating.
Incretin mimetics and non-insulin injectables
These medications come in oral pill form, or in injectable form, and include the GLP-1 and DPP-4 inhibitors. They slow down digestion and signal the pancreas to make more insulin. These have a desired side effect of weight loss, and can lower A1C, while using the body’s natural blood glucose lowering mechanisms.
Injectables that are for diabetes, but are not insulin help the pancreas to produce more insulin. However, they may cause a side effect of nausea. Extended release injectable medications are given once weekly.
Insulin
When a combination of diet, exercise, and metformin are not enough, and you have exhausted all other medications for diabetes, it may be time to start insulin. Especially if you have tried several other medications and have not been able to lower your A1C below 7 percent, then insulin is advised.
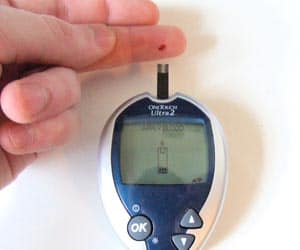
Importance of monitoring blood glucose
It is always important to monitor your blood sugar when you are trying to keep your diabetes in control. Using your glucometer, you can keep track of how many blood sugars are in your target range. Generally, your target range will be 80-130 mg/dl fasting (before you eat or drink anything in the morning). Two hours after a meal, your blood sugar target should be less than 180 mg/dl. Your healthcare provider may adjust your targets based on individual factors.
It is also a good idea to write a daily journal that chronicles what you eat, what your blood sugar levels are, and any medicine that you take, along with exercise completed.
In order to get the right combination of medications to live healthy with diabetes, you should work with your diabetes care team. Your team may include:
- nurses
- dieticians
- certified diabetes educators
- primary care practitioners
- endocrinologists who specialize in diabetes
- physical therapists
- exercise physiologists
- pharmacists
- or any number of other specialists that you may need for your individual diabetes care.
To learn about how to put together the perfect diabetes care team, see our article here: https://www.thediabetescouncil.com/how-to-build-the-perfect-diabetes-care-team/
Tips for keeping your AC1 under 7 percent:
- Make a plan and stick to it
- Build a support system network
- Read food labels – look for serving size, and total carbohydrates
- Shop for whole foods (lean meats, whole grains, fresh fruits and vegetables, and low-fat dairy products)
- shop and prep meals in advance
- Eat small frequent meals, instead of larger meals
- Get out and get moving. Turn off the TV, or watch and work out
- Decrease stress by trying relaxation techniques, meditation, yoga, or other relaxing activities
Diabetes is a balancing act
It can be a bit troublesome to try to get your diet, exercise, and medications straight. All of this effort is to have your A1C stay under 7 percent, so that you are living healthy with diabetes. However, if your A1C starts creeping up, and you have tried many other diabetes medicines in order to try to get your A1C down to no avail, don’t balk at starting insulin.
Should I start insulin?
If your healthcare provider decides that it is time for you to start insulin, then it probably is. In order to avoid long term complications when your beta cells have just given out, and are not making enough insulin anymore, you should start insulin if advised to do so. It would be better to take an insulin injection to get your A1C down below 7 percent, than it would be to end up with a non-healing ulcer, on the dialysis unit, or experience going blind.
For most people with diabetes, the goal is to keep the A1C below 7 percent, and to live healthy with diabetes. This can be achieved by using an individualized and patient-centered approach. Some important factors that should be taken into consideration when picking a diabetes medication are:
- the costs
- patient preference
- side effects (including weight gain)
- and the risk of a low blood sugar.
Further reading:
Over to you
Have you ever been told you had to go on insulin? How did it make you feel, and how did you overcome your fear?
If you have never had to go on insulin, share your success stories and difficulties of managing your diabetes with diet, exercise, and/or oral medications, or other non-insulin injections. We would love to hear from you.
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on May 30, 2020
References
- http://www.everydayhealth.com/type-2-diabetes/treatment/treatment-before-insulin
- http://www.joslin.org/info/can_i_treat_diabetes_without_drugs.html
- http://www.everydayhealth.com/hs/better-type-2-diabetes-control/diabetes-treatment-not-just-insulin/
- http://care.diabetesjournals.org/content/38/Supplement_1/S41.full