What happens when you’re diagnosed with type 2 instead of type 1?
Everyone has heard of ‘diabetes’ but what they may not be aware of is that there are a few different types of diabetes out there. Each with their own unique circumstances of development and treatment options. Unfortunately, a lot of the more widely known information about diabetes is surrounded by misconceptions which many often come with dangerous advice.
There have been way too many reports of Type 1 diabetes misdiagnoses. Even more common is the initial incorrect diagnosis of type 2 diabetes instead of the correct diagnosis of type 1. This vital mistake is an oversight in the medical profession which can have fatal consequences.
Let’s first take a look to familiarize ourselves with the differences between type 1 and type 2 diabetes:
Contents
What is Type 1 Diabetes?
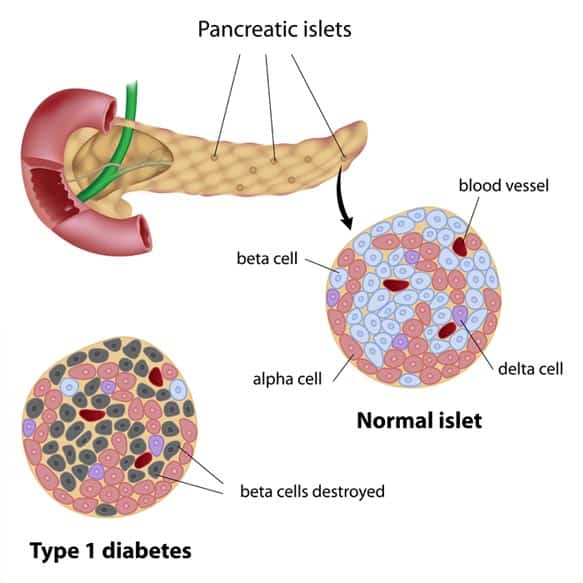
Type 1 diabetes was previously referred to as “juvenile diabetes”. It is an autoimmune disease in which the body’s own immune system sees the beta cells within the pancreas (responsible for insulin production) as invaders and launches an attack. Type one diabetes more commonly develops in children and adolescents but adults of all ages can also be diagnosed with type 1 diabetes.
When you have type one diabetes, you are insulin dependent for the rest of your life. This type of treatment regimen consists of multiple shots given daily (MDI) or with an insulin pump attached to your body with an infusion set. This infusion set features a plastic cannula placed right underneath the skin subcutaneously. The insulin pump mimics the function of the human pancreas by giving a background dose of insulin throughout the day (referred to as basal), and allows you to give yourself insulin at mealtime (referred to as bolus). You can read more about diabetes type 1 here.
What Happens When There is a Lack of Insulin?
Your body needs insulin to help balance your blood sugar levels by converting the excess glucose into energy. Without insulin, the body is not able to convert the glucose into energy and begins to instead focus on burning fat. This signals the liver to convert normal fatty acids into ketones. When released into the bloodstream, ketones can quickly become a life threatening condition, known as DKA (Diabetic Ketoacidosis)
What is Type 2 Diabetes?
Type 2 diabetes is the most common form of diabetes because it’s generally diagnosed in adults over the age of thirty-five. The pancreas ends up not producing enough insulin. The insulin that it does produce is not used properly by your body. This results a glucose build up which instead could have been used as energy.
Initial treatment options of type 2 diabetes involve lifestyle changes, oral medications and increased activity. Over time as the pancreas begins to work overtime, some people with type 2 diabetes may require an insulin regimen for their management.
I recommend you read the following guides:
So now that we know a little more about type 1 and type 2 diabetes, let's talk about why missing a type 1 diagnosis can be dangerous:
Even those in the medical profession are not up to date with all the signs and symptoms of both types. Both often have many of the same symptoms that jump out to doctors as ‘red flags’, but for type 2 diabetes.
These common symptoms include:
- Increased urination
- Increased thirst
- Slow healing wounds
- Headaches
- Lose of weight
- Fatigue
- Blurry vision
Because these symptoms occur in both types of diabetes, doctors often make the assumption that an adult cannot simply have type 1 diabetes. This sort of thinking is out of date and can prove to be fatal. There are tests that can be done to determine which type of diabetes you have, but they are not considered to be routine tests at the doctor’s office.
If reading this is making you question your diagnosis, that you may have type 1 diabetes and not type 2, please request your doctor for an antibody test for type 1.
Most adults diagnosed with type 1 diabetes have what the medical profession refers to as LADA (Latent Autoimmune Diabetes in Adults).
Signs that Your Type 2 Might Actually Be Type 1
Understanding the common signs that type 2 might actually be type 1 can help you advocate for your health.
You’re Pretty Thin
Research has suggested that up to 90% of those with type 2 diabetes are overweight. Those with LADA are often times much slimmer. Generally, there are two different body types of those with LADA.
Some patients with LADA are quite slim and may even be presenting with symptoms of DKA. These patients will require an insulin regimen much sooner than the second body type, who tend to be slightly overweight. The latter body type of LADA’s often have an easier time controlling their blood sugar levels with oral medications for many years. But as time goes on, their medications keep increasing until they are no longer producing any insulin at all on their own. The extra weight also increases their risk of developing insulin resistance, which makes controlling their blood sugar even more challenging.
You’re Following Your Management Plan, But It’s NOT Working
You find that you’re following your diabetes management plan of eating healthy and exercising, but it doesn’t seem to be helping or making much difference. If you are doing everything you are supposed to be doing and your blood sugar levels are still rising, this could mean that the beta cells in your pancreas aren’t producing as much insulin as they used to. While not getting the results you are expecting in managing diabetes can be frustrating, when you understand that you potentially have LADA instead, it makes much more sense.
Multiple Medications with Increasing Doses
If you are also taking two or more medications to control your diabetes but your blood sugar still keeps rising, there's a very good possibility that you have LADA. With LADA, your body’s immune system slowly attacks and kills off your beta cells. There really isn’t a way to predict when insulin may be required.
You or a Family Member Has an Autoimmune Disease
If you or someone in your family suffers from an autoimmune disease such as rheumatoid arthritis, Celiac disease, or Hashimotos Thyroiditis(hypothyroidism) it’s much more common that you have type one diabetes than type two.
So why is a misdiagnosis so important to watch out for?......
Many doctors misdiagnose people with type 2 diabetes instead of type 1 simply because of their age. Many doctors don’t feel the need to test for type 1 diabetes if the patient is over the age of thirty-five because young children and adolescents more commonly diagnosed with type 1.
Because of this, doctors try to treat the condition with diet and exercise first. When that does not work, they may start you on some oral medications and/or non-insulin injections to regulate your blood sugar before testing for type 1 diabetes. Often times by the time they end up testing for type 1 (LADA) in adults, their condition has deteriorated to the point they are now in DKA.
Those with type 2 diabetes can develop diabetic ketoacidosis but it’s rare when you are over the age of thirty-five. If you think you’ve been misdiagnosed with type 2 diabetes instead of type 1, watch out for these warning signs:
- Consistent vomiting for over two hours
- Sharp stomach pains or upset belly
- Breathe smells like fruit
- You easily get weak, tired, confused, or dizzy
- Trouble breathing
All these symptoms could mean you have type 1 diabetes instead of type 2 diabetes.
Conclusion
As you can see, being misdiagnosed with type 2 instead of type 1 diabetes can have some severe health effects. Experiencing a misdiagnosis is not as uncommon as most people think. In fact, one in every five people are misdiagnosed with type 2 diabetes when they actually have type 1. That’s nearly twenty percent of all new patients with diabetes!
Always speak with your healthcare provider about any symptoms you are experiencing. If you suspect you have type 1 diabetes, do your research and bring it back to your doctor to let them know why. It's important to make yourself and your doctor aware so that you can start receiving the proper treatment and avoid any preventable complications. This is a serious condition that needs to be addressed immediately before you are hospitalized or it's too late.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on September 14, 2018









