I hope that absolutely no one has been hospitalized…at least due to a low blood sugar since you read Part 1 of this 2 part series! Part I of the series is all about diabetes emergencies and how Hypoglycemia can be avoided in order to save you trip to the hospital.
In Part 2, we will be covering the emergencies related to Hyperglycemia, also called High Blood Glucose. Again, we will focus on the prevention strategies and emergencies affecting people with Type 1 Diabetes and Type 2 Diabetes only.
As mentioned in Part 1, since the emergencies affecting ladies who are pregnant are so highly specialized, consult your Obstetrician early in your pregnancy for your specific guidelines. You can further explore our website, TheDiabetesCouncil, for many informative articles related to Gestational Diabetes. There is also a great Gestational Diabetes FAQ page where you will find the answers to many of your questions on Gestational Diabetes.
Contents
Hyperglycemia (High Blood Glucose)

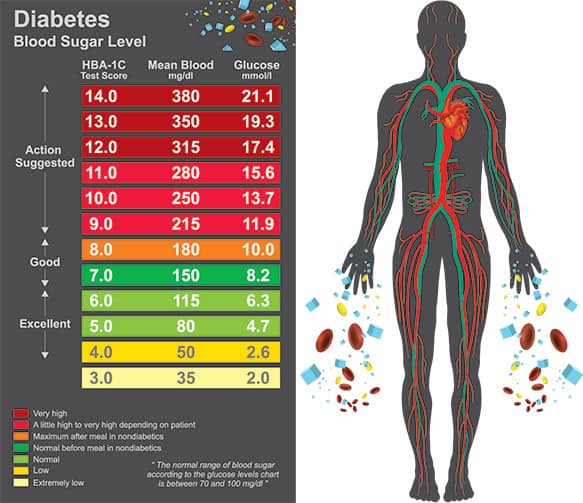
Hyperglycemia, which is also referred to as High Blood Glucose, is defined simply as an elevation of glucose (blood sugar) above normal limits. What are normal limits anyway? What are MY normal limits supposed to be? Yes, I can hear you!
Your physician or endocrinologist (physician who specializes in care of people with diabetes) is responsible for providing you with your target blood glucose levels. This article is really going to teach you about the things that can make your blood sugar high, and what you can do to avoid getting to a place where you have to dial 911. Listen, I’m am a RN, and we are the last people who want to go to the hospital if we are ill, so I understand.
What Should Your Blood Sugar Target Be?
Your target blood sugars will vary depending on how recently you were diagnosed, your age, your other health conditions, what medicines you are taking and of course, what time of day you are checking your blood sugar. Obviously, before meals, we would expect your blood glucose to be lower. After meals, we would expect it to be higher…how much higher? Depends on who you ask, right?
I can provide you with two sets of targets which all healthcare providers follow for the general population (not pediatric patients or the elderly which will have higher targets). The following one is provided by the American Diabetes Association (ADA)- The Standards of Medical Care in Diabetes-2018:
Before Meals 80-130 mg/dL
1-2 Hours After Meals Less than 180 mg/dL
American Diabetes Association (ADA)
The one below is provided by The American Association of Clinical Endocrinologists- Diabetes Guidelines (AACE/ACE)-2015:
Before Meals 80-120 mg/dL
1-2 Hours After Meals Less than 140 mg/dL
Symptoms of Hyperglycemia
We will begin with the symptoms first:
- Thirst
- Frequent urination (frequent bed-wetting for kids)
- Tiredness, sleepiness
- Blurry vision
- Dry skin
- Unintentional Weight loss (can occur over time or rapidly)
- Frequent Infections
The more serious symptoms to watch out for which indicate a need to call your physician or 911 are listed below:
- Nausea/vomiting
- Abdominal (stomach) pain or cramping
- Fruity odor to your breath
- Confusion
- Lethargy, extreme tiredness
- Trouble breathing (very late symptom) Call 911 Immediately
Treatment for Hyperglycemia
- The first action you should take is to check your blood glucose using your meter. If the numbers are very high, I normally suggest that my patients go wash their hands with soap and water and check their blood glucose again.
- Next, treat your high blood sugar with any medication your physician has given you. If you are unsure of exactly how much to take, call your doctor.
- Drink water! While this is considered a treatment for lowering blood sugar, it also helps to prevent dehydration. The water helps flush out some of that extra sugar out of your body!
- Exercise! This is also considered a treatment for high blood sugar as long as your blood sugar is not too high (above 250 mg/dL) and you do not have any of the more serious symptoms listed earlier. Exercise will lower your blood sugar.
- If you are wearing an insulin pump, you should check your infusion site and give a bolus using your insulin pump. If your blood glucose does not come down by your next check, take a manual injection of insulin and change out everything. This includes your infusion set, insulin cartridge and tubing (or pod).
- Bear in mind, you should always be using your fingertips to test your blood glucose using your meter, not testing from an alternative testing site such as your forearm. Blood glucose testing meters are made to test capillary blood which is obtained from our fingertips. Blood obtained from other areas of our body will provide inaccurate test results. Always use the dark or colored cap for your lancing device. The clear cap is for the alternate site testing.
- Remember that food or drink residue left on your fingertips can provide a falsely high reading for many hours. Washing your hands will remove this; even some lotions can affect blood glucose readings.
I recommend reading the following pieces:
Early Prevention for DKA and/or HHS
DKA is diabetic ketoacidosis and is the Hyperglycemic (High Blood Glucose) emergency for people with Type 1 Diabetes. DKA can also occur in people with Type 2 Diabetes as well.
HHS or hyperglycemic hyperosmolar nonketonic state only occurs to people with Type 2 Diabetes. Blood sugars are generally much higher with HHS where patients are much more tired and ketones are usually not present. It is rarer for a patient to be in HHS than in DKA; we do not see it as often.
What’s the difference between the two and does it really matter for you? This is where it gets confusing for the general public, because initially, sometimes it does for us on the front lines as well.
We have to rely on how the patient looks, what the tests begin revealing, and their clinical condition minute by minute to help us determine which they have. In the beginning, it really doesn’t matter since we are treating them in the same manner, which is really, very aggressively, to save their life, because both of these emergencies are life threatening.
Ultimately, for right now, it does not matter. I am going to teach you how to prevent either one by using the same rules from the DKA Prevention and Sick Day Guidelines.
DKA Prevention
- If your BG is over 250 mg/dL twice in a row, check for ketones.
- Take your medication as directed to treat your high blood sugar.
- Drink at least 8 oz of water every hour.
- Recheck you BG and ketones in 1 Hour and then every hour until normal.
- If your BG has not gone down or if you still have large ketones, contact your physician. You may need to proceed to your nearest emergency room.
- If at any time you begin having any serious symptoms listed above, call 911.
The key here is to bring down your blood sugar, get rid of ketones in your body, and prevent the dehydration. I know what I just asked you to do for which you may be laughing at me right now, but the cascade of events that lead to DKA can start occurring within just a few hours. I have seen many patients go to bed with a high blood sugar only to wake up in a state of DKA. This can happen especially quickly in children and the elderly.
If you have a BG over 250 mg/dl, treat it, recheck it in 2 hours. If it is still over 250 mg/dL, start the above DKA Prevention Guidelines. This goes for every BG over 250 mg/dL, whether it is as a result of food, illness, lack of medication, whatever. I know you have probably had many times when you have had high blood sugars like this and DKA has not occurred. You are not infallible, it will happen. Damage is occurring and your body will not be happy in a state of hyperglycemia for long periods of time and it will react.
The great news is, if you just follow these simple guidelines, you can prevent that horrible trip to the hospital and more importantly, the risk to your life.
One tip regarding ketone testing strips is that once you pop the top of the vial, opening it, they are only good for 90 days. I know they have an expiration date on them just like your insulin does and your BG test strips do. But once you open those and start using them, they go bad within a certain amount of time. Most insulins are good for 28 days once they are open and in use; BG test strips are good for 90 days once opened and in use. All 3 of these need to be kept in room temperature once opened and do not store them in your bathroom or car.
Sick Day Guidelines
The biggest thing I can teach you about Sick Days with Diabetes is take your medications!! Even if you can’t eat, check your blood sugar and take your insulin!
Why? Because your blood sugar will be higher because you are sick and you still need your insulin whether you are eating or not!
If you skipped your long acting insulin that works 24 hours because you’re not eating, your blood sugar the next day is going to be twice as high!
If you skip your fast acting insulin at breakfast because you can’t eat when you are sick, your blood sugar at lunch is going to be sky high because you didn’t correct your blood sugar at breakfast. Is this starting to make sense?
Your blood sugar will always be higher when you are sick, so always take your diabetes medications. Check your blood sugar more often, and call your doctor if:
- You can’t keep fluids down for longer than 4 hours (vomiting/diarrhea).
- You have moderate to large ketones that are not lowering.
- Your temperature is greater than 100 degrees.
- BG over 250 mg/dL is not responding to your treatment (or with any BG levels under 70 mg/dL).
- Start your DKA Prevention!
So many patients land in the hospital due to DKA when they are sick because they stopped taking their diabetes medication simply because they weren’t eating. I would be a rich woman if I had a dollar for every time I have been told that story!
Keep a Sick Day Bag of goodies at home with saltines, broth, chicken noodle soup, ginger ale, both regular and diet because you’ll need to alternate.
Causes of Hyperglycemia
- Foods
Yes, food, in particular too many carbohydrates, can raise your blood glucose. This also includes liquids, especially the concentrated forms of carbohydrates such as fruit juices, regular sodas and other sugary drinks. These are wonderful to treat a low blood sugar, but just one half of a cup (½ cup or 4 ounces) will raise your blood sugar 30 to 50 points.
I know your entire family blames every high blood sugar you have on something you have eaten. It’s been done so many times by everyone you know, maybe even by your own doctor, that you have started believing it yourself. “Those potatoes I ate at dinner last night caused my high blood sugar this morning.” I have heard this so many times and I can dispel this as a complete MYTH RIGHT NOW!!!
There is absolutely NO WAY ANY FOOD can affect your blood glucose the next day…period. High fat foods can affect your blood glucose for hours…maybe four or five at the most. How would you know? Test your blood glucose before a meal; if it is normal before, then test again 2 hours after you eat. If not normal yet, continue testing hourly until normal. This will tell you how long a certain food affects your blood glucose.
This is NOT an exact science…you will get different results every single time because there are so many factors besides food that affect your blood sugar!
The moral to the story is that we instruct our patients to check their blood sugar 2 hours after they eat. If you are not a pediatric or geriatric patient and your 2 hour after meal target is less than 140 mg/dL, then that’s your goal. If your BG was too high, you know you ate too much!
Remember, it could be a high fat food that causing it, but if you did not consume over 10 grams of fat, you know you probably just ate too many carbohydrates. If you did not eat too many carbs, then possibly, you may need an adjustment on your medications.
Only checking your blood glucose first thing in the morning is not really providing nearly enough information for your doctor. How are they going to figure out what medicines you need or what adjustments you need based on 1 BG number the same time every day? Add one extra check per day.
What I ask my patients to do is check 2 hours after any meal, alternating which meal they check after. Make it convenient for yourself; if you work all week, only check 2 hours after dinner. On the weekend, check 2 hours after breakfast one day and 2 hours after lunch another day. Keep a record of all these checks in a logbook.
Your doctor does not have time to push buttons through your meter. He barely has time to listen to your heart. Just write them down and take the logbook in; it’s the only way they are going to figure out how to adjust your medications.
- Health Conditions
Chronic diseases, along with diseases like cancer, will cause fluctuations in your blood glucose levels.
- Medications
Some medications will cause high blood glucose levels. Medications that have been implicated include: beta blockers, a diuretic, second-generation antipsychotics and protease inhibitors. Those most known for causing hyperglycemia are steroids.
Steroids can be in pill form, an inhaler, a nebulizer treatment, IM (Intramuscular) or an IV (Intravenous) medication. The last two are administered by a Healthcare Professional in their office or at a hospital. Steroids are used to reduce inflammation.
Those who have asthma (like me) have a steroid rescue inhaler and maybe even nebulizer treatments to reduce inflammation in their lungs when they have an asthma attack. They may be prescribed an oral medication (pill) call prednisone when they get sick to help reduce inflammation in the lungs. Prednisone will do wonders in opening up your lungs, but it does have a direct effect on your blood sugar also.
When you throw out your back and nothing is working…your doctor may suggest a corticosteroid injection. This will definitely help your back by reducing the inflammation, but make your doctor aware, because he or she may need to increase your diabetes medications for a few days. This takes me right to my next subject…pain.
- Pain
Pain has a direct effect on your blood glucose levels and most of you are probably already aware of this. If not, be aware, when in pain, expect your BG levels to be much higher as a result of stress hormones. Taking steps to reduce pain will make a big impact on your blood sugar levels. Please discuss this with your doctor as one of the issues.
- Medications
If you take insulin and your BG levels aren’t within your goal, please see a Certified Diabetes Educator at least once a year. The CDE can help by doing a full assessment and figuring out what your BG trends indicate. They will also do a physical exam to assess your insulin injection sites, discuss if you are rotating, how you use your insulin pen or vial and syringe, how you store your insulins. We continue until we figure out if there are any issues that might be contributing to your higher blood sugars.
For the majority of the patients that I see who have been on insulin for years, most are doing at least one thing incorrectly. One thing they were just never educated one that makes a huge difference in their blood sugars.
For example, one thing that I see very often with insulin pen users is that they will store the pen needles on the pens or use the pens until all the insulin is gone (like 2-3 months). No one ever told them WHY is it important to never do this! So, with the pen needle off, the cartridge is airtight. When the pen needle is on, the insulin is constantly exposed to air, causing it to go bad pretty quickly. It is like injecting water, not full strength insulin. Same with using insulin past the 28 days, it loses its strength. So, the patients think they are just saving some time and money by leaving it on there or using the pen until its empty, but they are really losing that entire insulin pen.
- Too Little or Lack of Medications
This could be due to many different factors. Patients sometimes stop taking their medications due to cognitive issues (dementia, forgetfulness, age) and there is no caretaker checking their blood glucose to see how high it becomes. Depression can cause people to just stop taking all their medications. Cost can become an issue at any time and cause a person to stop taking a certain medication or all of their medications. Drug abuse can cause a person to stop caring about taking their diabetes medications. These are the people I typically see in the hospital and some of the reasons that led to them stopping or taking less medication than they were supposed to take.
One thing which is difficult for most people to understand is that what is working today as far as your treatment…your pill or insulin doses, will not work 6 months from now. That is the nature of this disease, especially for people with Type 2 Diabetes. Your pancreas will not be secreting the same amount of insulin 6 months from now as it does today.
Unfortunately, diabetes is a chronic, progressive disease. Exercise and weight loss do help tremendously, but we have not found a potion yet to make your pancreas start producing the perfect amount of insulin again and cure your diabetes.
Weight changes do make a big impact on how much medication you need. If you have lost a lot of weight through diet and exercise recently, you probably won’t need as much medication. However, if you have lost 10 pounds in the past week and all your blood sugars have been over 250 mg/dL, you need to call your doctor immediately, because you need more medication now!
- Time of Day
The time of day that you are testing plays a big role in how high your blood glucose will be. For most people, checking fasting (first thing in the morning) will be the lowest point in the day. For other people, that may be a higher time for them due to hormonal changes called the Dawn Pheomenon and/or the Somogyi Effect which I touched on in my Part 1 article. Other times of day which should be low are before your meals.
Infections and Illness
Whenever you are sick or have any type of infection, expect your blood sugar to be high. Sometimes your blood sugars may go up a day or so prior to when you start feeling bad. I see this happen often in children that come in with DKA. We can’t find the source of their high blood sugars; everyone did all their preventive measures perfectly, then about 24 hours into their hospitalization, the child develops a fever. Sometimes it’s just our body’s way of letting us know we are sick.
I also have seen it often through the years with the elderly. Older women may not have symptoms of urinary tract infections (bladder infections); the only symptoms may be confusion and really high blood sugars if they have diabetes.
Foot wounds are another common source; most people for some reason, do not take their foot wounds seriously at all when they have diabetes.
Unfortunately, this is normally a grave error if they wait too long. The lesson here? If you have a foot wound, have it treated early. If your blood sugars starts rising and your foot wound isn’t healing, it is likely infected and needs to be treated immediately.
Further reading:
Stress
This is an often overlooked cause of hyperglycemia, but a very important one which I always ask my patients about. There are physiological reasons, hormonal ones of course, that cause your blood sugar to spike in the presence of stress. It is immediate and observable on a continuous glucose monitoring graph. I have seen it myself.
I saw a young patient some years ago for a 3 day diagnostic continuous glucose monitor (CGM) to determine trends causing her elevated A1c and blood glucose levels. She was to wear the CGM for 3 days and journal everything she ate, the insulin she took and any special situations, such as exercise, low blood sugars, etc…logging exactly what time each event occurred.
Three days later, the young lady returned and I uploaded the information, alarmed to see one spike from 100 mg/dL to 400 mg/dL that happened immediate. It remained for an hour, after which her blood sugar returned back to 100 mg/dL. I went through her journal and flipped to that day and time and was shocked at what I read, “Fight with best friend on phone for 1 hour.”
When she returned for her session with me to review the results, she was astounded at the direct effect that stress had on her blood sugar. I explained the effect of stress hormones and their effect on BG, but to be able to illustrate it to her was absolutely priceless.
This happens in YOUR daily life too! You might try to blame it away on the food you’re eating, or the medications you’re taking, but sometimes, stress can be much more of a factor in your diabetes than any of us realizes.
I see people all the time who are eating great, exercising and taking a ton of medication, but are under a tremendous amount of stress. Now, stress is difficult to run from, but there are ways to help lower your stress levels. First, figure out the cause of your stress: is it self-imposed, and if not, where is it coming from? Are you doing it to yourself by over-committing or is it your family asking for too much?
Is it work related? Are you working in a job that you love? I am very lucky right now in my life to be working in a job with people I really admire and respect, caring for people with diabetes. I look forward to going to work. I also enjoy writing articles about diabetes that I can share with all of you. This was not always the case…there were times when I was in jobs that were not a perfect fit for me. I was constantly stressed when I went to those jobs.
Take time for yourself to relax, recharge and do things you love to do. Take a bath, read a book, sit by a fire, take a walk. These things will go a long way in reducing stress in your life.
Ask for help!
As I said in Part 1, please remember to reach out to all members of your Diabetes Team for support. Your physician, their nurse, your Certified Diabetes Educator, even a therapist or counselor is sometimes needed to help you get through difficult times. Speak up! Tell someone, because this is your health and we are here to help you in any way we can.
Please let us know any suggestions you have for keeping your blood sugars low in the comments section below and thank you so much for taking the time to read my article today. Also share the article with those who might find it useful.
To Review…
- Know when to check your blood sugars and what your targets are!
- Know the symptoms of Hyperglycemia
- Know when to call your doctor and when to call 911!
- Know the DKA Prevention and Sick Day Guidelines
- Know when to check for Ketones
- Check your blood sugar more often on Sick Days
- Know what all of the causes of hyperglycemia are!
TheDiabetesCouncil Article | Reviewed by Dr. Jerry Ramos MD on May 30, 2020
References:
- https://www.thediabetescouncil.com/prevent-hospitalization-result-diabetes-part-1/
- https://my.clevelandclinic.org/health/articles/11443-blood-sugar-what-causes-high-blood-sugar-levels-in-the-morning
- http://clinical.diabetesjournals.org/content/diaclin/early/2017/12/07/cd17-0119.full.pdf
- https://www.aace.com/files/dm-guidelines-ccp.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK279052/
- https://www.thediabetescouncil.com/the-ultimate-guide-to-ketone-testing/
- http://spectrum.diabetesjournals.org/content/24/4/234