People with diabetes are twice as likely to be at risk of having glaucoma compared to people without diabetes. We will first look at how the eye works, what glaucoma is, followed by the relationship between glaucoma and diabetes.
Clara’s story
Clara’s eyes were feeling tired all of the time. She was attributing the tiredness to her Type 2 diabetes, but she wasn’t too sure about it. That’s why she contacted TheDiabetesCouncil to raise her concerns about the increasing pressure in her eyes.
Her left eye had suddenly become red, and she was experiencing sharp pain in her eyes. She had somewhat of a headache, too. After hearing about Clara’s symptoms, she was advised to see her eye doctor for an examination, as glaucoma was suspected.
Clara got in touch with us to report that she had been to her ophthalmologist, and she had been diagnosed with the most common type of glaucoma, open-angle glaucoma. She was using some drops in both eyes, and she relayed that she was feeling better, and that the pain in her eye and other symptoms have subsided.
To help others in Clara’s situation, we have written this comprehensive guide about glaucoma and diabetes.
How does the eye work?
If you want to understand eye diseases, specifically glaucoma, it's important to understand how the eye operates.
It’s an incredible, wonderful organ! Without our eyes, we could not see the world around us. The eye is a spherically shaped organ that has a tough outer surface. The covering in the front of the eye is curvy. This covering is called the cornea. The cornea serves to protect the eye.
Light makes its way through the eye by way of the anterior chamber. In this chamber, there is fluid called aqueous humor that the light travels through. Light then goes through the pupil or hole in the iris, which is the colored part of the eye. Light then hits a lens that works on focusing the light some more. Next, light goes through another chamber with fluid in it. This is called the vitreous. At this point, light reflects off the back of the eye called the retina.
The retina then takes note of all of the images including the fine details picked up by the macula, and transmits that information to the brain by the way of electrical activity. The brain then receives the messages about the images seen by the eye. The brain can then process the images. In a word, amazing!
I suggest reading the following articles:
What is glaucoma?
When you think of glaucoma, imagine sore, swollen eyes, and increasing pressure. If just thinking about it hurts your eyes, you are not alone. Glaucoma takes its toll on the optic nerve, and tends to get worse as time goes on.
Like diabetes, glaucoma can run in families and gets worse with age. Interestingly enough, there are no early warning signs, and many people have no symptoms at all when they first find out that they have glaucoma. As high blood pressure can silently damage your heart, glaucoma can similarly damage your eyes and cause blindness.
That’s why a trip to the ophthalmologist may help you to continue to “see the light.”
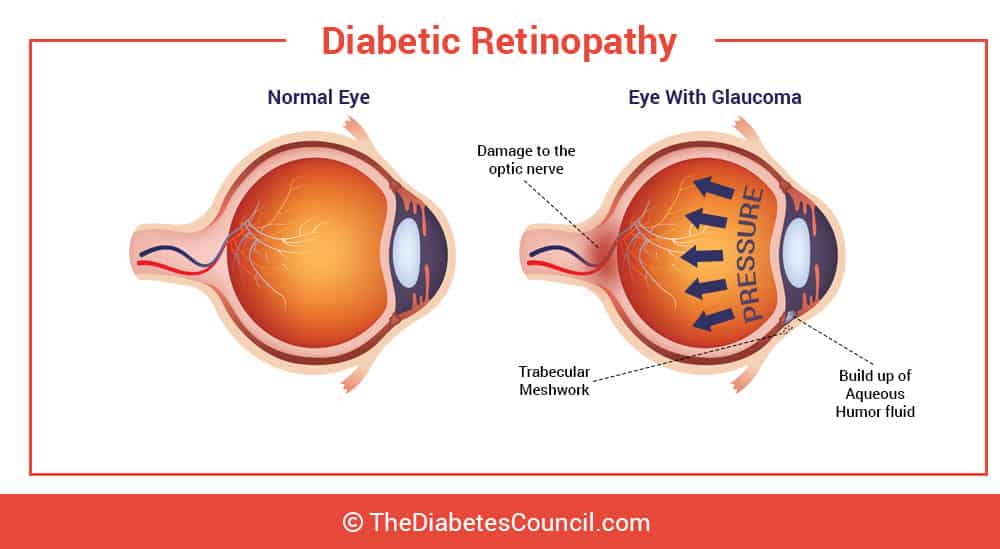
Glaucoma happens when there is pressure built up in your eye over a long period of time. This prolonged pressure in the eye is called “intraocular pressure.” If left unchecked, the pressure from glaucoma can injure the optic nerve. The optic nerve is the nerve that extends from the back of your eyeball. The optic nerve relays the picture of what your eyes see to the brain. Damage to the optic nerve can cause permanent vision loss. With no treatment for glaucoma, the result is blindness. Blindness can progress rapidly within a few years when glaucoma is left untreated.
Why is there so much pressure?
In glaucoma, the increased intraocular pressure is related to stagnated fluid (called aqueous humor) in the eye. In other words, the fluid doesn’t flow around the eye the way that it does in a normal, healthy eye with no glaucoma and no intraocular pressure. The fluid can’t get through the channel in the eye, and may even get blocked and build up. The end result is glaucoma.
Causes of glaucoma
If there is injury to the eye, glaucoma can occur as a result of the injury. It could be an injury from an object, or from a certain chemical that manages to get in the eye. Eye infections that become severe can cause glaucoma, as can a blocked blood vessel in the eye. Any inflammation in the eyes can cause glaucoma. Eye surgery can cause glaucoma in a rare instance. Both eyes are usually affected, although one eye may be worse than the other. People with diabetes are twice as likely to be at risk of having glaucoma compared to people without diabetes. Diabetes is one of the main risk factors for glaucoma, as we will discuss more as we move on.
Two types of glaucoma, and one rare type of glaucoma
Primary Open-angle (POAG) or wide-angle glaucoma
The first type of glaucoma is called open-angle glaucoma or wide-angle glaucoma, and it is the most common type of glaucoma. It occurs in a full 90 percent of glaucoma cases.
This condition can occur when the mesh-like channel gets blocked, and the fluid, or aqueous humor, is unable to flow through the eye efficiently.
Angle-closure glaucoma
This kind of glaucoma is seen more in Asian countries than in the Western world. Other names for it include acute or chronic angle-closure or narrow-angle glaucoma. The space between your iris and your cornea gets too small in this kind of glaucoma. This causes a buildup of intraocular pressure. People with this kind of glaucoma are more likely to have cataracts, and are more likely to be farsighted.
Neovascular glaucoma
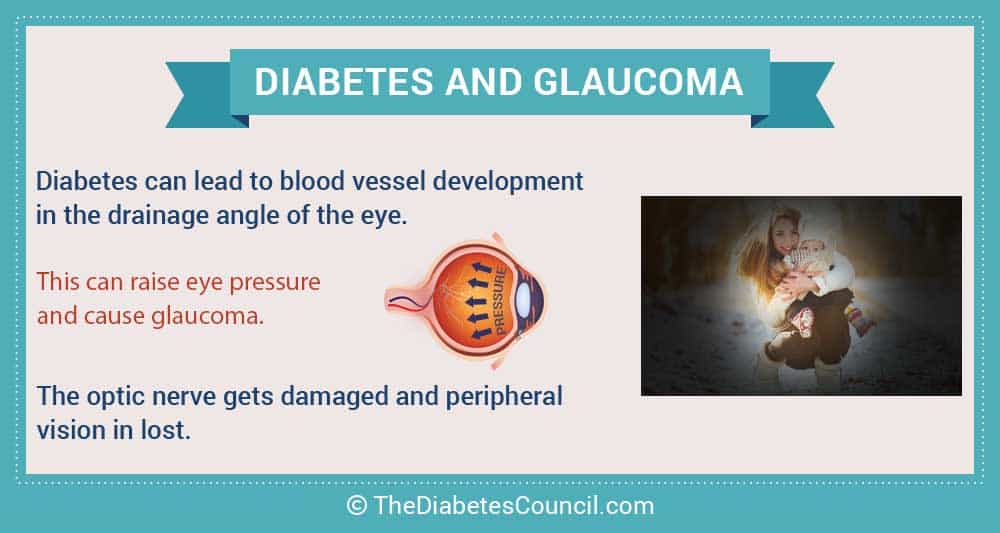
Neovascular glaucoma occurs rarely, but is often associated with diabetes. This is due to diabetic retinopathy. What happens is the eye forms collateral circulation, or new blood vessels around the retina, in order to move fluid through that is blocked. When the new blood vessels grow into the iris of the eye (colored part), this shuts off the flow of aqueous humor (fluid) through the eye, thereby raising the intraocular pressure.
This type of glaucoma is notoriously difficult to treat. Laser surgery is one option that is available to patients. There has been some limited success using drainage implants in this type of glaucoma.
How does loss of sight progress in glaucoma?
In the beginning, there are no symptoms of glaucoma, therefore sight may be normal. After a period of time, poor vision may develop in one area of the visual field. Often this is on the side, or in the peripheral field of vision. After a while with the increased intraocular pressure, more vision is lost gradually until the loss of vision extends to the entire field of vision.
Am I at risk for glaucoma?
What puts you at risk for glaucoma?
There are a number of factors that come into play. Diabetes, in fact, is one of the main risk factors or causes, and people with diabetes get glaucoma twice as often as people without diabetes.
In addition to diabetes, the following factors put you at increased risk for glaucoma:
- “halos” around lights
- sudden loss of vision or loss of vision
- severe eye redness
- in infants, an eye that looks hazy
- nausea or vomiting
- eye pain
- tunnel vision
Symptoms of glaucoma
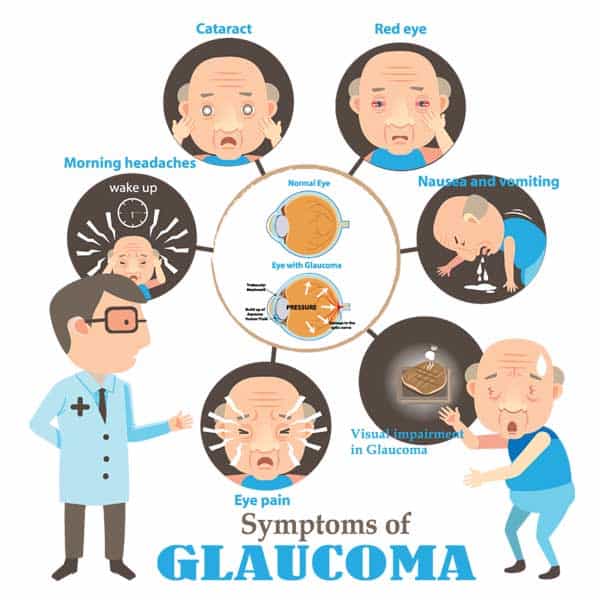
Early identification of the disease can prevent blindness; therefore those over 40 years old should have an eye examination at least every two years. When pressure rises to maximum levels, it can cause sudden and severe eye pain. The person may get severe headaches, their vision may be compromised, or the person may see “halos” around lights. At any rate, if any of the following symptoms are present, seek immediate consultation of an ophthalmologist to evaluate for glaucoma.
The following symptoms are worth seeking immediate medical attention for:
- “halos” around lights
- sudden loss of vision or loss of vision
- severe eye redness
- in infants, an eye that looks hazy
- nausea or vomiting
- eye pain
- tunnel vision
Pain in the eye: How do I get a diagnosis?
For starters, have your primary care provider refer you to an ophthalmologist, or call one yourself if your insurance doesn’t require a referral. An ophthalmologist is different than an optometrist. Ask around the community for recommendations if you are not sure where to find a good one.
Once in the doctor’s chair, they will put some drops in your eyes to dilate or make your pupil larger. This allows the doctor to see the back of your eye, including the optic nerve, to determine if the nerve is healthy. He or she will probably take photographs of your optic nerve in order to compare it with photographs over time. A tonometry test will check your eye pressure. Of course, a vision field test and other related tests will also be done. The ophthalmologist will be checking to see if you have lost either your side or your peripheral vision. None of the tests are painful.
I have glaucoma. Now what kind of treatment is there?
Once your doctor has diagnosed you with glaucoma, you may be thinking, “Now what?”. The ophthalmologist could either give you prescription eye drops, or suggest microsurgery or laser surgery. It’s possible that you may require a combination of two treatments, such as medication and laser surgery. Let’s look at the current available treatments for glaucoma.
Prescription eye drops for glaucoma
There are two types of eye drops to treat glaucoma. One kind of eye drop reduces fluid in the eye, while the other kind of eye drop medication helps the fluid, or aqueous humor, to flow as it should through the eye’s mesh channel. Your eye doctor will ask you about your other medications, any allergies to any medications, and if you have problems with your heart or lungs. This is because some ophthalmic medications for glaucoma can affect your heart and lungs. Some patients may require more than one kind of prescription eye drops for their glaucoma.
Side effects of prescription eye drops for glaucoma
Side effects for prescription eye drops for glaucoma can be:
- allergic reaction
- redness
- burning
- blurry vision
- dry, irritated eyes
Laser surgery for glaucoma
There is a particular type of laser surgery that can be performed on a patient with glaucoma to reduce intraocular pressure. This laser procedure has been around for over 20 years. Once it is confirmed that the eye drops can no longer get the pressure in the eye down enough, or when there are too many side effects from the medication, laser treatment may be an option for such patients. It may also be used when intraocular pressure is severe as a first line treatment.
Who is a candidate for laser surgery for glaucoma?
The procedure works for open angle glaucoma with high intraocular pressure. It is only for open angle glaucoma because there cannot be any blockage in the drainage system in the eye for the procedure to be performed. Your eye doctor will need to evaluate your situation to determine if you are a candidate for this laser surgery.
How does Selective Laser Trabeculoplasty (SLT) work?
The laser is applied to tissues in the eye that are part of the drainage system of the eye. This allows for better drainage of the fluid to release the pressure. This doesn’t happen overnight or directly after the laser procedure. It can take up to 3 months for the full results of the laser treatment to realize.
The laser is referred to as a “cold laser.” This is because not much heat is used, and there is less subsequent scar tissue and pain associated with the procedure.
How effective is laser treatment for glaucoma?
There are few side effects with laser surgery for glaucoma. Prescription eye drops in fact have a much greater incidence of adverse side effects. The post-operative inflammation is generally minimal. The intraocular pressure is generally lowered by about 30 percent when laser surgery is the first line of treatment. It’s somewhat similar in effect to patients who use “prostaglandin analogs,” a class of eye drops for glaucoma. The treatment remains effective for up to 1 to 5 years or more. A second laser procedure may be performed if the first treatment failed, as evidenced by increasing intraocular pressure. The second treatment doesn’t usually last as long as the first one did. A third treatment is not considered to be effective. If surgery fails, patients are put back on eye drops for glaucoma, or they may try eye surgery.
Even if the surgery is successful, the patient may only get some benefit, and may need to use prescription eye drops for glaucoma as well. It’s important for the patient to understand that laser treatment for glaucoma is not a cure. There is currently no cure for glaucoma.
SLT is FDA approved, therefore insurance including Medicare, Medicaid, and private plans cover it. Check with your insurance carrier to find out if the surgery will be covered, and how much your co-pay or out-of-pocket expenses will cost.
Microsurgery for glaucoma
When prescription eye drops and laser surgery do not work to decrease intraocular pressure, you may require microsurgery.
Trabeculectomy microsurgery (glaucoma filtering surgery) for glaucoma
In a trabeculectomy, the eye surgeon cuts a small hole in the white part of the eye (sclera). This hole makes it possible for fluid that is trapped to move through the mesh channels in the eye. This in turn lowers pressure in the eye, and protects the optic nerve from damage caused by eye pressure.
What to expect before surgery
Local anesthesia or intravenous sedation will be used, and you will not feel anything. The patient will have a medication injected behind the eye to paralyze the eye so it does not move during the surgery.
What to expect after surgery
Following the surgery, you can expect red and irritated eyes. You will likely notice that your eyes are watering more than they usually do. When fluid is allowed to flow through the eye because of the surgically created hole in the sclera, a raised, blistered area may form. This is called a “bleb.” It will be located on the upper portion of the eye and is not usually seen because the eyelid covers it.
What kind of problems can I have after this surgery?
If the surgically created hole in the sclera closes up, then eye pressure will go up again. Your body will try to repair the damage created by the surgeon, and heal the hole in your eye as your body would try to do with any other injury in your body. For younger people, this healing may occur even more rapidly. To help slow the healing process so that your body does not close this very useful surgically made hole, the surgeon may prescribe anti-wound healing drugs like mitomycin-C and 5-FU.
If the drainage hole closes up, the surgery can be repeated in the same eye several times.
Valve implantation surgery for glaucoma
Another method to drain the eye fluid and relieve intraocular pressure is a valve implantation. For this surgery, the surgeon places drainage devices called seton, valves, tubes, or shunts, into the eye. This is generally reserved for those whose treatment has failed. By the time they get to this surgery, they have tried prescription eye drops, laser treatments, and trabeculectomy.
What to expect before surgery
This surgery is done outpatient, using a local anesthetic that is injected into the side of the affected eye. You will be sedated, and you will not feel anything. During the surgery, they use a microscope to look into your eye and see all the details. It takes around an hour, or longer if the patient has already had some eye surgeries, or if they have eye problems, such as inflammation or abnormal blood vessels from collateral circulation that builds up around the eye in response to the increased intraocular pressure.
What to expect after surgery
Your eyes are delicate organs; therefore there will be some irritation, tearing, and discomfort following this surgery. You will need to avoid certain activities following surgery, such as lifting anything over ten pounds, bending over, or straining with a bowel movement. You can expect a good measure of blurry vision. Aftercare is very important following this surgery, so make sure to follow your surgeon’s instructions post op. You will likely make frequent trips to the eye surgeon during recovery.
Why do people with diabetes get glaucoma more than those without diabetes?
The reason why people with diabetes get glaucoma twice as often as people without diabetes is still quite unclear.
There has not been a whole lot of research done to date. While researchers do disagree on whether diabetes causes glaucoma, they do agree that the insulin resistance in Type 2 diabetes causes a rare type of glaucoma, neovascular glaucoma. Similarly and conversely, people with glaucoma tend to get diagnosed with diabetes twice as often as people without glaucoma. So what is it? What is the relationship between diabetes and glaucoma, and vice-versa?
The link between diabetic retinopathy and glaucoma
Many of these conditions can cause blindness. Diabetes is a complex disease in which micro vascular complications happen all over the body as a result of high blood glucose.
It is no different for the eyes. The tiny vessels going to and from the eyes can become damaged. This is called diabetic retinopathy, which we will discuss further below. Sometimes the damage occurs in the form of increasing intraocular pressure, the primary problem in glaucoma. Glaucoma is just one of the diseases that can affect the eye of a person with diabetes. In addition to glaucoma and diabetic retinopathy, cataracts also pose a problem for people with diabetes. Cataracts are a cloudy covering over the lens of the eye that forms, and causes blurred vision. Cataract surgery is generally required to restore functional vision.
The relationship between diabetes and glaucoma is complicated, and confusing!
The relationship between diabetes and glaucoma is very complicated, and often confusing. The relationship is affected by the type of diabetes and the type of glaucoma one may have. Both must be identified in order to examine the relationship between the two, hence the confusion. With all types of diabetes, when left uncontrolled for a long time, there can be the development of diabetic retinopathy. We know that this leads to neovascular glaucoma, which is rare, but what about other types of glaucoma?
Does diabetes lead to other kinds of glaucoma besides neovascular glaucoma?
The million-dollar question here is: does Type 1 Diabetes and Type 2 diabetes lead to any other forms of glaucoma? We might be interested to know whether or not there is a link to the most common form of glaucoma in the Western hemisphere, POAG (Primary Open-Angle Glaucoma).
Is Type 1 diabetes a risk factor for Primary Open-Angle Glaucoma?
Although there is not much research to back it up, it appears that Type 1 diabetes is, at least, not a risk factor for POAG. Hyperglycemia in Type 1 diabetes makes retinal ganglion cells function better, not worse. This may be why a confirmed link has not been found between Type 1 diabetes and POAG.
Is Type 2 diabetes a risk factor for Primary Open-Angle Glaucoma?
When looking at Type 2 diabetes as a risk factor for the most common type of glaucoma, POAG, there does indeed seem to be a link for this. Of 47 studies including 3 million people, most with Type 2 diabetes and most with POAG, conclusions were that the length of time that someone has Type 2 diabetes and elevated fasting blood glucose levels were related to higher intraocular pressure.
However, this research was not without its problems and there may have been some biases. For one thing, detection for glaucoma is easier for those with diabetes, as they are already expected to have a vision examination one time per year. Therefore, glaucoma in these patients may be picked up by ophthalmologists based on the simple fact that the patient is there for detection of glaucoma. Despite this, research results have been strong and are reproducible.
Research points to insulin resistance in Type 2 diabetes being a contributing factor to glaucoma. Reducing insulin resistance should be the goal for patients for a myriad of health reasons, not just for glaucoma. One benefit for patients of reducing insulin resistance is lowered intraocular pressure, and a reduction in risk for POAG. However, more studies are needed to nail down the link between Type 2 diabetes and glaucoma.
What is diabetic retinopathy, and how does it lead to glaucoma?
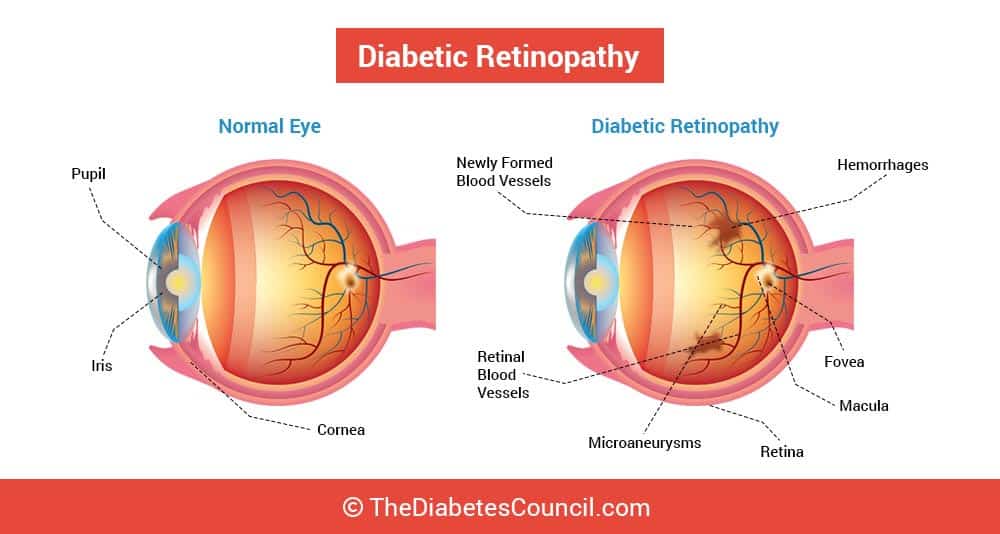
The retina is the tissue in the eye that is sensitive to light, and is found on the lining in the back of the eye. Diabetic retinopathy is the most common eye disease for people with diabetes. Leaky blood vessels and decreased blood supply to the retina hinders oxygen in the retina. Then the retina will start to make a new network of blood vessels to try and get oxygen needed to the tissues. When the circulation problem leads to increased intraocular pressure from poor drainage of the aqueous humor (fluid), as sometimes happens, there you have it! Voila!!!- Glaucoma. People with diabetes are affected by retinopathy, and it amounts to 7.7 million people with diabetes in the United States aged 40 and over.
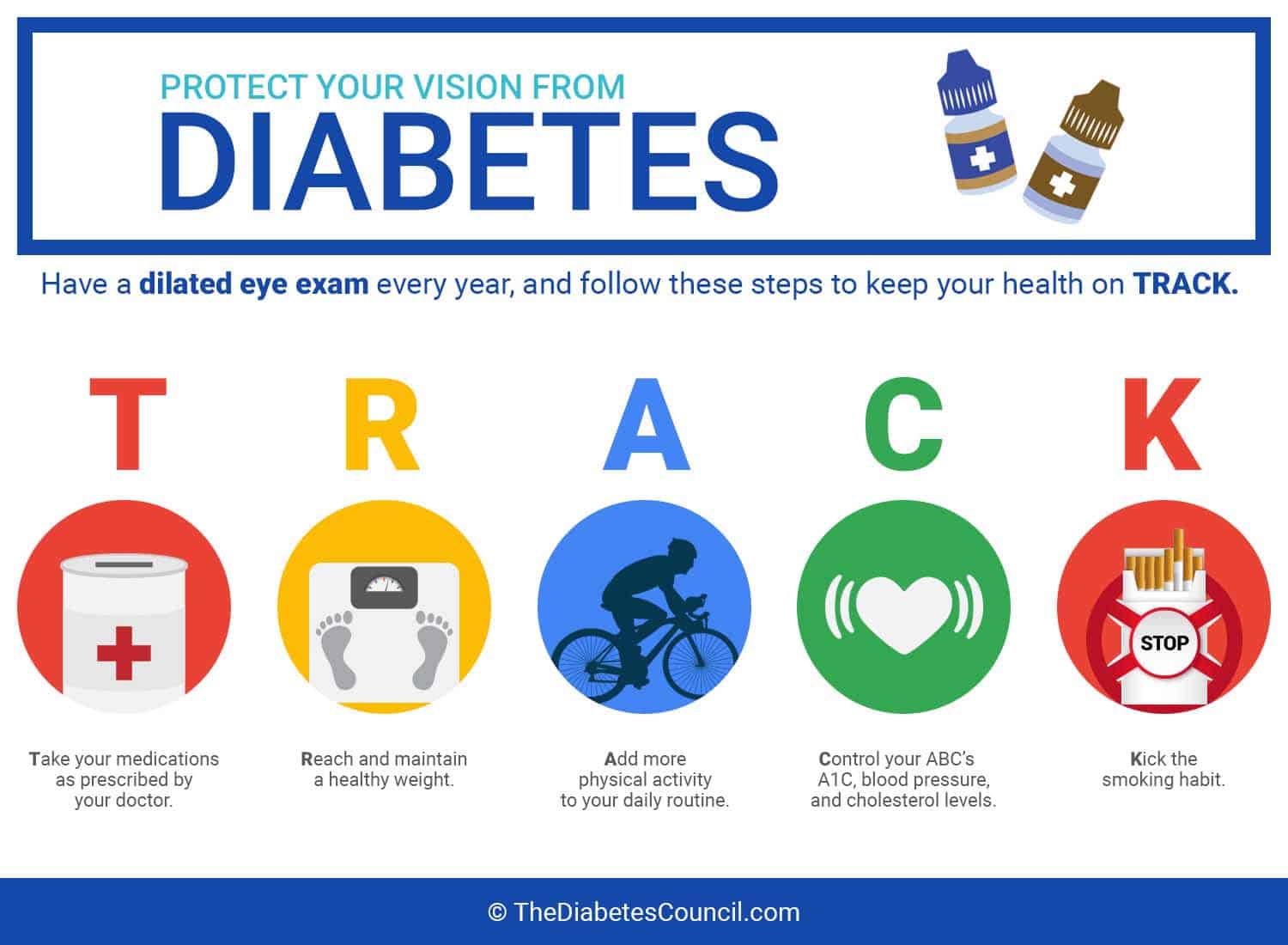
If you have Type 2 diabetes, what is the best way to prevent glaucoma?
As with many things, primary prevention of glaucoma is key. By taking care of your diabetes, you will have less risk for glaucoma.
Efficiently managing your diabetes, keeping your A1C below 7 percent in most cases and blood glucose in target ranges will go a long way in preventing the onset of glaucoma. Early detection is a must for protecting your sight, and it is imperative that treatments are rendered in order to keep glaucoma from getting worse. If you have diabetes, you should have a glaucoma test every year along with your dilated eye examination. Even if you never develop glaucoma, diabetes is the number one cause of blindness for adults 20 to 74 years of age. A yearly dilated eye exam is a must to prevent loss of sight from diabetes, no matter what the cause. Besides glaucoma, people with diabetes can lose their sight from diabetic retinopathy and cataracts as well.
Is glaucoma a side effect of diabetes?
No, glaucoma is not a side effect of diabetes. Diabetes is a risk factor for glaucoma. However, glaucoma is one of the eye complications that can result from poorly controlled diabetes.
What is the prevalence of glaucoma in peoples with diabetes?
Almost everyone is at risk for glaucoma. There are 3,000,000 people in the US who have been diagnosed with the disease. It is estimated that about half of the people are undiagnosed. Based on research, about 2.71 percent of people with diabetes had open-angle glaucoma. This statistic may be surprising: as it does stand to reason that incidence of glaucoma in diabetes would be higher.
Further reading:
Am I at risk?

With Type 1 diabetes, POAG risk is not increased. However, when diabetic retinopathy develops, either in a person with Type 1 diabetes or in a person with Type 2 diabetes, neovascular glaucoma can occur.
As always, we invite our readers to share their insights, advice and any other additional missed information in the comment section below. If you any glaucoma story let us know down below as well.
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on June 01, 2020
References
- http://www.diabetes.org/living-with-diabetes/complications/eye-complications/
- http://www.diabetesforecast.org/2013/may/does-diabetes-cause-glaucoma.html
- http://www.diabeticretinopathy.org.uk/diabetes_glaucoma.html
- http://www.glaucoma.org/treatment/selective-laser-trabeculoplasty-10-commonly-asked-questions.php
- http://www.visionaware.org/blog/visionaware-blog/could-glaucoma-actually-be-diabetes-of-the-brain-a-new-hypothesis-says-maybe/12
- http://ophthalmologytimes.modernmedicine.com/news/are-patients-diabetes-more-susceptible-open-angle-glaucoma?page=full
- http://www.sciencedirect.com/science/article/pii/S0161642097302474
- http://www.diabetes.org/living-with-diabetes/complications/eye-complications/
- https://www.sciencedaily.com/releases/2011/08/110817120237.htm