Unfortunately, renal failure or nephropathy (commonly referred to as kidney failure) and unmanaged diabetes go hand in hand. In addition, 50 percent of people with diabetes will experience some form of kidney damage in their lifetime, even if they never experience kidney failure or end up on dialysis.
In this article, we will look at how renal failure and insufficiency can have an impact on people with diabetes, and how people with diabetes can avoid renal failure and dialysis. We will look at risk factors, causes, and symptoms, as we explore the relationship between renal failure, diabetes, and high blood glucose.
We will also look at what happens to a person with diabetes when their kidneys fail. We will discuss dialysis and kidney transplantation.
First, let’s see what Lydia had to say when she contacted TheDiabetesCouncil.
Contents
Lydia’s story
Lydia had received a laboratory result from her doctor that was very alarming to her. She had an excess amount of protein in her urine, usually an early sign of kidney damage. He informed Lydia that her kidneys were being affected by her diabetes, and she needed to work on self-managing her diabetes. He ordered some more tests to further look at her kidneys.
Was Lydia headed to the kidney dialysis center? Her friend Tracey, whom she’d met in a diabetes support group had been the first person she knew who was on dialysis. Tracey seemed to have a very difficult life in and out of the dialysis center. Lydia was afraid to end up like Tracey.
Lydia knew that she hadn’t been efficiently self-managing her diabetes. Her A1C had been greater than 8 percent a few times over the last few years. While most of the time she kept it around 7.5 percent, she was aware that her doctor wanted her to get it below 7 percent, and keep it there in order to avoid diabetes complication, including kidney disease.
Lydia’s doctor had her attention now. She was now ready to set goals to get her diabetes back on track in order to avoid kidney and other related complications, and live a healthy life with diabetes. We decided to invest some time and research into helping Lydia and others with diabetes understand the connection between kidney, blood pressure and diabetes.
It would be great if all people with diabetes could avoid the dialysis center and live healthy with diabetes. After all, it’s not so much the diabetes that’s the problem – it’s the high blood glucose! Now let’s get started, and see what we can find out to help Lydia, and possibly you as well!!!
Lydia’s doctor had first done a microalbumin test on her urine that showed protein into her urine. She had protein amounts that were higher than the cut-off, so her doctor ordered more tests. He probably ordered a GFR (Glomerular Filtration Rate), to determine if there was any kidney damage, and the extent of it.
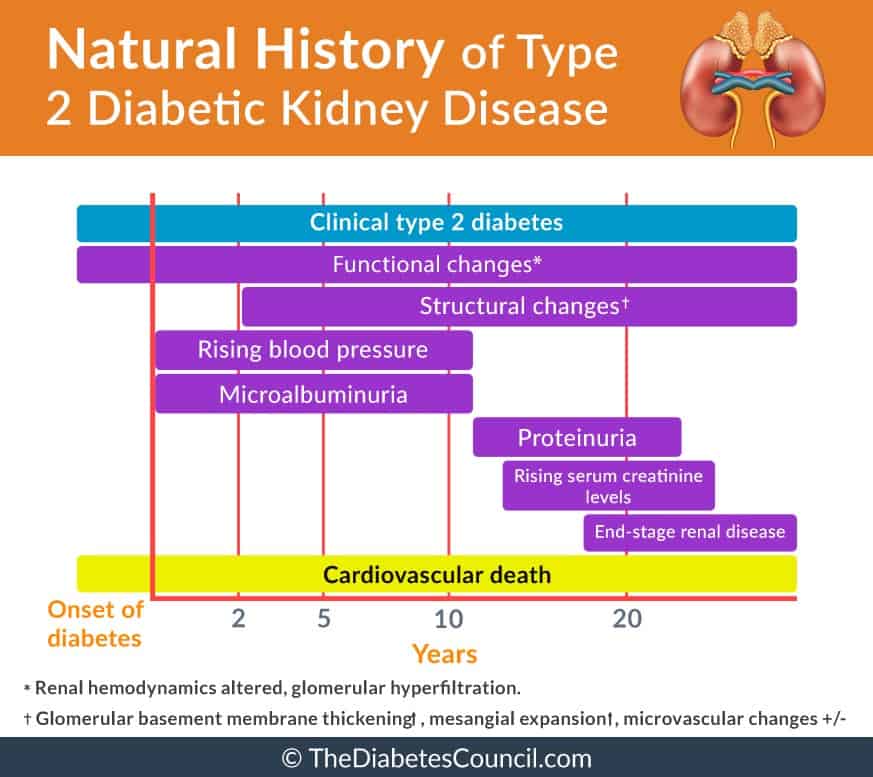
What is renal failure?
In a research conducted by Ravi Retnakaran et al. entitled ‘Risk Factors for Renal Dysfunction in Type 2 Diabetes’, they confirm that type 2 diabetes was the leading cause of end-stage renal disease (ESRD). While not all, many patients with type 2 diabetes will likely develop renal dysfunction during their lifetime. In the U.K. Prospective Diabetes Study, it was shown that 24.9% of patients developed microalbuminuria within 10 years of diagnosis of type 2 diabetes, but only 0.8% of those developed ESRD, as assessed by elevated plasma creatinine (>250 μmol/l) or the need for renal replacement therapy.
Each year, over 100,000 people will be diagnosed with kidney failure in the United States. Forty-four percent of these cases are caused by diabetes. It presents a significant financial burden, as well as a physical, mental and emotional on patients and their families, and accounts for 32 million in medical costs per year.
Renal failure is the end result of CKD (Chronic Kidney Disease). Renal failure, also known as nephropathy, renal insufficiency, or kidney failure, is a condition in which the kidneys do not function properly, and do not filter waste products from the blood. Renal failure is Filtering waste products from the blood is the main function of the kidneys.
Types of kidney failure
Related to the kidneys, two bean-shaped organs located in the upper abdominal cavity, there are two different kinds of failure.
First, there is Acute Kidney Failure. This kind of kidney failure is usually reversible, and there is usually a cause for it. In Chronic Kidney Failure, there is usually also a cause, but the damage is irreversible.
In Chronic Kidney failure, the damage is not an “acute” attack on the kidneys, but rather a chronic wearing down of the kidney’s functioning over time. People with diabetes can have acute kidney failure. However, they most often have chronic kidney failure.
I advise reading the following articles:
Chronic Renal failure in people with diabetes, or diabetic kidney disease
For our purposes, we will focus on chronic kidney failure.
Chronic kidney failure in people with diabetes can be referred to as diabetic kidney disease. In chronic kidney failure with diabetes, there is a decrease in urine, or an absence of urine, or an increase in the level of waste products in the blood as indicated by increased creatinine or urea levels in the bloodstream. Blood loss and protein loss in the urine can also signal kidney insufficiency or failure.
Two kinds of diabetic kidney disease
There are two kinds of diabetic kidney disease. The type that you may have is related to the amount of protein that is found in your urine. The two kinds of diabetic kidney disease are:
- Microalbuminuria: also called incipient nephropathy, the amount of urine that ends up in the urine is between 30 and 300 mg/day. It may stay at the same level, get better with treatment, or progress to macroalbuminuria.
- Macroalbuminuria: also called proteinuria or overt nephropathy, the amount of protein that ends up in the urine is greater than 300 mg/day. This condition cannot be reversed, and will progress to ESRD (End Stage Renal Disease)
In renal failure, increased fluid in the body leads to increased swelling. This is due to the kidneys effect on salt and fluid levels in the body. When they are not working properly, they cannot regulate blood pressure effectively. High blood pressure also affects the kidneys adversely, and can lead to failure. Acid levels in the bloodstream rise, as do potassium and phosphorus levels. Blood calcium levels are decreased.
Due to a decrease in blood calcium levels, bone health suffers and the patient is anemic. There is also an increased risk of cardiovascular disease with chronic renal failure. At the point when kidneys fail, dialysis becomes necessary for life.
Causes of renal failure
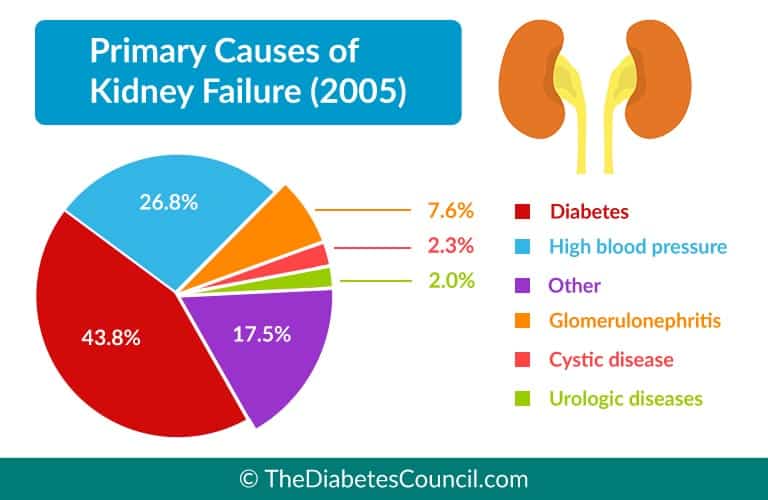
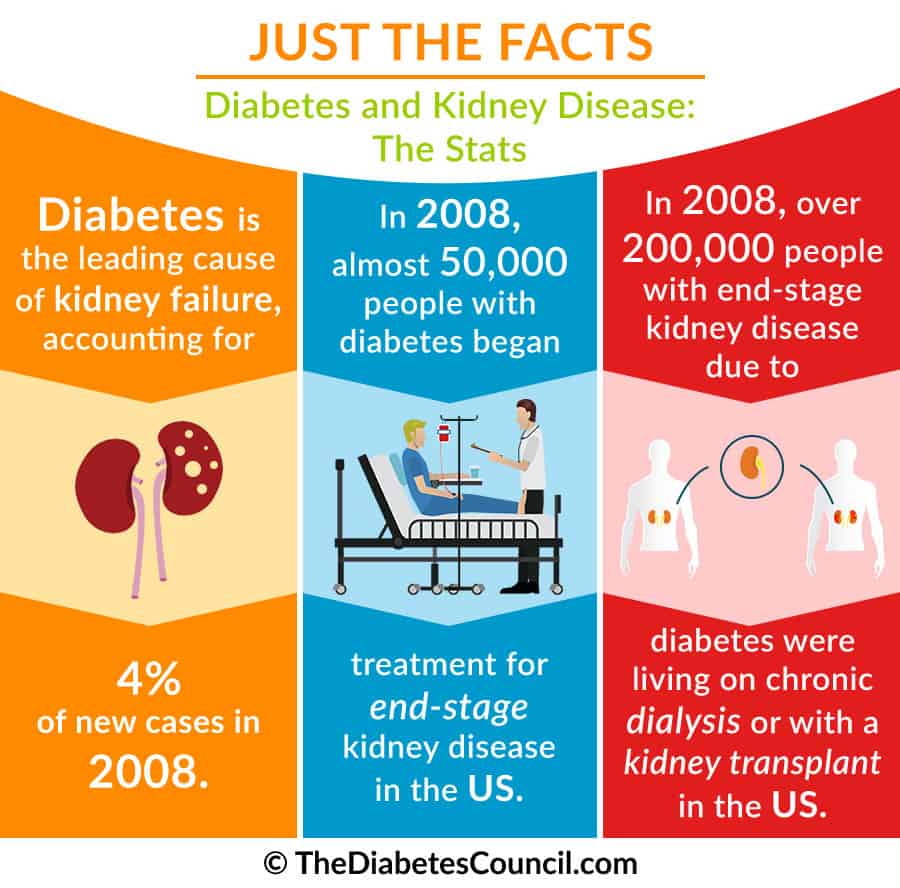
As we have said, diabetes is the cause of renal failure in almost half of all cases. From the chart below, we can see that the most prevalent cause of kidney failure is diabetes, followed by high blood pressure, glomerulonephritis, cystic diseases, urological diseases, and other factors.
How many people with diabetes actually get kidney failure?
From a study of veterans, we can see the prevalence of renal disease in those with diabetes is largely male and Caucasian. When looking at ESRD (End Stage Renal Disease) associated with diabetes, the prevalence was higher among males, and higher among those of the black population.
44,671 (10.7%) of the 415,910 veterans with diabetes had a diagnosis of any renal disease. With the average age of 67 years, about 98% were male and 60% were of white ethnicity. The prevalence of diabetic nephropathy was 6.0%. ESRD was present in 4.2% of subjects. ESRD caused by diabetes-associated prevalence was higher amongst black compared to white veterans and male compared female veterans.
Symptoms of chronic renal failure
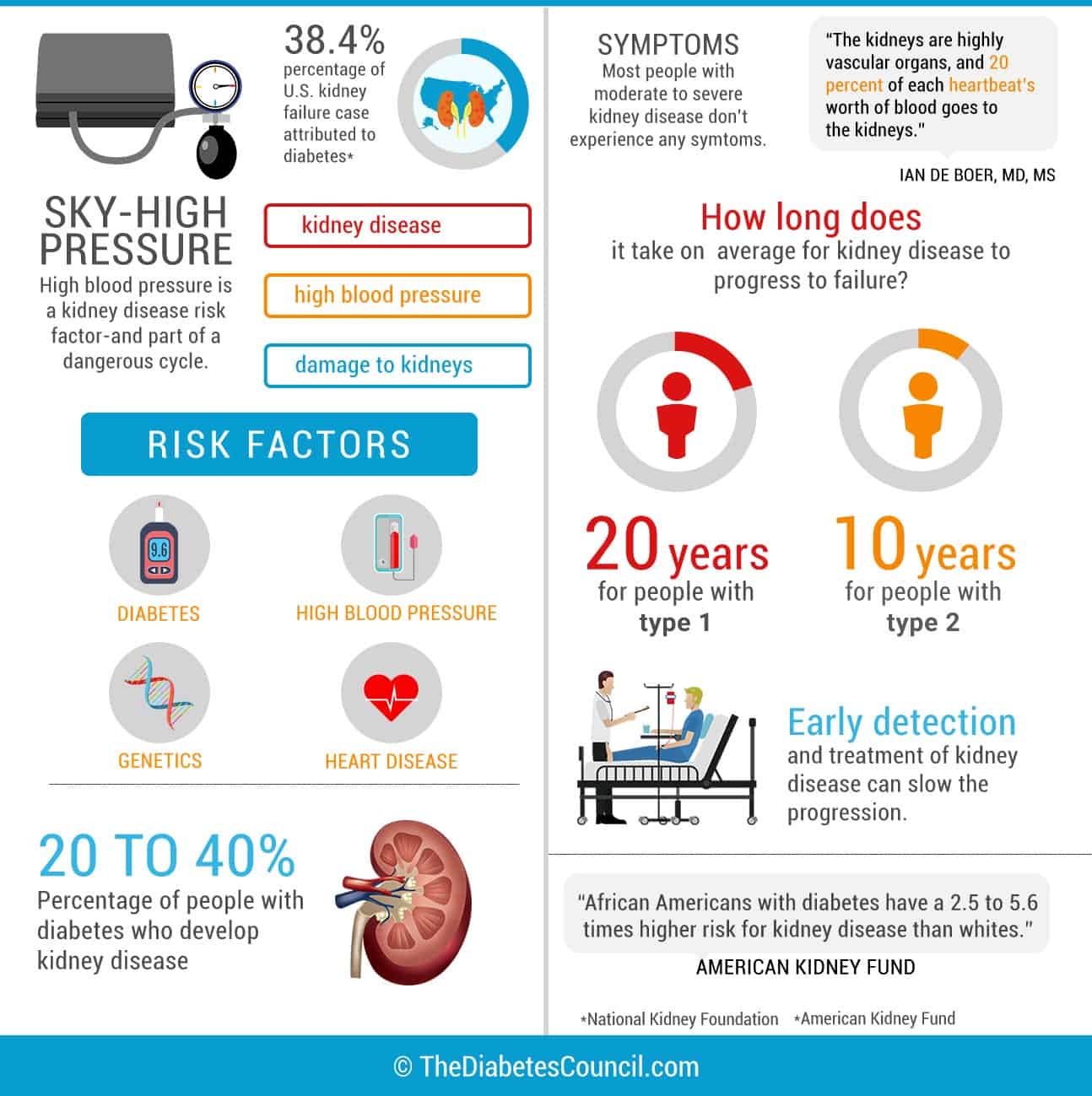
In the early stages of renal failure, most people don’t feel any different. The lack of symptoms makes yearly screenings very important at detection and treatment of early renal failure. You can lose half of your kidney functioning and still not know it. Once the disease progresses further, the first sign is swelling in the hands, face, feet or ankles. In addition, increased protein in the urine can make the urine foamy.
Other symptoms that present themselves with chronic renal failure are listed in the image below:
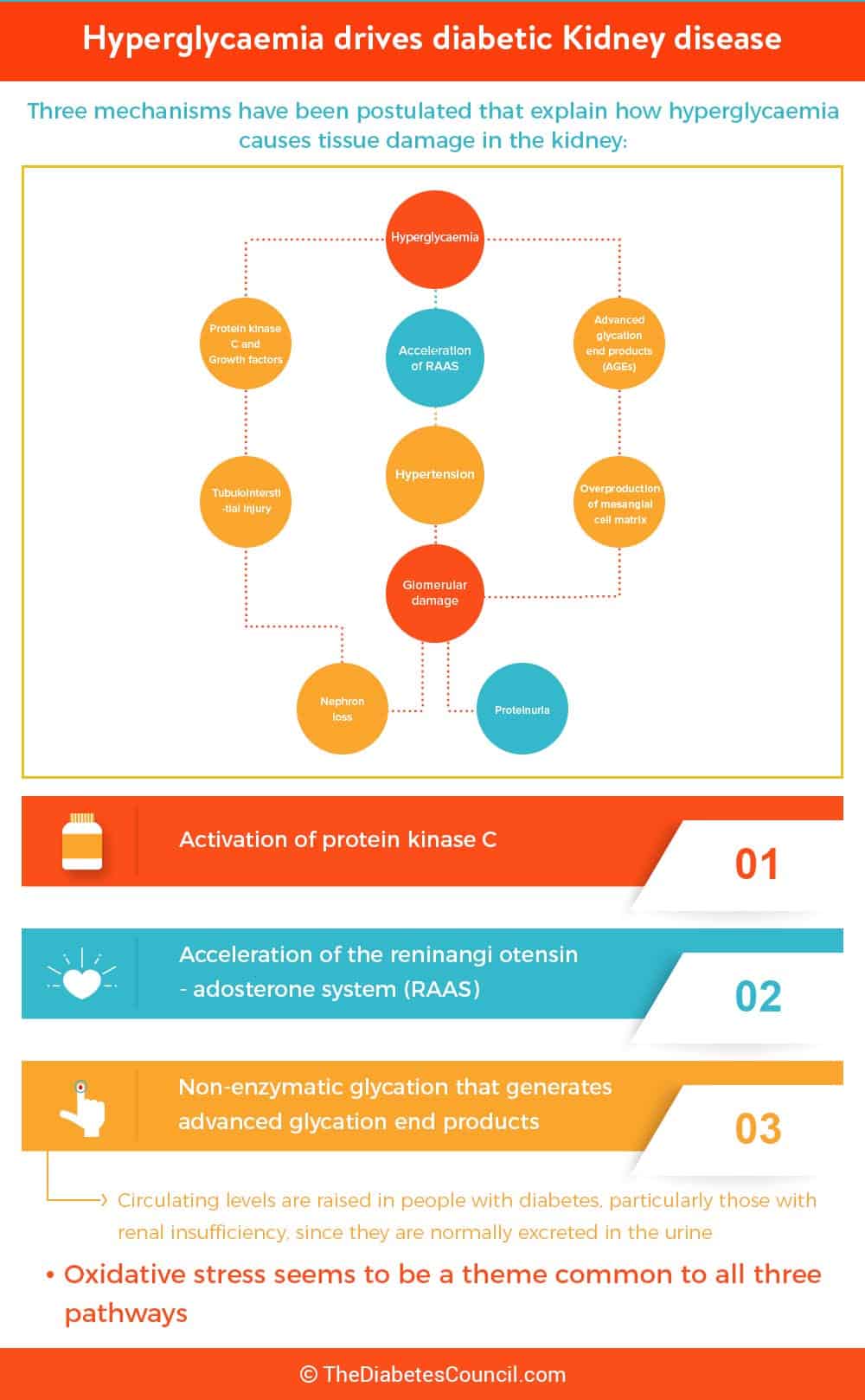
How does diabetes affect the kidneys, and can diabetes cause renal failure?
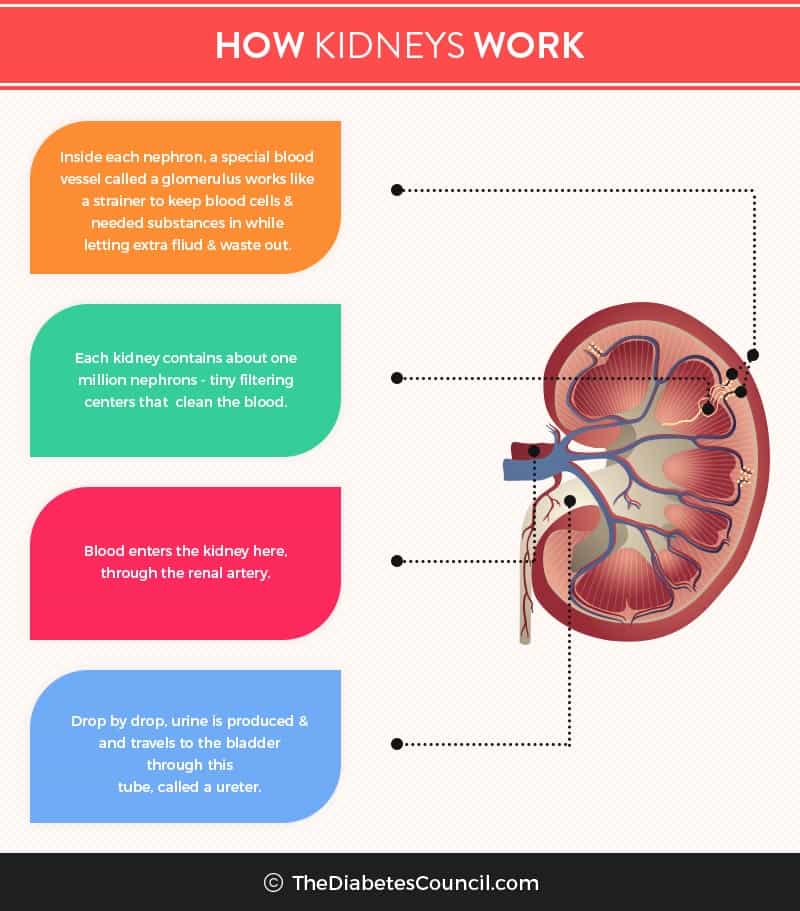
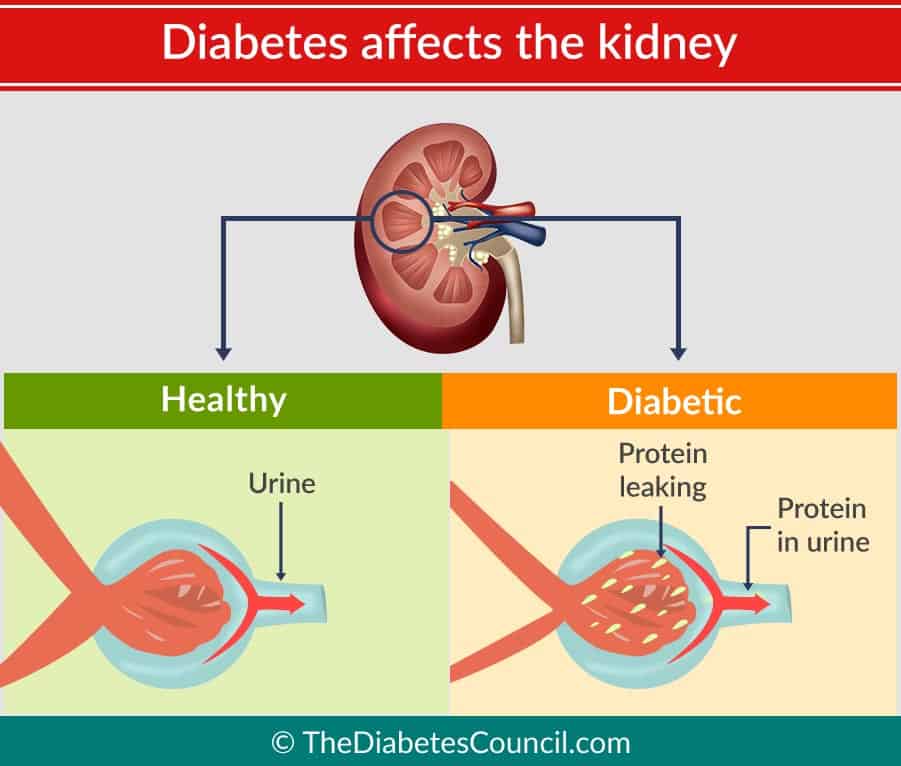
Without a doubt diabetes affects the kidneys adversely and can cause renal failure. We have seen that it is the number one reason that a person has renal failure. When we digest our food, the body turns the food into waste products. The kidneys, having many tiny holes in them, act as a filter for the waste products. Normally, protein and red blood cells are too large to pass through the million filters in the kidneys.
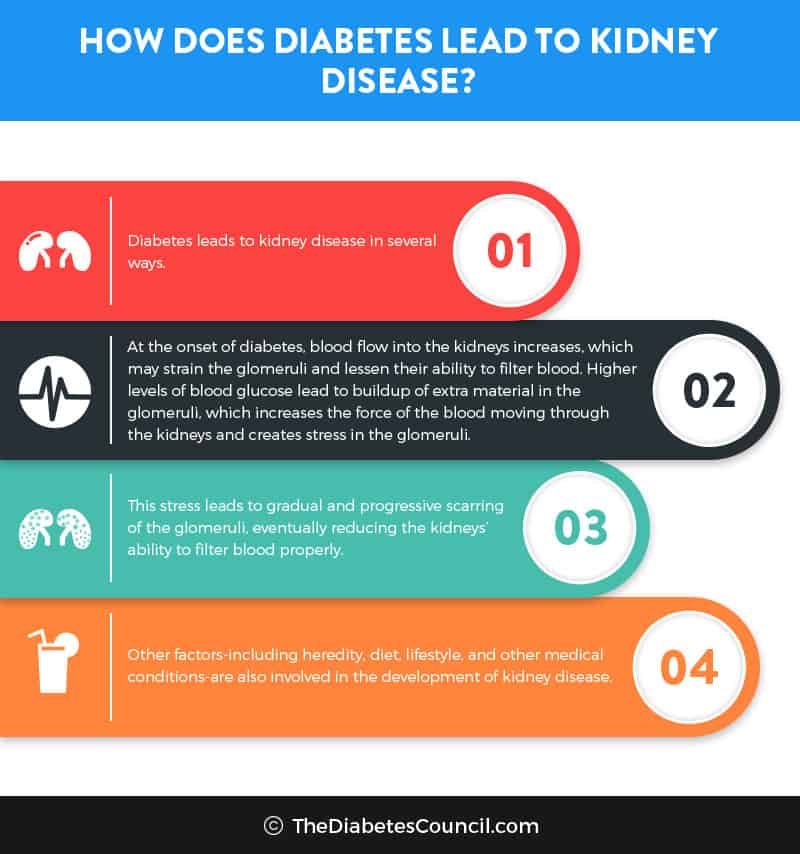
When a person has diabetes, they damage their filtration system. High blood sugar causes the kidneys to filter the blood excessively. This is due to diabetes causing the rise of chemicals that are found in the kidneys that cause the glomeruli to leak and let the protein through. The filters get clogged up and wear out eventually. They can start to leak after many years of this. That’s when you start to see protein and blood when testing urine.
Elevated blood glucose causes proteins in the kidney’s glomeruli to link together. When these proteins link together, they can cause scarring within the kidney. When the glomeruli get “scarred,” this condition is called glomerulosclerosis. It takes many years for this condition to develop, and these scarred tissues gradually take over the whole kidney and all of the tissue. As this occurs, the kidneys are unable to perform their function of removing waste products from the body.
Did you know
What about Lydia?
By identifying Lydia’s microalbuminuria, the doctor may be able to offer treatments to keep Lydia’s kidney disease from getting any worse. That is, Lydia may be able to keep her kidneys from getting worse by following her doctor’s advice. She will need to start to better self-manage her condition.
Still, even with controlled diabetes, a person with diabetes can suffer a kidney damage despite efforts at self-management. That doesn’t mean that she shouldn’t self-manage. There are many reasons to self-manage your diabetes, not only to protect the kidneys, as diabetes can affect every organ in the body.
Lydia should start measures to protect her kidneys now, and not wait until she has “macroalbuminuria,” (large amounts of protein in her urine). If she were to wait until she had macroalbuminuria, Lydia would likely move on to End Stage Renal Disease (ESRD), the dialysis center, and the kidney transplant list.
Other ways that diabetes damages the kidneys
Not only can diabetes damage your kidneys by disrupting the filtration system that they provide for the body, diabetes can also damage the nerves that signal your bladder is full. This pressure can damage the kidneys. Urine that stays stagnant in the bladder for too long a time puts a person at risk for Urinary Tract Infection (UTI).
What can you do to prevent diabetes from damaging your kidneys
Yearly screening for kidneys
- Microalbumin or ACR (albumin/creatinine ratio) urine test
Besides practicing good self-management skills and keeping your A1C below 7 percent, you should also get annual screenings to make sure that diabetes is not damaging your kidneys. A microalbumin test should be done on diagnosis of diabetes, then yearly. The laboratory will need to get a urine specimen to perform this test. If you do have protein in your urine, your doctor may want you to see a Registered Dietician to discuss reduction of salt and protein in your diet to help keep your kidneys safe. A value less than 30 is considered normal. In other words, you don’t have much protein spilling into your urine. This is a good thing.
- Glomerular Filtration Rate
The estimated Glomerular Filtration Rate (eGFR) should also be done to make sure your kidneys are working like they should. Less than 60 ml/minute can signal kidney disease. A GFR should be done on diagnosis, and then yearly (unless there is kidney damage, in which case GFR is done more often).
Other measures to prevent kidney damage from diabetes
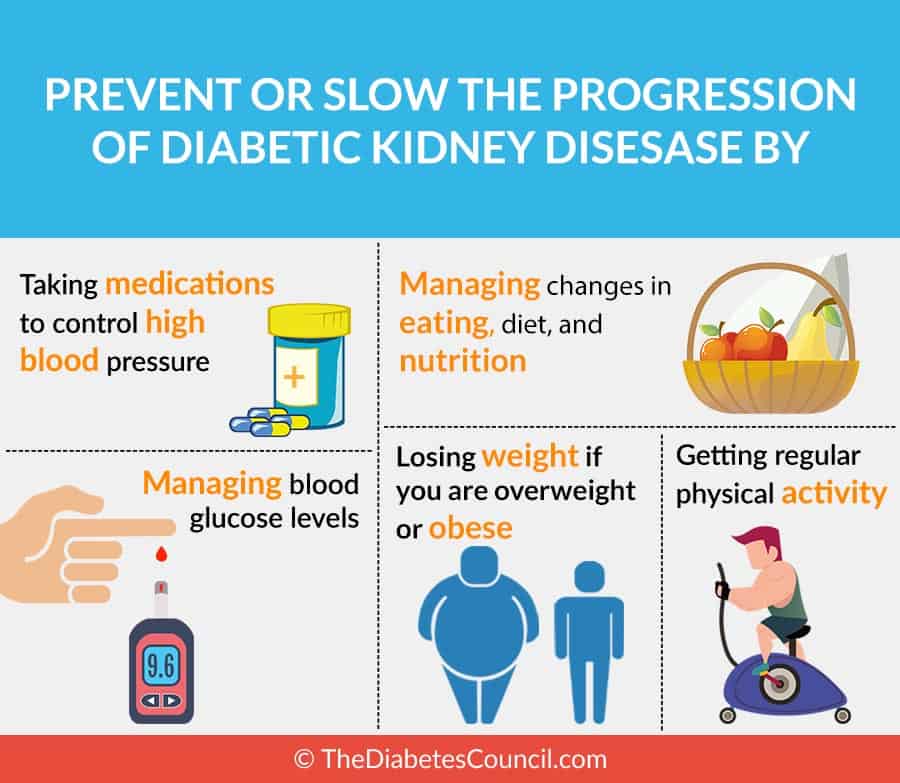
- Keep your blood glucose and A1C in target
As always, self-manage!!! Keep your A1C and your blood glucose in a target range. For most people with diabetes, the A1C should be less than 7 percent. Fasting blood glucose targets are now at 80-130mg/dl, and 2 hours after the start of a meal, your blood glucose should be less than 180 mg/dl. Your doctor may set different targets for you, depending on your age and other health factors. Speak with your doctor about what your targets are for these important numbers.
- Quit smoking
This is a given. If you have diabetes, you are worsening your condition if you smoke. Diabetes affects the circulation, and cigarette smoking also damages the circulation. Nicotine binds with oxygen in your blood stream, and keeps oxygen from getting to body tissues. This worsens circulation. Contact the Quit Line in your state. Most offer nicotine patches, gums, or lozenges to help you quit. Quit Lines also have counselors that can talk you through a rough patch, or give you tips on how to quit.
- Keep your blood pressure controlled
For most people with diabetes, a goal for blood pressure is below 130/80. Talk to your doctor if you are not sure what your personal target is. Make sure to take your blood pressure medication as prescribed. Your doctor puts you on these medications to protect your kidneys from damage, so it is important that you take them.
- Keep your blood cholesterol controlled
All of your cholesterol numbers should be in target. Especially focus on your LDL cholesterol (low density lipoproteins). These are the bad fats. You will want to keep your value for this lab result at less than 100. This means that you don’t have so much of the bad fats floating around in your blood stream that can cause plaque to build up in your arteries and damage your kidneys.
Increasing the good fats or HDL (High density lipoprotein) is also important. Eating more foods with “good fats” in them helps to elevate this number above 50. You can get this lab result above 50 by eating more foods that contain “good,” monounsaturated fats such as found in olive oil, avocados, nuts such as almonds, and the like.
- Stay active
Aim for 30 minutes of physical activity most days. Walking is a great exercise, and most people can do it without injury. Other forms of aerobic exercise include swimming, bicycling, and running. Don’t forget strength training 3-4 times per week! Speak to your doctor about your activity level, and what is appropriate for your condition.
- Eat healthy foods
Follow your diabetes meal plan, pay attention to protein portions, and watch salt (sodium) from the salt shaker, to processed meats and other processed foods, and from restaurants.
- Avoid medications that can damage the kidneys
Avoid NSAIDS (Non-steroidal anti-inflammatory Drugs) such as ibuprofen or naproxen. Make sure that you ask your doctor before taking any herbal supplements due to they may harm your kidneys.
What happens to kidneys if you don’t control your diabetes?
High blood glucose is responsible for all of the long term complications of diabetes. It’s no different with kidney failure. Keeping your A1C and blood glucose at bay, along with your blood pressure and cholesterol, will help you to avoid kidney damage or failure.
Is there a difference between Type 1 and Type 2 diabetes course of renal failure?
A research in Diabetologia on October of 1993 showed the comparison between the course of ESRD for those with Type 1 and for those with Type 2 diabetes. In the research, they found that:
- there was a higher mean glucose level in the first 10 years after diagnosis for Type 1s
- Type 1s had a lower systolic blood pressure
- The duration of diabetes prior to ESRD was longer for Type 1s than it was for Type 2s
- Type 1s were more likely to have other microvascular complications of diabetes such as retinopathy, gastroparesis, or neuropathy
- Type 1s were less likely to have cardiac disease and Congestive Heart Failure (CHF)
- Stroke and vascular surgery rates were similar
- Type1s and Type 2s both had equal likelihood of having a first degree relative with high blood pressure
Diet for renal failure
If you already have chronic renal failure, your doctor or dietician will want you to start on an eating plan called the “Renal Diet.”
Your kidneys are damaged; therefore, your kidneys cannot handle a regular amount of protein as they could in the past. Your kidneys also can’t handle excessive amount of salt or potassium, due to the kidney’s role in regulating these electrolytes. If you choose not to decrease your protein, sodium, and potassium levels, it makes your kidneys work harder to filter waste, and you will experience ESRD sooner. A renal diet is lower in protein, fat, sodium or salt, and potassium. You will most likely be asked to:
- cut back on protein containing foods, especially animal products such as milk, eggs, and cheese
- eat a low fat diet that is also low in cholesterol, as your body cannot handle high cholesterol foods like it used to, and you will get plaque build-up in your arteries from all of the excessive cholesterol in your bloodstream
- avoid high salt or sodium in your diet, and keep sodium to 1500 mg/day to keep your blood pressure in a better range to protect your kidneys (canned foods, frozen dinners, processed foods and meats)
- avoid excess potassium since your kidneys can no longer regulate this electrolyte. Potassium keeps your heart beating regularly and helps your muscles to work right, but kidney disease may result in high potassium levels, an irregular heartbeat, or even cardiac arrest. Avoid foods like apricots, oranges, potatoes and bananas, which are all high in potassium
Stages of Kidney failure
The five stages of chronic kidney disease are mainly based upon the Glomerular Filtration Rate, or GFR. The first stage is essentially no kidney damage, and the second stage is minimal damage. The following graph shows a detailed description of the five stages of chronic kidney disease:
| Stage of CKD | GFR Range | Description of Stage | Stage of treatment |
| Stage 1 of CKD | 90+ | Kidney function is normal, but urine findings, abnormalities of structure, or genetics point to CKD. | Control of blood pressure, risk factors, and observation. |
| Stage 2 of CKD | 60-89 | Kidney function is mildly reduced, other findings point to CKD. | Control of blood pressure, risk factors, and observation. |
| Stage 3A of CKD
Stage 3B of CKD |
45-59
30-44 |
Kidney function is moderately reduced. | Control of blood pressure, risk factors, and observation |
| Stage 4 of CKD | 15-29 | Kidney function is severely reduced. | Planning for ESRD. |
| Stage 5 of CKD | Less than 15 or on dialysis | End Stage Renal Disease (ESRD) or renal failure | Choices of dialysis or transplant, or both. |
Gestational diabetes and renal failure
Pregnancy puts a great strain on the body, and kidney disease for pregnant women with gestational diabetes can and does occur. Proteinuria in late pregnancy presents a problem. Women with diabetes prior to becoming pregnant who have intact renal function seem to have little problem. In other words, going into the pregnancy, they have no pre-existing kidney damage.
Those with diabetes prior to pregnancy who go into the pregnancy with already impaired renal function do not fare as well. They are at risk for decline of renal function during pregnancy that causes permanent damage. Preeclampsia with increased blood pressures further compensates the kidneys of the diabetic mother.
What is End Stage Renal Disease?
When a person enters stage 5 of renal disease, they have what is termed as “End Stage Renal Disease” or ESRD. The kidneys are severely damaged at this point. There is then a choice of dialysis or kidney transplant, or both.
What happens when you enter ESRD? Is there treatment?
When kidneys fail and no longer do their job to filter waste products from your body, there are two options for treatment. A person can either go to regular dialysis sessions, or they can have a kidney transplant. Often times they have both. They will be on dialysis while on the kidney transplant list waiting to have a match and kidney donated to them.
Two treatments for ESRD
Your treatment options for ESRD are:
Dialysis
When your kidneys don’t work, you need a machine or apparatus to do the job your kidneys used to do, and that machine is a kidney dialysis machine.
There are two types of kidney dialysis:
Hemodialysis
If you need hemodialysis, this kind of dialysis circulates your blood through a machine that has a filter with tiny fibers called “dialyzers.” You will be in a hospital bed or in a chair, and they will hook you up to the machine by accessing a “hemodialysis graft.” You will have to watch how much liquids you drink, and a registered dietician can tell you what your fluid intake should be daily. Fluids can raise your blood pressure during hemodialysis. Then your heart must work much harder. This is the reason for fluid restrictions during dialysis.
Getting prepared
Before you go on hemodialysis, you will first need an access to your bloodstream. Needles will be put into the access in order to draw your blood out of your body, remove waste products from your blood, and put your blood back into your body. This may involve an overnight hospital stay, or an outpatient procedure. There are three types of access that are used for hemodialysis. They are:
- Dialysis fistula
A specialized surgeon will use your own blood vessels to make a fistula. They usually connect an artery to a vein in your arm. More blood flow makes the vein grow large and get strong. Then it can be used to insert the dialysis needle. After the surgery, you will have to wait several weeks for the graft to heal before it can be used. This is the best method for accessing the bloodstream in order to perform dialysis.
- Dialysis graft
If the surgeon chooses to do a graft, the vein and artery are connected by a tube. The main benefit here is that it can be used sooner than a fistula can. Infections and clotting problems are more common with a graft.
- Catheter for temporary access
When kidney disease progresses rapidly, there may not be any time for a permanent access to your bloodstream to be established. That’s when they will put a catheter made of soft material into a vein. It can be located in your neck, your chest, or your leg near the groin area. This access will only be temporary; however, some patients do use a catheter for long term access also. If you will need the temporary access for longer than three weeks, then they will most likely place it under the skin. This helps to improve comfort level, and to reduce the risk of complications such as infection of the temporary access site.
Peritoneal dialysis
In speaking with your doctor, you can decide if peritoneal dialysis is a better choice for you. In peritoneal dialysis, the patient’s belly is used as a natural filter to remove waste products. A cleaning solution called a “dialysate” is used. This form of dialysis keeps you out of the dialysis center, because it can be done anywhere. This allows a person on dialysis to perform regular activities of daily living more readily. They may even be able to work or travel if they use peritoneal dialysis.
There are two types of peritoneal dialysis that are commonly used.
They are CAPD (Continuous Ambulatory Peritoneal Dialysis, and CCPD (Continuous Cycler-assisted Peritoneal Dialysis.
Discuss options with your doctor to see which one may be the right choice for you.
What about a kidney transplant?
Dialysis saves lives for those with chronic kidney failure, but it serves to provide only about ten percent of a normally functioning kidney’s ability to filter wastes from the body. In addition, dialysis can cause other serious health issues including:
- anemia or decreased number of normal red blood cells
- nerve damage
- infection
- cardiac disease
- high blood pressure
Longer life with a kidney transplant than without one
It should be noted that the average life expectancy of someone on dialysis is only five years. Research has tended to favor a transplant over long term kidney dialysis. Transplant patients generally live longer than dialysis patients.
You will go through a major surgery, with a long recovery period. There is a possibility of transplant rejection. However, after the organ transplant, you may have more energy, fewer diet restrictions, and an overall better quality of life. Patients have fewer complications to report.
If you obtain your kidney for transplant from a living donor, you can expect to live anywhere from 12 to 20 years. If your kidney came from a donor who is deceased, then you can expect to be around for the next 8 to 12 years. If you can manage to have a kidney transplant before you end up on dialysis, then you could live 10-15 years longer than someone on dialysis.
It’s possible that you may have to be on dialysis for a time while waiting on an organ for transplant. They will need to locate a good match for you whether it is from a deceased donor or from a living donor. This is due to being on dialysis for a long time can shorten the life of a new kidney after the transplant. Still, a transplant is preferred in most cases over dialysis.
If you are not to the point where you need dialysis, but you know that your kidneys are indeed failing, you may want to look into Pre-emptive Transplantation. This is defined as a transplant prior to beginning on dialysis, for the best results possible. Quality of life is better with this method, and life expectancy is increased over those on dialysis. This type of transplantation is doubly beneficial for those with Type 1 Diabetes. A pre-emptive transplantation almost always uses a kidney from a live donor.
For more information and frequently asked questions on pre-emptive transplantation, go to: http://www.bidmc.org/~/media/Files/Centers%20and%20Departments/TransplantInstitute/preemptfaq.pdf
Live vs. deceased donor
A live donor is preferred in all cases because of improved kidney graft functioning, among other things. It is definitely the preferred method for pre-emptive dialysis as mentioned above. Still, no matter how long a person has had to be on dialysis, they are better off with a transplant organ from a live donor.
Transplant list
To get a kidney transplant, you will need to get on the kidney transplant list. To find a transplant center in your area, you may visit the Organ Procurement and Transplantation Network (OPTN) website. Select "Transplant Centers by Organ" for Member Type, then select “Kidney” for Organ Type, then select your state. Choose a transplant center that best fit your needs. Discuss with your doctor, and be prepared to be on a waiting list until a suitable organ donor is found.
You will likely have a transplant team to evaluate you right from the beginning. They will help you decide which treatments are right for you.
Need more information?
You can receive free booklets from The National Kidney Foundation that will provide you with information on diabetes and kidney disease. The national toll free number to request free information from NKF is (855)653-2273.
You may also browse the NKF store at www.kidney.org/store .
Over to you
We hope that you have learned something about diabetes and kidney disease, as I have in researching and writing this article. If you have diabetes and have had renal failure, and would like to share your experience with us, please do so in the comments section below. If you have experience being on dialysis, also share if you will! If you have managed to keep your kidneys healthy with diabetes, we would love to know how you have managed to do it. If we left anything out, please let us know!!!
References
- https://www.kidney.org/atoz/content/diabetes
- http://www.diabetes.ca/diabetes-and-you/complications/kidney-disease
- http://www.renal.org/information-resources/the-uk-eckd-guide/ckd-stages#sthash.B4tM9ld4.35jidPB6.dpbs
- https://www.ncbi.nlm.nih.gov/pubmed/21266265
- https://www.niddk.nih.gov/health-information/health-topics/kidney-disease/kidney-disease-of-diabetes/Pages/facts.aspx
- http://patient.info/health/diabetic-kidney-disease-leaflet
- http://www.bidmc.org/Centers-and-Departments/Departments/Transplant-Institute/Kidney/The-Benefits-of-Transplant-versus-Dialysis.aspx
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetes-and-kidney-failure
- http://www.diabetes.org/living-with-diabetes/complications/kidney-disease-nephropathy.html
- http://www.diabetes.org/living-with-diabetes/treatment-and-care/transplantation/
- https://medlineplus.gov/diabetickidneyproblems.html
- https://www.uptodate.com/contents/pregnancy-in-women-with-underlying-renal-disease?source=see_link
- https://medlineplus.gov/creatinine.html
- https://medlineplus.gov/kidneytests.html
- http://www.medicinenet.com/diabetes_and_kidney_disease/article.htm
- http://www.webmd.com/diabetes/guide/diabetes-kidney-disease
- https://www.kidney.ca/diabetes-and-kidney-disease
- http://www.kidneyurology.org/Library/Kidney_Health/Kidney_Disease_of_Diabetes.php
- http://www.heart.org/HEARTORG/Conditions/More/Diabetes/WhyDiabetesMatters/Kidney-Disease-Diabetes_UCM_313867_Article.jsp#.WFWbLfkrKuU
- http://www.diabetesforecast.org/2016/mar-apr/renal-rules.html
- http://diabetes.diabetesjournals.org/content/55/6/1832
- https://www.kidney.org/atoz/content/Diabetes-and-Kidney-Disease-Stages1-4
- http://care.diabetesjournals.org/content/27/suppl_2/b45
TheDiabetesCouncil Article | Reviewed by Dr. Jack Isler MD on May 23, 2020