Gastrointestinal disorders occur more often in those with diabetes. In fact, at some point in their life, those with diabetes will develop a GI problem such as ulcers, gallstones, IBS or another GI disorder. Upwards of 75% of diabetes patients report to their doctors experiencing GI symptoms.
Overlooked or Misdiagnosed
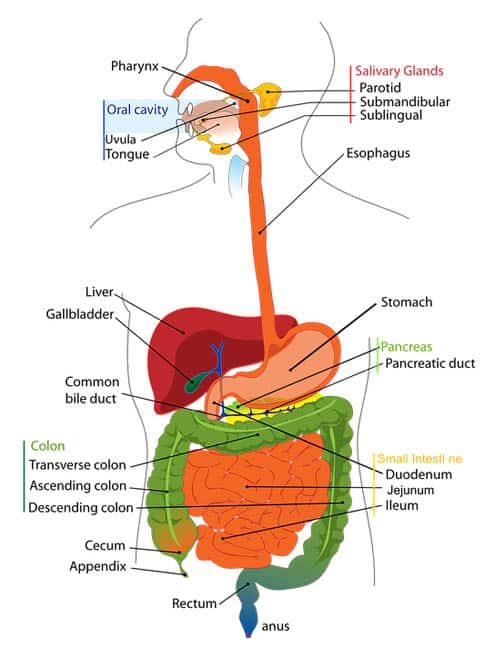
While many experience these symptoms the diagnosis is not always the same and oftentimes is misdiagnosed initially. The entire gastrointestinal tract can be damaged and affected by diabetes starting at the mouth to the esophagus all the way through to the anorectal area. Because of the complex nature of GI symptoms and the area of the gastrointestinal tract that they cover, this leads to issues in diagnosing and treating GI conditions in diabetes patients.
I advise reading the following articles:
Previously GI conditions were not associated with diabetes. This also lead to misdiagnosis, overlooked conditions or even improper treatments. New research has begun to suggest otherwise, which is leading to an increase in GI issues and conditions in diabetes patients.
Blood Sugar Control and its Correlation to Gastrointestinal Conditions
Acute and chronic periods of high blood sugar can lead to GI complications. And as with other diabetes complications, poor blood sugar control is usually associated with more severe GI issues. Those with retinopathy and neuropathy should be tested to check for GI conditions. Dysfunction in how the neurons supply the enteric nervous system in the body can lead to GI complications. Similar to how nerves in the feet lead to neuropathy, the body’s intestinal nerves can also lead to enteric neuropathy. This type of neuropathy is known as autonomic neuropathy which can lead to an abnormality in how the body secretes and absorbs nutrients. Damage to the intestinal nerves that inhibit or stimulate the motility of the intestinal system as well as its function can accelerate or decrease the rate of intestinal function.
Common GI Conditions in Those with Diabetes
While the GI tract is a complicated one and many people with diabetes can suffer from a variety of GI conditions, there are some more common ones that they are often diagnosed with. They include:
Gastroparesis
Gastroparesis is a condition where the process of emptying the food in the stomach is delayed which creates a retention of the contents in the stomach. People with gastroparesis often experience bloating, distention of the stomach, abdominal pain, vomiting and nausea. Foods that contain a high amount of fiber or fat are not tolerated by many people with gastroparesis and can lead to an increase in heartburn and reflux issues.
Diagnosing Gastroparesis
Many patients are diagnosed with gastroparesis based on their symptoms alone. However, additional testing is done to confirm this diagnosis. An upper GI endoscopy can rule out any obstructions in the stomach or the duodenum, but this test does not give an accurate picture of the gastric emptying process. To confirm ma delay in gastric emptying an upper GI barium study may be necessary.
Treatment of Gastroparesis
There are many different treatments of gastroparesis available to help provide a relief in symptoms as well as management of diabetes. Consuming more frequent small meals can help to provide patients with some relief. Avoiding high fat and fiber foods can help as well. Sometimes a liquid diet may be recommended and as symptoms begin to get worse alimentation and parenteral hydration may be necessary. During the most severe gastroparesis episodes a nasogastric tube suction may also be used. There are also medication treatments that help to facilitate the gastric emptying process for those with gastroparesis.
Candida Infections
Those with diabetes can develop yeast infections in their GI tract, especially when they have poor control of their blood sugar. A yeast infection in the mouth, is known as Thrush, which is characterized with a white coating on the tongue and the throat proceeded by pain and burning. If a yeast infection extends further in the GI tract it can lead to candida esophagitis. This can cause heartburn, difficulty swallowing and bleeding in the intestinal tract. Thrush or oral candida can be diagnosed by an examination, while candida esophagitis may require that an endoscopy is completed. Treatment for both is highly affective through oral antifungal medications to help eradicate the yeast infection.
Ulcer Disease
An acid irritation in the stomach or even the esophagus can create indigestion, heartburn and a burning sensation in the abdomen. Duodenal and gastric ulcers is caused by a specific bacteria known as Helicobacter pylori (H pylori). Treatment of ulcer disease works to suppress the gastric acid with ant secretory medicines. When H. Pylori is present antibiotics may be given as well. Those with gastro esophageal may require proton pump inhibitor treatment because the eradication of the H. pylori bacteria often times worsens their symptoms.
Enteric Neuropathy in the Small Intestine
The enteric nerve which supply the small intestine may be damaged through long term complications of diabetes. This damage can lead to abnormal secretion, absorption and motility of the intestine. Symptoms like abdominal bloating and diarrhea may occur. The delay in the emptying of intestinal fluids can also increase bacterial overgrowth. Broad spectrum antibiotics may be necessary to reduce the growth of bacteria in the small intestine.
Enteric neuropathy can also lead to chronic pain in the abdomen, similar to that of the peripheral neuropathy in one’s feet which can occur as a long-term complication of diabetes. Treatment of chronic enteric neuropathy includes pain medications and antidepressants.
Celiac and Diabetes Connection

Celiac is diagnosed with an endoscopic biopsy done of the small intestine as well as with an anti-gliadin and anti-endomysial antibodies lab test. The only treatment option available currently for those with celiac is to adhere to a strict diet that is gluten free. Celiac disease is commonly referred to as coeliac disease or gluten sensitive enteropathy.
Fatty Infiltration or Liver Disease
Fatty infiltration of the liver is common in those with Type 2 diabetes due to poor blood sugar control. Fatty infiltration can lead to elevated liver enzymes and abdominal pain. Sometimes, it can also progress into fibrosis and even cirrhosis.
Diagnosis can be made through an examination but must be confirmed with an abdominal ultrasonography or a percutaneous liver biopsy when necessary. Treatment options are geared towards the improvement of blood sugar control and a low-calorie diet.
Further reading:
Wrap-Up
Gastrointestinal problems in those with diabetes are unfortunately very common but not typically diagnosed in the medical practice. The duration in which a patient has had diabetes and their blood sugar control should be taken into consideration when GI symptoms occur. Because the entire GI tract can be affected, diagnosing and treating these conditions can be challenging. If you have been experiencing GI symptoms or issues you should speak to your doctor immediately to discuss the potential of GI conditions and what treatment methods may be available to help provide you with relief.
References:
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on May 24, 2020





