In this article, we will cover everything that you need to know about how to avoid an extremity amputation due to diabetes. We will cover skin and foot care, what to look for, and when to contact your doctor. We will discuss whether or not you need to see a podiatrist, and what to do if you do have a diabetic foot ulcer. We will look at how to get it treated, so that it heals and doesn’t progress to amputation.
We will also look at what to do if you are going to have, or have already had an amputation due to your diabetes. We will look at ways you can become mobile again safely. We will also discuss ways to protect your remaining limbs so that you don’t have another amputation later. We will discuss what to look for related to residual limb care, and how to locate needed resources, such as a physical therapist.
In my own experience as a nurse for 22 years, and as a certified diabetes educator, I have seen many people with diabetes lose functional mobility, and even their life, after an amputation. I have seen a person go from having a blister and not even knowing they have diabetes to having a below the knee amputation in under two weeks.
In addition, I have worked with people who have been through femoral popliteal bypass surgery, amputation of the toes, then a below the knee amputation. I have watched them come in and out of the hospital until they have an above the knee amputation. With cardiovascular disease, the risk of another amputation is very high.
I have watched their pain and suffering, and seen the struggles that their families go through after amputation due to complications of diabetes. I have sat up late with them, while they try to deal with phantom residual limb pain, as their mind plays tricks on them and they feel pain in the already amputated leg.
Roger’s story
To bring this devastating scenario home in your mind, the story of Roger tells it best. Roger is a 69 year old who has had Type 2 diabetes for the past 15 years. His A1C has always been a bit too high for comfort at 8 percent, and he prefers a Southern US diet of high fat and high carbohydrate, despite his diabetes education.
Roger stated he just has to have fried chicken, even though he knows he shouldn’t eat it so often, and he loves his sweet Southern tea. The only thing he loves more is his two year old grandson, Tyler. Tyler is a busy boy, and like most 2 year olds, he is into everything.
Roger still works in the fields for his son-in-law on the family farm. One night, he came in from a long day in the fields, and he took his work boots off. He sat them in the corner of the mud room where he always sits them, and went to watch the evening news.
The next morning, Roger got up and ate breakfast, showered and got dressed, and stepped back into his work boots. He worked all day, and came home again that evening and took his boots back off. His wife immediately noticed an angry looking sore on the bottom of his left foot. She asked him what had happened, and he said he didn’t know. You see, he hadn’t felt anything unusual.
His wife went to investigate, and looked in his shoes. In the bottom of the left shoe, just under where the new sore was on Roger’s foot, was a set of keys on a key ring. Roger had unknowingly walked on the set of keys all day, and he didn’t even know it. Tyler must have been getting into everything, and dropped the keys in Roger’s boots, his wife thought.
Roger had walked on the keys and had not felt it due to his diabetic neuropathy, a direct complication of his Type 2 diabetes. He now had a diabetic foot ulcer, uncontrolled diabetes, and was at risk of gangrene and subsequent amputation of his left limb. After a home health nurse came for a while, Roger was not healing.
Unfortunately, Roger did not heal, and later had a below the knee amputation due to a non-healing diabetes foot ulcer. Roger knows now to check his right foot every day, and to check his residual limb for signs of infection as it is still healing.
The moral of Roger’s story is to always practice daily foot care and checks. Always check shoes for foreign objects, and make sure footwear fits well, and does not pinch the skin. We will get into foot and skin care more a little later on. Let’s talk about some statistics related to amputations in the diabetic population.
Contents
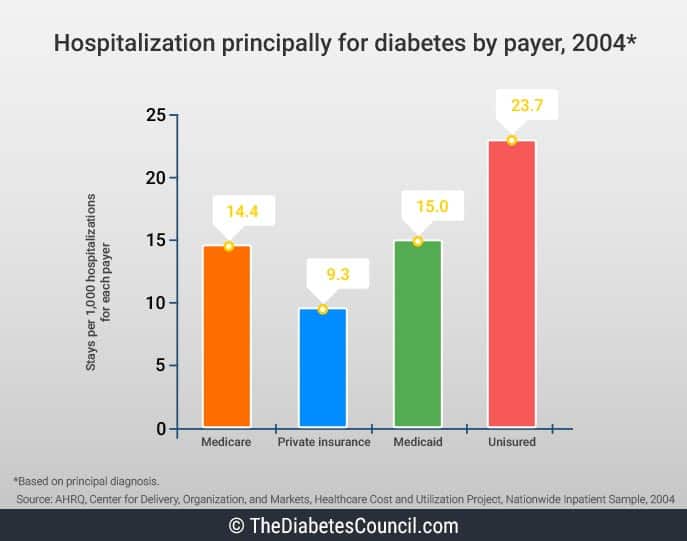
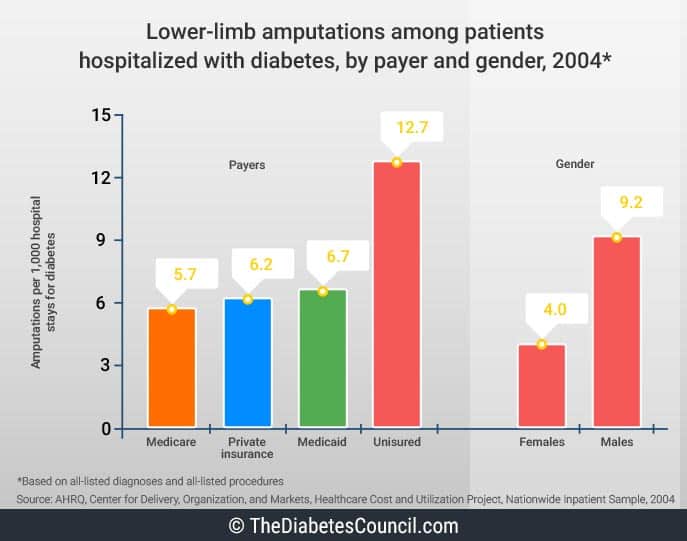
Over half of limb amputations (about 67 percent) in the United States are attributable to diabetes and related complications. The majority of limb amputations are performed on the lower extremities.
From 1980 to 2003, lower extremity amputations increased from 33,000 to 84,000 in 1997, and dropped back down to 75,000 amputations in 2003. In 2010, about 73,000 lower-limb amputations were performed in adults aged 20 years or older with diagnosed diabetes. As is easily seen, amputations are still a big problem for those with diabetes.1
I advise reading the following articles:
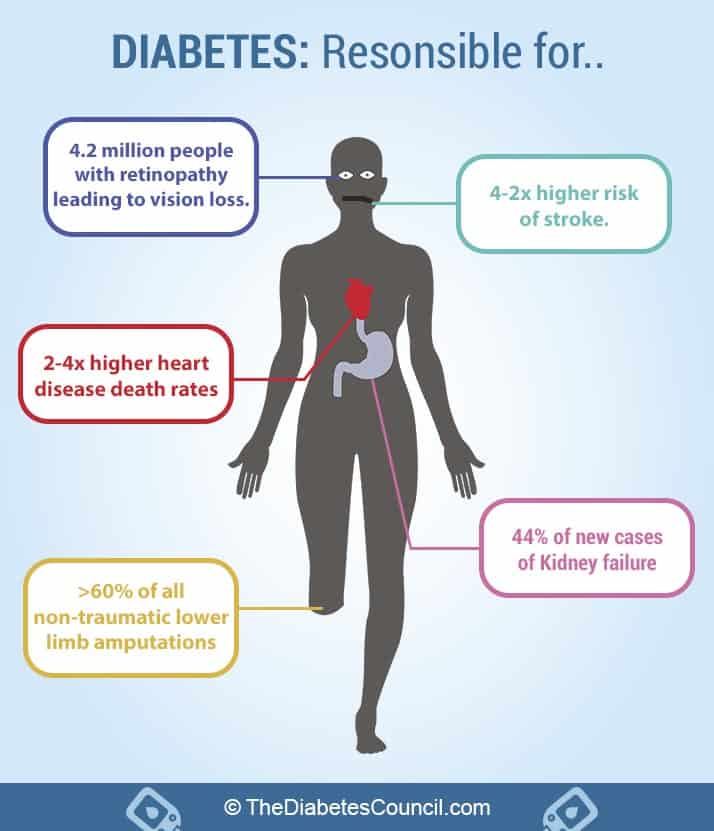
Diabetic neuropathy and subsequent damage to sensory nerves in the feet contribute greatly to deformities and ulcers, thereby increasing the risk for amputations if left untreated. For those under the age of 65, 3.9 of 1000 people with diabetes had an amputation. From age 65 to age 74, the incidence increased to 6.6 per 1000. For those over the age of 75, amputation occurred at a rate of 7.9 per 1000.
Rates were 50 percent higher for men than women. The elderly have more amputations, as do the non-Hispanic black population. The rate for amputations for people with diabetes is 28 times higher than for people without diabetes.
These statistics are alarming when compared with the CDC estimate that 23.6 million Americans currently have diabetes, a number that is up from 18.2 million in 2003. No wonder a cornerstone of diabetes self-management and education is foot care.
The cost of amputations is high, financially and emotionally. We don’t want you to experience the pain and suffering of an amputation due to your diabetes, so let’s get started on the way to happy and healthy feet by learning how you can avoid an amputation!!!
Types of diabetic foot amputations and rates per 1,000 people
People with diabetes can have 4 different kinds of amputations of the lower limbs, or legs. Per 1,000 people, 2.6 have an amputation of the toe, and 0.8 have an amputation of the foot. 1.6 will have a below the knee amputation, and 0.8 will have an above the knee amputation.
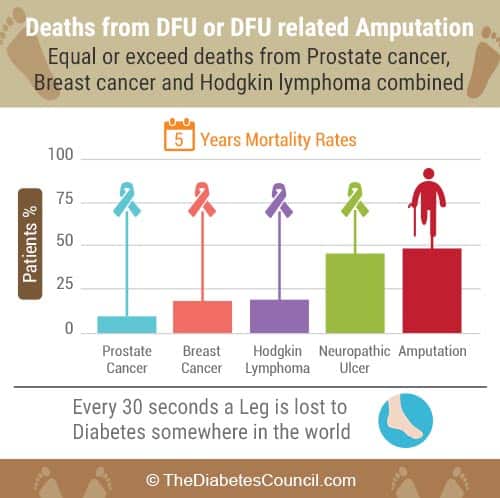
Far fewer, but some, will have amputations of fingers, hands, or even arms. Extremity amputations equal loss of functional mobility, and decrease the quality of life, and life expectancy for a person with diabetes. Of those ages 20 and older, people with diabetes have the most non-traumatic amputations of any group.2,3
What causes people with diabetes to have more amputations?
Let’s look at some of the factors that make it more likely for a person with diabetes to end up with an amputation. For starters, some of the factors that contribute to amputation for diabetics are…
- Nerve damage or diabetic neuropathy causes decreased feeling, and a person with diabetes cannot feel it when they get a tack in their foot, or injure their limb
- Skin changes from diabetes causes skin to break down, and this combined with diabetic nerve damage and poor circulation leads to non-healing ulcers
- Calluses form on the feet
- Ulcers develop that are non-healing
- Poor Circulation, including Peripheral vascular and arterial disease, contributes to problems with healing
- External factors that we can control, like whether or not we smoke, can have a big effect. Smoking increases the risk of diabetic non-healing ulcers and subsequent amputation
- Prolonged high blood sugars (uncontrolled diabetes) causes complications of diabetes, including nerve damage (neuropathy), and poor circulation
- High blood pressure uncontrolled over time will contribute to the development of non-healing ulcers and subsequent amputation
- When nerve damage and circulation is poor, infection can set in, and once the wound bed is gangrenous, amputation is required
Let’s break a few of these reasons for amputation down a bit further…
Why do people with diabetes have more amputations?
It is true that people with diabetes can be plagued with a whole host of skin and foot problems related to Peripheral Arterial Disease (PAD), and to diabetic neuropathy, or nerve damage that occurs from years of high blood sugars. A small nick in the skin can lead to a non-healing ulcer which can quickly turn to gangrene and necessitate amputation.
Neuropathy and PAD, oh my!
Patients with neuropathy get a “pins and needles,” burning pain in their fingers and toes. This numb feeling makes it difficult for people with diabetes to feel pain. People with diabetic neuropathy can injure their foot and not even feel it. On top of that, poor circulation, and changes in the shape and anatomy of the foot make it more likely for a person with diabetes to injure their feet or hands. Like Roger, you can get an injury and be unaware of it until it is too late.
Neuropathy, when it leads to foot malformation such as Charcot’s foot, makes it hard to find shoes that fit properly and don’t rub a blister. In this case, people with diabetes tend to stuff their feet into ill-fitting shoes and cause themselves more problems. They should be fitted for the appropriate diabetic shoes, which are custom therapeutic shoes made to fit and accommodate any foot deformities that may exist.
When neuropathy leads to loss of sensation, and injury of the extremities, infection can ensue. This is why neuropathy is one of the main reasons for amputation.
Charcot’s Foot
Charcot’s foot is one condition that can develop related to diabetic neuropathy. There is a significant loss of the ability to feel trauma, temperature, and pain. The patient injures their foot, as they continue to walk. This results in worsening of the injury. People with a tight Achilles tendon are at increased risk of developing Charcot’s foot deformity.
Weakening of the bones with Charcot’s foot occurs with progressive bone damage, and bones can fracture due to this weakness.
The foot changes shape and takes on a “rocker bottom” look. This severe deformity can lead to amputation. Symptoms include the foot is warm to the touch, there is redness, swelling, and pain in the affected foot.
Prevention is key in relation to Charcot’s foot, which includes good diabetes self-management practices to prevent neuropathy. Regular podiatrist check-ups should occur, and a person with diabetes should practice appropriate foot care and prevent injury of their feet.
If diagnosed, a series of x-rays may be used. For treatment, in the early phases, Charcot’s foot will be immobilized. The patient will be non-weightbearing to help the foot to heal from any fractures that may have occurred. The patient may be fitted with a cast or brace, or may be given crutches or a wheelchair to use during convalescence.
Custom shoes with special inserts may be ordered. Activity level is modified to prevent further injury to the foot. At any rate, Charcot’s foot puts a person with diabetes at further and greater risk for amputation.
Callouses, corns, warts, and foot ulcers beware
A person with diabetes would also benefit from therapeutic shoes if they have excess callouses on their feet. Thick callouses can break down, and turn into non-healing foot ulcers. These, unpleasantly, can lead to amputation.4
Bathroom surgery
Patients who try to remove their own callouses, warts, or corns by performing “bathroom surgery,” can give themselves a non-healing ulcer that later requires an amputation. This is why people with diabetes should never try to remove their own callouses, warts or corns. They also should not use any over-the-counter callous, wart, or corn remover products on their skin.
See a podiatrist
It is important when callouses, corns or warts are present, to have these issues addressed at a podiatrist’s visit. A podiatrist is a doctor who specializes in problems of the feet. They generally see many people with diabetes, and they can perform a Comprehensive yearly diabetes foot examination using a 10 mm monofilament, and treat many conditions of the foot.
A podiatrist can also trim thickened toenails, which is something a person with diabetes should not do on their own. They can order therapeutic shoes, therapeutic shoe inserts and check circulation. They may be able to pick up on problems with your feet that you would not otherwise be aware of.
Diabetes comprehensive foot exam
A comprehensive foot exam is done yearly, and includes assessment of present diabetes complications, such as neuropathy, nephropathy, retinopathy, peripheral vascular disease, and cardiovascular disease. Notes are made related to any prior amputations, history of an ulcer, or presence of a current ulcer. The examiner will assess for calf pain, changes in the feet since the last evaluation, and any problem with shoes.
The exam includes assessment of smoking status, A1C level, skin, and hair and nail condition. The examiner will look for thin, fragile, shiny and hairless skin when evaluating for circulation problems. Thickened, discolored, ingrown or infected toenails may signal a fungal infection.
The examiner will measure and draw the patient’s skin condition into a diagram, using a key to mark where pre-ulcers, ulcers, calluses, or bunions are, to name a few. They will note toe and foot deformities, including Charcot’s foot, and prominent metatarsal heads (protruding toes). They will also look for foot drop, and check for pulses in the feet, (the posterior tibial and dorsalis pedis pulses).
An important part of the examination is checking for protective sensation. The examiner uses a number 10 monofilament, which is like a small piece of fishing line to touch the patient in certain places on their foot while their eyes are closed. If the person can tell where the examiner touched them on the foot (ie: pinky toe), then the examiner will note that they have sensation in that area. In areas over callouses, the patient may not be able to feel the monofilament so well. The examination does not cause the patient any pain.
The examiner also assesses for the appropriate footwear that is fit properly. At this point, the examiner can order therapeutic shoes or foot inserts if necessary. If shoes or foot inserts are ordered, they are often covered by insurance, and it is best to get them at the podiatrist or orthoptist, as opposed to at the shoe store.
The podiatrist will teach the patient appropriate foot care. The patient should be able to demonstrate the foot care. Education related to A1C, and smoking cessation should also be done at this time, or planned for a later visit with a certified diabetes educator.
If vascular or laboratory studies are needed, the practitioner can order those for the patient, and make appropriate referrals to other providers as appropriate(RN foot specialist, CDE, PCP, endocrinologist, vascular surgeon, foot surgeon, rehabilitation specialist, pedorthist, or orthotist).
The examination can be performed by a Certified Diabetes Educator, a podiatrist, or an RN foot specialist, to name a few.
The good, the bad, and the ugly
When a person with diabetes has PAD, blood flow to the feet and hands is decreased, making the limb more susceptible to cuts and sores that won’t heal. If a cut or sore will not heal, and blood flow is poor, eventually gangrene sets in. When gangrene sets in, it is simply too late to save the affected limb from amputation.
After years of high blood sugars take its toll on nerve pathways, the end result is decreased feeling and sensation in the feet and hands. Simple injuries to the extremities may not be felt by the person with diabetic neuropathy. For these reasons, it is easy for a person with diabetes to get an injury or infection of the extremities that leads to an amputation.
The good news is that with good diabetes self-management, proper foot and skin care, and with daily checks to skin and feet, amputations can largely be prevented. The following are some things that you can do in order to prevent a non-healing ulcer or other injury to your extremities, and ultimately prevent an amputation. Let’s take a look…
- check your feet (and hands) every single day if you have diabetes
- at the first sign of any problem with your extremities, see your doctor or healthcare provider
- check in to getting special shoes that may be covered by Medicare or other insurance companies
- always follow your doctor or healthcare provider’s advice if they prescribe a treatment for a non-healing ulcer
- if you have not already, STOP SMOKING (smoking decreases the amount of oxygen that gets to your extremities and contributes to poor circulation – it’s a double whammy!)
- get your A1C down to below 7 percent, and keep it there, unless your doctor sets another target for your A1C)
- if you need to lose weight, shoot for 5-7 percent of total body weight
- exercise 30 minutes most days of the week
- eat a healthy diet of whole foods (lean meat, whole grains, fresh or frozen fruits and vegetables, and low fat dairy products)
- keep a good check on your blood glucose regularly, and keep it in your target ranges as much as possible
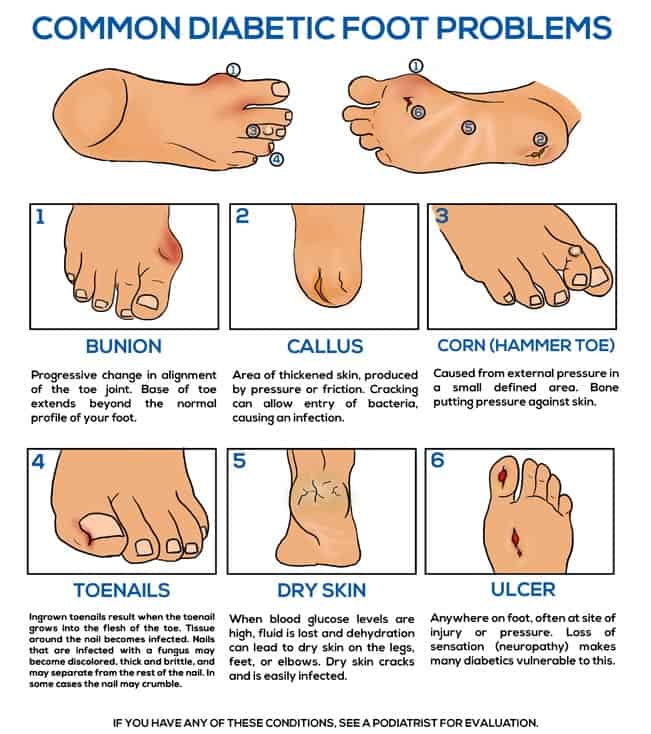
Common diabetic foot problems
- Bunion – caused from a progressive change in the toe joint alignment where the base of the toe extends out
- Callus – area of skin that has become thickened from pressure, which when cracked, can cause an opening for bacteria to enter
- Corn (hammer toe) – external pressure from bone pressing against skin causes a small, defined area
- Ingrown toenails develop when the toenail grows into the skin of the toes, and can cause infection
- Nail fungus – nails become discolored, usually yellowed, thick and easily crack or even crumble
- Dry skin – with high blood glucose, skin becomes dry from dehydration. Dry skin on feet, hands and elbows cracks easily, opening a pathway for infection
- Ulcer – an ulcer can develop at a site of injury or pressure, loss of sensation (neuropathy) contributes to this
Osteomyelitis related to diabetic foot ulcer infection
Death related to diabetic foot ulcer, infection and amputation is significant, and account for at least 50 percent of all diabetes related hospitalizations in the US. Fifteen percent of diabetic foot ulcers will progress to osteomyelitis, or infection of the bone. This presents challenges for healing, and it greatly increases the risk that the patient will need an amputation.
Any diabetic foot ulcer that has been infected for more than two weeks is at risk for osteomyelitis. It should be evaluated for any patient where there is a deep ulcer, involving extensive layers of skin. Chronic ulcers are especially susceptible to osteomyelitis. Ulcers over boney prominences seem to be high culprits for osteomyelitis.
If a diabetic foot ulcer has been infected for more than six weeks, and involves swelling in the toes or foot, there may be osteomyelitis. A white blood cell count and other inflammatory markers, such as high blood glucose levels, should further alert clinicians to perform x-rays and evaluate for osteomyelitis.
If you have osteomyelitis, you will be prescribed antibiotics. You will most likely be taking antibiotics intravenously. If you are prescribed oral antibiotics, make sure to take all of your medications. Fever, chills, and redness at the site of infection should be reported promptly to your doctor.
Foot and skin care – what you can do to prevent amputation
Besides controlling your blood glucose levels, exercising every day, taking your medications as prescribed, and seeing a podiatrist annually for a Comprehensive Foot Exam, there are some things that you can do to keep your feet healthy. You can avoid an amputation. Just follow some simple steps here…
- Make sure to check your feet every single day for redness, sores, blisters, calluses, ingrown toenails, numbness, open sores, change in temperature, and loss of hair.
- Clean your feet by washing them with a mild soap, and warm water. Be careful not to get the water too hot. Make sure you dry your feet well, getting in between your toes. Never soak your feet, because this increases dry skin. Lightly apply a non-alcoholic lotion to your feet, but not between your toes. Friction between the toes could give you a blister.
- Cut toenails straight across, using a toenail clipper that is straight, not curved. It is ok to apply foot powder between your toes if you prefer to.
- Always protect your feet from extremes of temperature, foreign objects, and wear cotton or wool socks, (see our guide to Diabetes Socks). Soft, padded socks help avoid sores and blisters. Seamless socks are best, and make sure not to get a sock that has the top band too tight as to cut circulation.
- Change your shoes once a day to alter pressure points, and make sure to check your shoes for pebbles or other sharp objects. Wiggle your toes and move your ankles every so often to increase blood flow to your feet. Avoid crossing your legs for a long period of time. Finally, wear sturdy, supportive shoes with a wide width and a plenty of room for your toes.
- It’s a good idea to be fitted with shoes late in the day. By then, your feet have already swollen as much as they are going to. Ask for a salesperson to measure your foot, and help you to get a good fit. Put on both shoes with socks, and walk around the store a few times to make sure the shoe is not pinching or rubbing you in the wrong places.
- Never, ever wear sandals, flip flops, or go barefoot if you have diabetes. Hot pavement in the summer is not your friend, and can severely burn your feet.
Are we doing a better job at preventing amputations these days?
Amputations among people with diabetes went down over the past decade. It’s possible that better diabetes education is available, and a bigger emphasis is placed on the importance of foot and skin care. At any rate, it’s good as a CDE to see the numbers going down, and continued efforts should be done to prevent as many amputations as possible.
From the latest research:
“These findings indicate a reduced rate of major amputations in diabetic patients, which suggests an implementation of the consensus guidelines of foot care. We also propose further reduced amputation rates if patients with an increased risk of future amputation (i.e. male sex, kidney disease) are identified and offered preventive treatment early.”5
So you have a foot ulcer that won’t heal, and you have to have an amputation – now what?
The doctor has told you that you have an infection in your foot ulcer, and you need an amputation. What do you do now? At first you may be in denial, or even refuse to have the amputation.
Having a foot or leg amputated is traumatic and means a major body-image change. Allow yourself time to grieve and deal with what losing a part of your body means to you. It may be helpful to join an amputee support group, or speak with others who have had an amputation.6
Refusing an amputation
You can certainly get a second opinion if you are unsure about having an amputation. You should also reach out to a Peer Visitor at the Amputation Coalition (their number is listed a little further down in this article). Some hospitals also have a peer visitor program. These programs are great to help you to realize that there is life after amputation. There are others like you, and there is support out there.
It’s a tough decision, and it is hard to get past the denial and grief. You may wonder will you be able to walk your daughter down the aisle, or play with your grandchildren. All of these thoughts are normal, and part of the process. Seek counselling, and someone to talk to.
Unfortunately, if you refuse to have a needed amputation, the infection and gangrene will spread to other parts of your body, and eventually to your blood stream. You will become septic, and you will likely be given palliative measures to keep you alive. An amputation can give you more years of living, and you will need to have some help and support to get through it to rehabilitation.
Set up needed services for after an amputation
Seeing as this is not the best option, and getting past the denial, having the amputation is important for your health and survival. It’s a hard pill to swallow, and many patients understandably have a difficult time with the decision to amputate. Counseling may be needed, and hospital social workers to assist in setting up needed orthotics, physical therapy and assistive devices when home are important for rehabilitation.
Get a new leg
You will likely be transferred to a rehabilitation hospital following amputation. They will work with you to arrange home health services, usually consisting of a nurse, physical therapist, and social worker if needed.
Get a prosthetist
A prosthetist will be consulted to make a new leg for you. This is a person who will help to make your new limb, and get it fitted right for you. They really lead the care team for getting your new leg. They have a master’s degree, or a doctorate, so they are highly educated in their field. They make sure that you get the appropriate type for your medical conditions, and that you will be strong enough to use it.
The prosthetics used these days are light, and much improved from previous prosthetics. They are much easier to walk on and are more stable. This is due to socket materials, which are more comfortable, and there are now special socket fitting techniques.
The key to a comfortable, well-functioning limb is the socket fit. The socket is the customized portion of the prosthesis that fits over the residual limb. All other components are connected to it, If the socket is not comfortable, the limb will not function well. Because the limb will change shape over time, especially in the first year, the socket will have to be reshaped as well to ensure a proper fit.
The timing of receiving a new leg is dependent on the healing process and their limb, and many people have a post-operative prosthesis (POP). There are often physical therapy exercises and shrinker socks that are used to help shape and heal the residual limb.
The Prosthetist will work with the individual to select the appropriate components, which include the foot, adaptors, pylon, and other pieces that make up a complete leg. The Prosthetist, in conjunction with the Physical Therapist, will help you learn to walk using the prosthesis.
You may not be able to go home and live independently in the same way as you have before, but there are options and transitions available for you. Many people go to a rehab nursing facility, where there are intermediate levels of care, after they are discharged.
Make sure to modify your home before you get there, to accommodate things like a wheelchair, walker, cane, or crutches. You will likely be coming home still using a wheelchair at least part of the time. You can get family to help you, or hire a professional. The social worker also may have ideas. A physical therapist should be able to recommend any assistive devices you may need once home.
Further reading:
Once you are home, and get your new leg, the physical therapist will teach you how to walk on it, and make sure your new leg is not rubbing your residual limb in a way that injures it. The nurse will check your residual limb for signs and symptoms of infection.
Life after amputation
Many people with diabetes have coped with amputation, finding ways to be active and to participate in life the way they wish to.
From research, life expectancy after amputation is a serious picture with a bleak outlook. Look past the statistics and find the hope.
I have known quite a few people with diabetes who have been able to get up and moving again safely, and lived much longer than 5 years after their amputations. Some that I know, you cannot even tell that they have an artificial leg. So take heart, with the right attitude, you can prevail.
Cost of amputation
The biggest cost is personal, of course. When you add up the costs, your efforts to help prevent amputation are well worth it.
The monetary cost of amputation is also high, especially when you factor in all of the following services:
- Hospital
- Diagnosis & Prognosis
- Surgery
- Recovery
- Prosthetics
- Ongoing support
Research related to amputations
Your doctor takes your health seriously, and research shows that working closely with your entire clinical care team will help keep you healthy and mobile. That means keeping regular appointments, following recommendations for lab tests, medications, and other treatments, and working with specialists that can help address your unique needs.
Research has shown that an aggressive, team approach is needed when caring for patients with diabetic foot ulcers due to morbidity and disability that is caused by amputations. One such study confirmed this:
Mental Health
Staying active impacts your emotional health as well as your physical health (and longevity). Your physical therapist will help to get you moving at a safe pace. If you need help with any aspect of your mental health while you are recovering from an amputation, ask your doctor, or contact your local mental health facility.
Amputee Coalition of America
For information on diabetes and limb loss, amputation, prosthetics, and the ACA Peer Visitor program, you may contact the Amputee Coalition of America at (888) 267-5669. You may also visit their website at Amputee-Coalition.org.
The Amputee Coalition has a great document available about the stages that a person goes through as they experience limb loss called “First Step.” The brochure walks the patient through the stages, and what they should expect. Call the number above to obtain a copy of the pamphlet.
Also, on their website, there is an amputee support group database, and patients can call and ask for a Peer Visitor. A Peer Visitor is someone your age, from an area near you, who has similar limb loss experience. It’s a great resource for those who have had to undergo this life changing event.
Other Resources
HangerClinic.com: http://www.hangerclinic.com/new-patient/ampower/ed-resources/Pages/Amputee-Resources.aspx. There’s a wealth of information on the process of getting fit with a prosthesis, home adaptations, helpful organizations, grief and depression, travel, etc.
This link provides information on AMPOWER, Hanger Clinic’s amputee support group and resource center: http://www.hangerclinic.com/new-patient/ampower/Pages/Home.aspx.
A password-protected online community just for amputees, their family members and caregivers, can be found here: http://www.hangerclinic.com/new-patient/ampower/ed-resources/Pages/Educational-Resources.aspx.
Over to you
We would love to hear your take on this article, and any input you could provide related to your experience with diabetes and amputation. We hope that articles such as this can help to save others with diabetes from having an amputation. Please feel free to leave comments in the comments box below.
I would like to thank Karen Lundquist from Amputee-Coalition.org for her incredible help and feedback. Thank you Karen for the time and effort you took to review this piece. So don't worry about amputation but still know your risks.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on June 01, 2020
References
- http://www.amputee-coalition.org/fact_sheets/diabetes_leamp.html
- http://www.cdc.gov/diabetes/statistics/lea/fig3.htm
- http://www.cdc.gov/diabetes/statistics/lea/methods.htm
- http://www.diabetes.org/living-with-diabetes/complications/foot-complications
- https://cardiab.biomedcentral.com/articles/10.1186/1475-2840-11-18
- http://www.webmd.com/diabetes/tc/amputation-for-diabetic-foot-problems-topic-overview
- http://care.diabetesjournals.org/content/26/2/491