In North America, many women are often prescribed birth control medication (often known as oral contraceptive pills or hormonal pills) for treating various conditions as well as preventing unplanned pregnancy.
However, as contraceptive treatments become available without a prescription in the United States, many women lack the knowledge of the risks and side effects of these methods.
For women who are in the prediabetes category or already suffering from type 1 or type 2 diabetes, these treatments cause severe problems with the blood glucose management. To better educate women about how contraceptive methods affect the blood glucose level and various diabetes symptoms, this article will be covering these topics below:
Contents
- How Does Hormonal Contraceptive Work?
- Which Birth Control Pill to Choose?
- How Soon Do Birth Control Pills Work?
- Are There Side Effects of Birth Control Pills?
- Any Woman Take Birth Control Pills?
- How Does Contraception Pills Affect Diabetic Women?
- Tips on Taking Birth Control Pills
- What is Plan B Birth Control?
- Type 2 Diabetes and Other Hormonal Contraception
- Type 2 Diabetes and Intrauterine Devices
- Safety Guidelines of Contraceptive Methods
- Type 2 Diabetes and Barrier Methods
- Last Option: Sterilization
- Conclusion
How Does Hormonal Contraceptive Work?
In order to explain how hormonal contraceptives affect the blood glucose level and other diabetes symptoms, it is imperative that we explain how a woman becomes pregnant and how the hormonal contraceptives work:
What Happens When A Woman Becomes Pregnant?
In order for pregnancy to occur, 2 things need to happen:
1. an egg is released from the ovaries during the ovulation period and is transported to the fallopian tube, and
2. a man’s sperm has successfully fertilized the egg.
Once these two events occur, the fertilized egg will attach to the inside of the uterus. (from medical standpoint, pregnancy begins the moment the fertilized egg is attached to the uterus wall). This event allows the egg to receive nourishment from the mother so that it develop into a baby. In order to shut off the egg production and to sustain the fetus’ development, the secretion of estrogen and progesterone are highly elevated. As a result, some women develop gestation diabetes during their pregnancy.
I advise you to read the following articles:
How Does Hormonal Contraceptives Prevent Pregnancy?
Hormonal contraceptives come in various forms: pills, patches, vaginal rings, and implants. But for oral contraceptive pills, they usually fall into 2 categories. The first category contains a small dose of synthetic estrogen and progestin hormones.
These two hormones combine to stabilize a woman’s natural hormone level and prevent the natural estrogen from peaking during mid-cycle. Without the rise in estrogen level, the pituitary gland will not signal the release of other hormones that cause the release of an egg into the fallopian tube.
To be more specific, the synthetic estrogen’s role is to:
- Prevent the pituitary gland from making the follicle stimulating hormone (FSH) and luteinizing hormone (LH) to avoid ovulation.
- Help prevent the uterine lining (endometrium) from breakthrough bleeding during mid-cycle.
The synthetic progestin’s role is to:
- Prevent the pituitary gland from producing the luteinizing hormone in order to prevent egg release.
- Inhibit the sperm's ability to fertilize the egg.
- Create an unwelcoming environment in the uterine lining to a fertilized egg so that the implantation of the egg is almost impossible.
- Condense the cervical mucus to deter sperm movement, and prevent them from going through the cervix and finding the egg (please note that this is not the key factor to prevent pregnancy).
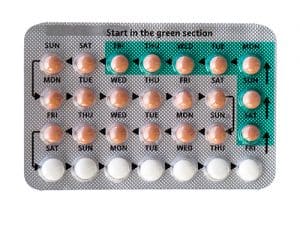
These oral pills come as monophasic, multiphasic, and extended cycle categories. Monophasic pills are used in a 1 month cyclic duration. Each active pill gives you the same dose of estrogen and progestin. And in the last week of the cycle, the inactive pills will allow you to have a regular menstrual period.
For multiphasic pills, the pills will be composed of various estrogen and progestin combinations. But similar to monophasic pills, you will receive inactive pills in the past week of the cycle to allow menstrual period.
Instead of a short-term cyclic contraceptive pills, the extended-cycle pills typically last for 13 weeks. The active pills will last for 12 weeks with the last week cycle being inactive. This method greatly reduces the number of menstrual periods from 13 periods to only 4 periods in a year (this means that you have 1 period for every 4 months).
What are Mini Pills?
Although the estrogen and progestin hormone combination prove to be highly effective, some women cannot tolerate the synthetic estrogen. This brings the second category of the contraceptive pills.
This category is known as mini pills and contains only progestin. These mini pills work by changing the uterus lining to make implantation of fertilized eggs less likely and condensing the cervical mucus so the sperms have a harder time reaching the egg.
Depending on the brand, some mini pills also work by preventing the release of an egg. These mini pills work when taken daily (all the pills in the active are active pills unlike the estrogen/progestin birth control). Although they may be less effective as the other category of birth control, these mini pills still be 95% effective if they are taken correctly and consistently.
Which Birth Control Pill to Choose?
As there are so many brands of birth control pills on the market, it may be difficult to choose a brand. And know that not every brand is a good fit for you. Instead of purchasing the pills without any consultation, talk with your doctor about which option would be optimal for you. There are several factors to consider:
- Your menstrual symptoms (cramps, severe blood flow, acne)
- Whether you are breastfeeding
- The severity of your diabetes
- Whether you suffer from cardiovascular problems
- Whether you are suffering from other health problems such as polycystic ovary syndrome and endometriosis
- Other medications you are currently taking
- Whether you are prone to bloating (some brands tend to promote more bloating than other brands)
How Soon Do Birth Control Pills Work?
If you follow the directions as instructed on the pill packaging and information pamphlet, the birth control pills usually become effective the first month you being the treatment. To ensure that you do not get pregnant within the first month, some doctors may recommend you to use of another form of birth control treatment (e.g. condoms, foams, diaphragm, cervical cap, or spermicide) as a safety net backup. After the first month passes, you rely just on the birth control pill.
How Effective Are Birth Control Pills?
In general, birth control pills have a 9 percent of failure rates. The rates may increase if you do not follow the directions properly (e.g. instead of following the directions and taking the pills the same time every day, you take them within the 12-hour window with higher failure rate results).
Aside from following the directions as precisely as possible, certain medication make the pill much less effective. Some of these medications tend to make the body metabolism faster. As a result, the birth control pill effectiveness runs short before the stated 24-hr timeframe. Other medications, supplements, and even food ingredients that influence the estrogen and progesterone secretion also affect the birth control pills.
Some of the known products that affect the effectiveness of birth controls are:
- St. John’s wort
- Rifampin
- HIV medications such as Saquinavir
- Some anti-seizure medications such as Topiramate and Carbamazepine
- Tartrazine (a yellow food coloring which contains the primidone chemical used to treat seizures and actively decrease nerve impulses)
- Phenobarbital
- Phenytoin
Another factor that affect the effectiveness of the birth control pills is vomiting and diarrhea. Because the pills do not have time to be processed by your body, it put you at a high risk of becoming pregnant. So on days when you are not feeling well, it may be a good choice to use a backup contraception method until you get back to good health for a month before falling back on birth control pills only.
What are Other Uses of Oral Birth Contraceptives?
Although birth pills are used primarily for pregnancy prevention, it is often used to treat other medical conditions. It be used to help regulate menstrual periods and make menstrual cramps less severe. Those who have a history of having very severe blood flow also benefit from the treatment. Other uses include:
- Treatment for severe acne
- Treatment for polycystic ovary syndrome (PCOS)
- Treatment for excessive hair growth due to high testosterone level
- Treatment for perimenopause symptoms such as hot flashes, night sweats, and vaginal dryness and irritation
- Treatment for PMS
- Treatment for migraines
- Treatment for hormone deficiency due to severe weight loss
Other benefits include:
- Lower threat of some cancers such as ovarian and uterine cancer
- Lower chance of anemia
- Lower risk of pelvic inflammatory disease
- Reduce chance of contracting flu
Are There Side Effects of Birth Control Pills?
Just like any medication treatments, there are always side effects. The common side effects of birth control pills include:
- Dizziness
- Nausea
- Headache
- Slight weight gain
- Slight to significant bloating depending on the brand
- Soreness or swollen breasts
- Spotting of blood between periods
- Periods with lighter blood flow
- Possible chance of depression
- Possible decrease in sex drive
Please note that these side effects should not be causing you serious discomfort. If at any point you find the pills to cause too many side effects, talk with your doctor and switch to another brand. A different formula of estrogen and progestin may work better for you.
Dangerous Symptoms You Should Not Ignore
However, if you experience the following side effects, you should contact your doctor immediately or seek emergency care help from the urgent care center or emergency room. These 5 side effects easily be memorized as “A-C-H-E-S”:
- Abdomen Pain
- Chest Pain
- Headaches (very severe)
- Eye problems which includes blurry vision, doubled vision, and high intolerance to light
- Swelling or aching in the limbs
These serious symptoms may be a sign that you are suffering from serious conditions such as stroke, blood clots, aneurism, extremely high blood pressure, heart disease, liver disease, or gallbladder disease.
As a matter of fact, there has been FDA investigation suggesting that certain birth control pills that contain drospirenone (a synthetic version of the progesterone hormone) may increase the chances of developing blood clots.
Brands of oral contraceptives that include drospirenone include YAZ, Yasmin, Safyral, Beyaz, Loryna, Gianvi, Syeda, and Zarah. Although the investigation is inconclusive (some brands show a correlation with the risk of developing blood clots and others do not), you may want to steer clear from these brands if you have a family history of developing blood clots. As a woman with diabetes, you may also want to avoid brands with the drospirenone ingredient.
Any Woman Take Birth Control Pills?
In general, birth control pills are safe for most healthy women. Having said that, they are unsuitable for women who fit these factors:
- Over the age of 35 years old and smoke
- Suffer from migraines with aura
- Have a history or family history of blood clots
- Suffer from serious heart or liver disease or have a family history of these diseases
- Suffer from high blood pressure or have a family history of these medical conditions
- Suffer from breast cancer or uterus cancer or have a family history of these cancers
How Does Contraception Pills Affect Diabetic Women?
In the past, women with diabetes were often told to avoid hormonal contraceptives due to the speculations that increased dosages of estrogen and progestin drastically affect the blood glucose level.
After years of clinical studies and correlation studies, there is still no consistent evidence to confirm that hormonal oral contraceptives directly increase the risk of developing diabetes (even for women with gestational diabetes). At the same time, the data cannot confirm that the estrogen and progestin worsen the symptoms of women who suffer from diabetes.
The only confirmation is that the use of DMPA (Depo medroxyprogesterone acetate) trigger slightly higher fasting glucose and insulin levels. In the present day, the FDA has recognized the use of estroprogestative pills as a safe preconception care option for preconception for women with uncomplicated diabetes.
Hormones and Blood Glucose Level
Although hormonal birth pills are labeled safe for women with diabetes, many individuals have experienced a loss of control in their blood glucose level when they first begin their treatment. However, this problem be fixed by a change in the insulin or medication treatment dosage.
For women who suffer from diabetes along with other diabetes-related complications, it may still be avoided. Women who are at the highest risk are the ones who suffer from cardiovascular diseases, deep vein thrombosis, or uncontrolled high blood pressure as a result of diabetes. Those who are at risk may consider using a progestin-only pill instead.
Possible Weight Gain Issue
A serious concern to consider for women with type 2 diabetes is that the weight gain associated with the pill drastically increase the chances of developing thromboembolic and arterial risks.
These lead to severe life-threatening complications. Those with gestational diabetes are at increased risk for developing type 2 diabetes after pregnancy. In addition, women with prior gestational diabetes history are found to have a higher risk of cholesterol problems and high blood pressure.
The high blood pressure increase the chance of developing kidney and liver problems, as well as glaucoma and retinopathy.
Osteoporosis Risk
Another factor to consider is that progestin-only pills cause a substantial bone loss in both healthy and diabetic individuals. For women who have diabetes and suffer from bone loss complications, progestin-only contraceptives should not be taken unless truly necessary. For women who are currently taking progestin-only pills, they should not continue the treatment for more than 2 years as the bone loss cannot be fully reversed after stopping the pills.
Risk of Depression
According to correlation studies, women who are on hormonal contraceptives are 2 times more likely to develop depression than women who do not use the birth pills. The risk significantly increases to 80% for teenagers between the age of 15 to 19 who are on estrogen/progestin combination oral contraceptives. However, the rates drops when other hormonal methods are used such as injections, patches, intrauterine devices, or vaginal rings. For young women with diabetes, other hormonal contraceptives may be a more beneficial option than oral birth control pills.
Tips on Taking Birth Control Pills
- Always have another backup form of birth control such as condoms, spermicidal foam, or Plan B emergency contraceptive on hand just in case you forget to take a pill or you have missed the window of effectiveness.
- Keep your pills with you in cases when you sleep over.
- Try to take your pills at the same time daily. Moreover, if you are using the patches, remember to replace your patch on the same day every week.
- If you are using the vaginal ring method, remember to take out the ring after 3 weeks of usage.
- Do not wait last minute to get your refills. As soon as you start the last prescription, go get your refills to avoid a lapse between treatments.
- Consult with your doctor first before skipping the inactive pills to avoid periods (it be done but it may significantly decrease your chance of having periods if extended active pills are used).
- Always remind your doctor or pharmacist you are on the pill, patch, or vaginal ring to lower the chance of medication counteraction.
What is Plan B Birth Control?
Plan B often be called as the “morning after pill”. It is an emergency over-the-counter contraception available to women to prevent pregnancy after sexual intercourse without protection.
Unlike the common believe, you do not need to wait until the morning to take the pill. As a matter of fact, the sooner you administer the birth control, the more effective it is at prevention.
According to research studies, Plan B reduce the chance of pregnancy up to 89% if the pill is taken within the 72-hour timeframe. However, if taken within 24-hours, the effective rate jumps up to 95%.
How Many Treatments Do You Need?
Unlike your usual oral pills, you only need 1 pill as a treatment. Each dose of Plan B contains 1.5 mg of levonorgestrel (an alternative synthetic form of progestin). Similar to the mini pill, it prevents pregnancy in 2 ways: 1) It prevent the release of an egg from the ovary, or 2) prevent the fertilization of the egg by changing the uterus lining to make the egg implantation impossible.
Plan B Is Not an Abortion Pill
It is a myth that Plan B works as an abortion pill (the RU-486 treatment). It does not cause an abortion or a miscarriage by any means. If the egg has successfully been fertilized and implanted in the uterus, the Plan B pill will not have any function at all.
Risk of Regular Plan B Use
Even though this emergency contraceptive is highly effective, you cannot use it as a regular birth control method.
According to clinical trial studies, regular use lead to significant weight gain of 15 pounds on average, ovarian cyst enlargement, severe cases of depression, gallbladder disease, respiratory disorder, and high blood pressure. These side effects be even more evident in women with diabetes.
Later in life when you decide to have children, you will be having much higher chance of developing ectopic pregnancy in which the egg develops outside the uterus. If left undetected, it may lead to rupture of the fallopian tube, severe blood loss, and even death. As a result, unless it is truly necessary, you should avoid taking a morning-after contraception.
Type 2 Diabetes and Other Hormonal Contraception
Birth control pills are not the only way to use hormones for pregnancy prevention purposes; they work as injections, implants, rings, and patches.
Vaginal Ring
Another alternative to the hormonal procedures is the vaginal ring. In this procedure, a transparent, flexible ring is inserted into the upper vaginal area. This ring will deliver a small dose of progestin and estradiol (a precursor hormone of estrogen) daily for a total duration of 4 weeks.
In essence, the ring works very similarly to the oral pills as it delivers both estrogen and progestin (unlike the implant and injection only delivering progestin).
Although this method does not last as long as the implant and injection, it is a safer choice for women who are unsure of the side effects. This is because if they sense that the effects are too bothersome or they wish to stop the treatment, they simply remove the ring by a medical professional.
Here is a great video that explains what is birth control ring.
Contraceptive Patch
For an even more convenient method, there is the birth control patch. Much similar to the nicotine patch, the contraceptive patch works when it is applied to the skin. After applying, the patch will release a progestin and estrogen combination dosage daily for one week.
The patch needs to be replaced every week for a total duration of 3 weeks. In the fourth week, no patch is needed to allow the period to begin. Similar to the vaginal ring and the oral pills, the patch impact on the blood glucose level and cause side effects that are related to the fluctuation of estrogen in the body.
For women who are suffering from diabetes, you should consult with your doctor about adjusting your insulin and medication dosage to compensate for the blood glucose change.
Injections
Injections have become a popular choice for women because of convenience and highly effective results. Just one injection already offer 3 months of birth control properties.
Presently on the market, the most popular brand is Depo-Provera, or short for DMPA (1 injection dose cost about $25). With this method, women only need to worry about birth control 4 times annually. For those individuals who have busy schedules especially in the morning, this be a highly convenient solution.
The disadvantage is that not everyone adjust to the progestin hormone in the injection and be a fan for the possible side effects such as bloating, weight gain, dizziness, unwanted hair growth, headaches, and anxiety episodes. And once you have the injection, you may have to deal with these problems for the next 3 months until the effects wear off.
Contraceptive Implants
For women who do not wish to receive an injection every 3 months, there is the option of a contraceptive implant. This is a small, thin plastic rod (about the size of a matchstick) being inserted under the skin of the upper non-dominant arm.
This procedure requires no incision but it must be injected and removed by a trained medical professional. Similar to the injection, this rod releases small doses of progestin to prevent pregnancy. Just one implant last for 3 years. This is an optimal procedure for women who do not wish to bear children in the near future.
Type 2 Diabetes and Intrauterine Devices
Intrauterine Devices (IUDs)
Intrauterine devices are small implants that are inserted into the uterus. Currently on the market, there are both hormonal IUDs and non-hormonal IUDs available for women with different needs. In general, all these devices are shaped like a little t-shaped plastic contraception that needs to be implanted and removed by a doctor.
At this time, there is only one brand of non-hormonal IUD (the brand is called ParaGard) available on the U.S. market. This IUD is often referred to as “Copper- containing Intrauterine Device” because it is made of plastic with a small amount of natural copper coated on the tips of the ends.
It works by blocking sperms from reaching the egg. Once inserted, it immediately becomes functional and actually be used as an emergency contraception to prevent pregnancy as much as 5 days after unprotected sex. And the most astonishing advantage is that it works up to 12 years before the removal is needed.
For women who have diabetes and are currently taking other medications for their conditions, this may be the optimal choice as this IUD does not contain any hormones and will not interact with any medications, supplements, or herbal remedies. The only risk is that women increase their chances of contracting an infection in the uterus. For women with diabetes who are at a higher risk of developing infections, this method of birth control may require some considerations.
There are 4 brands available on the U.S. market: Skyla, Mirena, Kyleena, and Liletta. They all work similarly as the progestin hormone condenses the cervical mucus to prevent sperms from reaching the egg in the uterus. Depending on the brand you choose, the IUD be effective between 3 to 6 years.
Safety Guidelines of Contraceptive Methods
According to the United States Centers for Disease Control and Prevention (CDC) guideline for assessing the safety of each contraceptive method based on women with various diabetes scenarios. The number ratings are:
- No restriction for the use of this method
- Advantages of using the method generally offset the speculative or confirmed risks.
- Theoretical or proven risks typically offset the advantages of using the method.
- Unacceptable health risks overshadow the advantages of using the method.
Rating System:
- CHC: combined hormonal contraception (pill, patch, and ring)
- COC: combined oral contraceptive
- Cu-IUD: Copper containing intrauterine device (e.g. ParaGard)
- DMPA: depot medroxyprogesterone acetate injection
- LNG-IUD: levonogestrel-releasing intrauterine device (e.g. Mirena)
- POP: progestin-only pill
Type 2 Diabetes and Barrier Methods
Although hormonal birth control methods a high effective, they are not the only way to prevent unplanned pregnancy. For women who have diabetes, the elevated estrogen and progestin subject them indirectly into developing other diabetes-related complication. As a result, it may be more beneficial to resort to non-hormonal methods.
Barrier methods be the best choice as they work by stopping semen from contacting the uterus. For most women with diabetes, barrier methods be an effective contraceptive choice because they will not affect blood glucose level and cause weight gain.
However, before using these methods, you should know that they may increase your chance of developing yeast infections. To avoid such complication, you should learn the correct way to use and maintain the cleanliness of the apparatus.
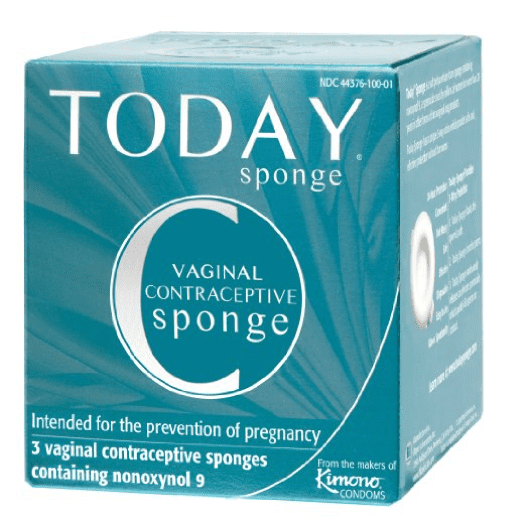
Birth Control Sponge
Just as described by the name, this method uses a foam sponge being inserted into the vagina to actively prevent unplanned pregnancy. It works in two ways:
1. It blocks the passage of which sperms must travel to reach the egg, and
2. It kills the sperms with the spermicide coated on the surface of the sponge.
Unlike other methods that require a medical professional for insertion, you apply the sponge yourself. The disadvantage is that if you do not insert the sponge correctly, the effectiveness of the sponge drastically decrease and result in pregnancy.
Cervical Cap and Diaphragm
Very similar to the sponge method, only it is made of more durable silicone.
Unlike the sponge which actually break apart from over bending, these two apparatus are less likely to break. However, because they are made of plastic, they be more difficult to insert into the vagina.
Further reading:
It also shift location due to certain sexual positions and heavy thrusting. If such incidence occurs, you may need to resort to Plan B oral contraceptive to avoid pregnancy. Another disadvantage is that these two methods cannot be used during menstruation as they block the blood flow.
Last Option: Sterilization
For women who do not wish to bear children or already have children, and find all birth control methods to be bothersome and/or irritating to their bodies, there is also the option of choosing permanent sterilization.
This surgical procedure called a tubal ligation (you often hear the common term “tying the tubes”). Unless a woman chooses to undergo another surgery to reverse the sterilization procedure, the effect is general permanent.
Although the result has the highest success rate, it be a disadvantage for women who are not 100% sure that they do not wish to have children. But for women who have type 2 diabetes and have a long family history of cervical and uterine cancer, sterilization may be the best option provided that they have thoroughly discussed the pros and cons with their doctors.
Conclusion
All women should have a say in taking care of their bodies and making the decision when they want to have a child. It is especially important for all women with diabetes as pregnancy severely affect the blood glucose level and cause life-threatening complications for both the mother and the baby. We hope that our article has answered your concerns and open up the options for choosing your birth control method. If you have any personal experience or comments to share, please leave us a message. We would be delighted to hear from you.
References
- Banerjee C. Obesity, Oral Contraceptive Use, and Cerebral Venous Thrombosis in Women. JAMA Neurol. 2016. doi:10.1001/jamaneurol.2015.5107.
- Berenson, Abbey., et. al. Effect of Injectable and Oral Contraceptives on Glucose and Insulin Levels. Obstet Gynecol (2011): Jan 117(1) 41-47.
- “Contraceptive Implants Come of Age,” Progress in Reproductive Health Research No. 61, World Health Organization.
- “Fuller Information and More Choice — The Responsible Way Ahead,” Progress in Reproductive Health Research, 1995, No. 35, part 2. World Health Organization.
- “Health Professionals,” Plan B Clinical Information.
- Mitchell D. Creinin, MD, “Emergency Contraception: More Than a Morning After Pill,” Medscape General Medicine, 1999.
- “Repeated Use of Emergency Contraception: The Facts,” International Consortium for Emergency Contraception. Policy Statement, July 2003.
- Sarah H. O’Brien, Terah Koch, Sara K. Vesely, Eleanor Bimla Schwarz. “Hormonal Contraceptives and Risk of Thromboembolism in Women with Diabetes”.
- Diabetes Care 2016 Nov; dc161534.
- Zuurbier SM, Arnold M, Middledorp S, et al. Risk of Cerebral Venous Thrombosis in Obese Women. JAMA Neurol. 2016. doi:10.1001/jamaneurol.2016.0001.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on May 28, 2020