Continuous glucose monitors or CGMs can be a lifesaving device for people with any type of diabetes. They continually check your blood sugar 24 hours a day and alert you you before you begin experiencing low or high blood sugar levels.
They can reduce the number of times you have to check your blood sugar each day which is welcome news for everyone with diabetes!
Insurance coverage is changing this year with Medicare jumping on board also, so this is the time to learn about this awesome piece of technology available to you.
I know there are a lot of questions surrounding the use of continuous glucose monitoring, so we will break it all down here for you!
- What is a CGM and how does it work?
- Is it right for me?
- Will I still have to check my blood sugar?
- What choices do I have currently on the market?
- Will my insurance cover a CMG? How much will it cost?
- Can I travel and play sports with a CGM?
In this article I will answer all your questions.
Contents
- What Is Continuous Glucose Monitoring (CGM)?
- How does Continuous Glucose Monitoring (CGM) work?
- Benefits of CGM
- Is Continuous Glucose Monitoring for Me?
- Types of Continuous Glucose Monitoring Systems on the Market
- Continuous Glucose Monitoring Insurance Coverage
- Continuous Glucose Monitoring Cost
- Traveling with your CGM
- Can I Still Do Sports with a CGM?
- Tips and Tricks with a CGM
What Is Continuous Glucose Monitoring (CGM)?
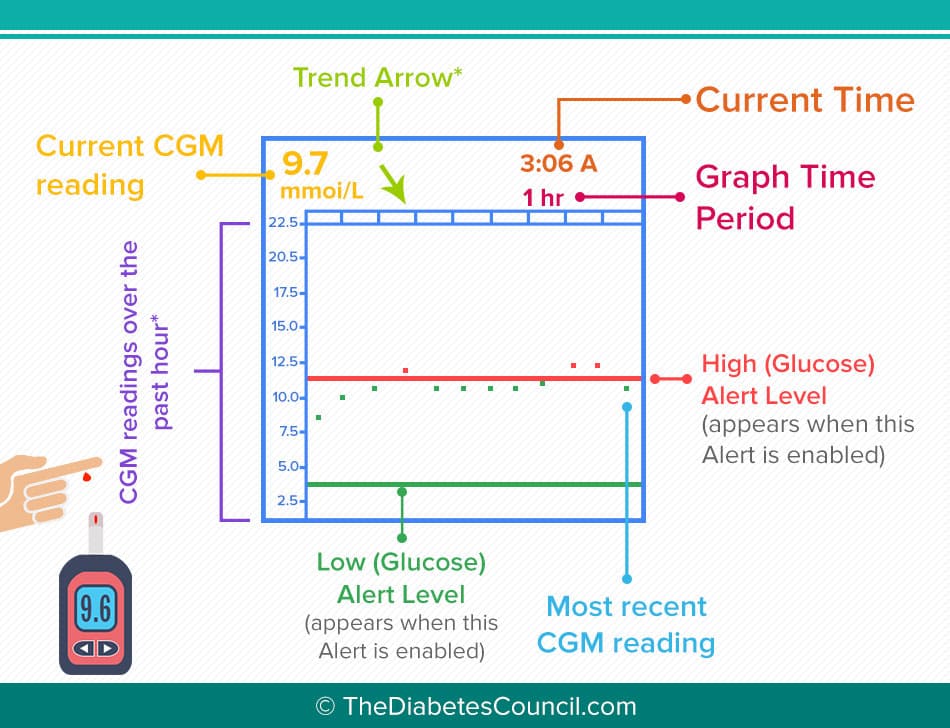
A continuous glucose monitoring system or CGM is a system that does just what it sounds like, it monitors you glucose (blood sugar) continuously…well, every 5 minutes, 24 hours a day! You are able to see what your blood sugars are with a receiver; the data is transmitted from a sensor which is inserted right beneath your skin which is attached to a transmitter which sends the data to the receiver.
Now, the newest system are even integrated with a Smartphone; with this advancement you can check your data right from your cell phone. For parents with children, this technology is peace of mind, allowing them to check their child’s blood glucose level any time-day or night.
There are two different types of systems:
The first is a personal continuous glucose monitoring system that you wear at home 24 hours a day 7 days a week. You are in charge of changing the sensor every 7 days and you can even upload your data and share it with your physician. Alternatively, it can also be uploaded when you go in for your doctor visits by the office staff.
The other CGM system available is called a Diagnostic CGM; this is available through some physician’s offices, normally only at endocrinology offices. This CGM is identical to all other CGMs, it senses your blood glucose every 5 minutes, 24 hours per day. You wear this CGM for only 3 days, checking your blood sugars with your meter 3-4 times per day before meals and maintain a log. You will be tracking your food intake, your blood glucose levels, any insulin you inject and any other pertinent details such as exercise and low blood sugar symptoms. You return at the end of the 3 days, the sensor and transmitter are removed, the data is uploaded and reports are generated and provided to your physician. You will then sit down and review all the reports and your logs in detail and will be amazed at what valuable information the CGM has provided in just 3 short days.
I recommend reading the following articles:
- Lancets & Lancing Devices For Diabetes: Read This Before You Buy
- Are People With Diabetes More Prone to Aggression?
- Can Diabetes Type 2 Be Reversed? Experts Answer
- How Will the FDA Approval of the Artificial Pancreas Change the Lives of Those Living with Type 1 Diabetes?
- Exercise Activities That Every Person with Diabetes Should Do
- Top 10 Popular Blood Glucose Meters Put to the Test
There are currently 2 types on the market today, but you will have to check with your physician’s office to see if they carry either one. If they do not, they can always refer you to an office who does. There is Medtronic’s iPro2 Professional CGM and FreeStyle's LibrePro.
I first started training patients on continuous glucose monitors using the 3 day diagnostic CGMs. At that time, I worked in a busy endocrinology office and we used them very frequently. It was a valuable tool in getting a glimpse inside the patient’s lives and what was really happening inside their bodies 24 hours per day.
The food/BG/insulin/activity log along with the CGM data provides the insight we need to provide you with a breakdown of just what is going on in your body. Many times we determine your insulin doses may need to be adjusted. Or your poor sleep is having a detrimental effect on your diabetes and you need a referral for a sleep study. Or the stress in your life is causing your blood sugars to rise.
Some years ago, I had a female Type 1 patient in her early twenties who was referred to a diabetes outpatient program I was working in for an individual visit because her blood sugars were out of control and her endocrinologist couldn’t determine the cause. I suggested the diagnostic CGM which he ordered. When she returned with her log and we uploaded her data, we were amazed at one spike in particular.
Her BG had gone from a normal level of around 110mgdL up to 400mgdL and stayed there for an hour, then dropped right back down to around 100mgdL again. We immediately assumed it was something she had eaten, and went to the log at that time and were stunned. She had written in her log, “fight with friend on phone for one hour”. We couldn’t believe it!
This illustrated the effect of stress on blood glucose levels so well, so much better than I could have ever have done in just telling her that. I tell patients this all the time, how stress effects their diabetes, but I don’t think they believe me! This made her a believer and I hope it helps you believe too. Better yet, go get a 3 day diagnostic CGM and see for yourself!
Regarding your food intake, most people believe it’s the food that is wreaking all the havoc on their blood glucose levels. Your friends and family believe this, your healthcare provider believes this, and you may believe this. Let’s face it, sometimes it is…especially if you are eating 2 Snickers bars for lunch every day. But, sometimes it’s the timing of your meals, or the lack of carbohydrates at meals, or the lack of protein with your meals. I could go on and on, but this is why you need to see a Certified Diabetes Educator! We sit down with you and flesh out these factors.
How does Continuous Glucose Monitoring (CGM) work?
So, the great news is, the technology for CGMs is becoming more advanced every day! They are becoming more accurate, and more advanced and now even have the ability to work with your Smartphone with the release of Dexcom's G5 Mobile CGM System.
The basic way any continuous glucose monitoring system works is you will insert a tiny sensor under the skin of your abdomen that can be worn up to 7 days. This sensor will be reading glucose levels in the interstitial fluid below your skin’s surface. The sensor is attached to a transmitter taped to your abdomen. This transmitter sends the glucose level data wirelessly to your pump, transmitter or your Smartphone where you can view it.
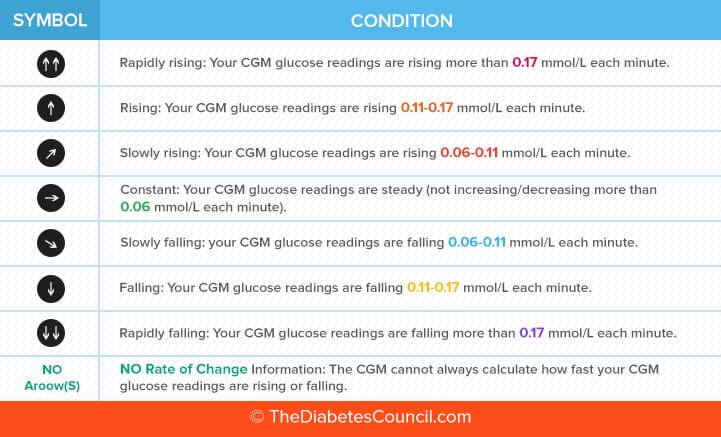
As I said earlier, the sensor will be sensing and sending your blood glucose levels every 5 minutes to your devices 24 hours per day. This means that at any given time during the day or night, you can look at your device and see how your blood glucose level is trending. You can also see how quickly your blood sugar level is changing; if it is dropping very fast, you would see 2 down arrows, if it is rising very fast, you would see 2 up arrows. Every company also has alerts you will set up in your device as to when you want to be notified of a high blood sugar and a low blood sugar.
Does CGM replace finger sticks?
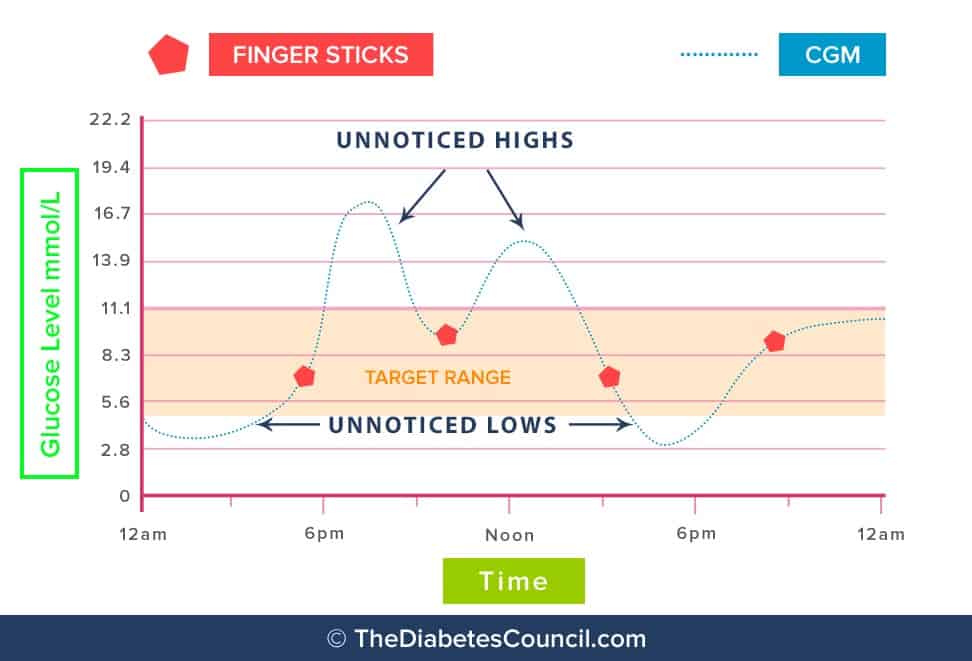
The short answer today to this question is no, but this answer may be changing in the future. Technology is always changing, but for now, you will still need to check your blood glucose using your blood glucose monitor by a finger stick 2 hours after you start the CGM and then every 12 hours to calibrate it.
Calibration is needed to ensure the sensor readings are matching the readings you are getting from your blood glucose meter. This is to make sure the sensor readings are as accurate as possible. Remember, technology is not perfect, so calibration is still necessary to achieve the most accurate data.
There is also a lag time of approximately 5-7 minutes between the blood glucose level in the capillary blood of your finger stick and the interstitial blood measured by your sensor. The interstitial blood glucose reading 5-7 minutes behind, which is why your Certified Diabetes Educator advises you to always check your blood sugar using your blood glucose meter if you get a low or high reading on your CGM.
One important fact to note is that taking medications that contain acetaminophen while wearing your sensor can give you false readings; it will falsely raise your blood glucose readings.
Benefits of CGM
The benefits of a continuous glucose monitoring system are absolutely tremendous! I have seen them firsthand.
Now, I know diabetes is a big pain in the-you-know-what for every single one of you reading this today. Having your friends and family constantly judging you for everything you eat, having to count every carbohydrate you eat, having to either take insulin injections multiple times per day or wear an insulin pump 24 hours a day. On top of that you have to check your blood sugar many times per day and worry about what your blood sugar levels are constantly. Having to deal with the horrible feeling you get from a high or low blood glucose or the danger of the low blood glucose levels. This technology can help you!!
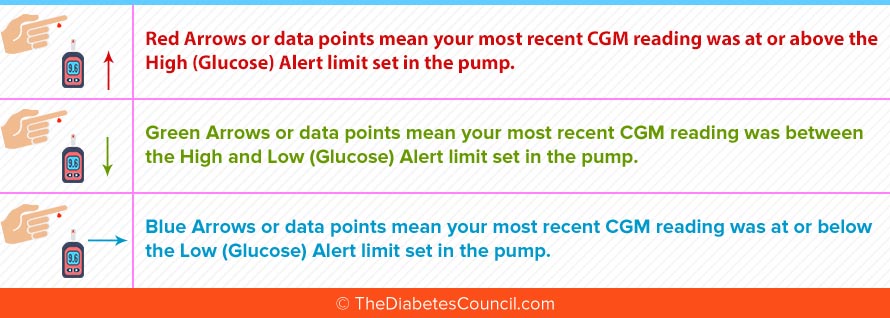
The purpose of any of the continuous glucose monitoring systems is to provide you with real time data, showing you what your current blood glucose is and how it is trending. In other words, is it dropping very quickly? It is rising very quickly? You will know right away by alarms that are set on your device. The alarms will also serve to warn you if your blood glucose reaches a certain low point and high point. You will work with your physician and your Trainer or Certified Diabetes Educator to determine what levels your alarms should be set at. The purpose to setting these alarms are to prevent the high and low blood sugars that are causing damage to your body and let’s face it, we know can be life threatening.
As a Registered Nurse, Certified Diabetes Educator, there isn’t anything that frightens me more than a patient not understanding the importance of preventing and properly treating hypoglycemia (low blood sugar).
If you have hypoglycemia too often, one to two times per week for a prolonged period of time (normally a two year window, depending on the severity of the lows), you will develop a condition called Hypoglycemic Unawareness. You will no longer feel the symptoms of your low blood glucose levels. When this happens, your blood sugar could drop extremely low, and you will become unconscious as your first symptom. If this happens and you are home alone with a blood glucose of 8 or 10 mg/dL, the odds of survival would be low.
If however, you had the benefit 2 years before of a continuous glucose monitor which alarmed when your blood glucose was 80mg/dL and you were able to successfully prevent all your low blood glucose levels, you would prevent the Hypoglycemic Unawareness from ever developing!
Is Continuous Glucose Monitoring for Me?

- If your blood glucose levels are not within normal limits fasting and 2 hours after any meal, and your physician cannot determine how to get you in control, a CGM will accomplish this.
- Physicians typically order for women with Gestational Diabetes (or even while they are trying to conceive) because their blood glucose levels need to stay on target for the health and proper development of their baby and to prevent any complications related to the pregnancy itself.
- If you have an insulin pump, your physician may recommend you consider adding a continuous glucose monitoring system.
- Another reason to choose continuous glucose monitoring is parents of children with diabetes and caregivers of people with diabetes. Can you imagine the peace of mind it could provide to parents of children, especially during the overnight hours? The newest systems have the capability to access the data remotely from compatible smart devices, allowing viewing of the data overnight, while the child is at school or while they are playing sports.
The technology for continuous glucose monitors is constantly evolving and being improved upon, so if you have access to the best systems in the world, why not take advantage of this advanced technology?
I believe the best first step would be to speak with your physician to see if a continuous glucose monitoring system would be right for you. They could provide you with brochures of all the available devices on the market today which we will review now.
Types of Continuous Glucose Monitoring Systems on the Market
There are several choices on the market today, so I will break it down for you here.
- Nutrisense (Use coupon for $25 OFF Health25):
- Dexcom G5 Mobile CGM System
- t:slim G4 Insulin Pump (integrated with a Dexcom sensor)
- Medtronic Guardian Sensor 3 (integrated with new Minimed 670G model pump)
- Medtronic Enlite Sensor (integrated on 530G and 630G model insulin pumps)
- Animas Vibe Insulin Pump and CGM (integrated with a Dexcom sensor)
Medtronic
Coming out this Spring of 2017 is the highly anticipated Medtronic Minimed 670G system. It is the first Closed Loop System; it will have a new Guardian sensor which will automatically stop and restart insulin based on your preset target blood glucose levels. The pump will be able to adjust your basal insulin every 5 minutes to keep you in your target range 24 hours per day.
Dexcom Continuous Glucose Monitoring System
Dexcom’s G5 Mobile CGM System recently gained FDA approval for making treatment decisions without using fingersticks…in certain situations. You will still need to calibrate every 12 hours, if too low or too high of course, or if your blood glucose is changing rapidly. This approval does mark a change in the way people with a CGM will treat their diabetes, so it is quite remarkable.
Continuous Glucose Monitoring System Watch
So, you can even download apps to your smart watches…like an Apple watch…that will allow you to monitor your CGM sensor data. It will function as your mobile receiver. Dexcom has an app you can download which allows you to do this. I found one great website which covers every question you can imagine regarding CGMs and watches.
Continuous Glucose Monitoring Reviews
Medtronic has provided some reviews on their own website and I will provide the links to additional reviews here as well, including one comprehensive head-to-head comparison.
Continuous Glucose Monitoring Insurance Coverage
Continuous Glucose Monitoring insurance coverage is, first of all going to be dictated by whether or not you have insurance, and then, by what type of insurance you have. Is it private insurance, or Medicare or Medicaid? All of these factors will play into what type of coverage you have for a CGM system.
There is some really exciting updated coverage news for 2017; Medicare just announced it will cover Dexcom’s G5 Mobile CGM under Durable Medical Equipment status. This is excellent news for Dexcom and for anyone who is covered by Medicare. This will only apply for Dexcom’s Mobile system which can be accessed from certain Smartphones.
Historically, people with Type 1 diabetes will usually qualify easier for a CGM than those with Type 2 diabetes, but if your physician can prove there is a medical necessity, then you may qualify for coverage. Let’s say you have coverage. Next, your insurance company may want to determine if you actually need a continuous glucose monitor. This can be done by providing blood glucose logs which are uploaded from your blood glucose meter. If you are experiencing both high blood sugars and low blood sugars, more than likely you will qualify. What will they consider as high and low? Hyperglycemia is defined as a blood glucose level of 250mg/dL or over. A low blood sugar is 70mg/dL or below.
If your insurance company denies coverage for your continuous glucose monitor, there are steps you can take; your physician’s office will be knowledgeable regarding these next steps, such as a Peer to Peer Review (just a fancy term for your doctor calling the insurance company’s doctor) and Appeals.
Continuous Glucose Monitoring Cost
The cost of your continuous glucose monitoring system will vary depending on a number of factors.
First, which system and company you choose. Secondly, which insurance plan you have.
If there are costs that you cannot afford, the CGM company may be willing to work with you. They may have a payment plan they can set up with you, so please talk with them if cost is an issue.
So, after you get the wonderful news that you have been approved, you will receive your CGM system and a limited number of supplies. Usually you will receive at least enough supplies to last one month. Some insurance companies will arrange to have 3 months of supplies shipped. This will vary depending completely on your insurance company. This will not be dictated by the CGM company or by your physician, it will be solely up to your insurance company.
Bear in mind, there will be costs upfront and then ongoing costs associated with having a CGM system. The ongoing costs will be for your supplies…your sensors and dressings to cover the sensors.
Traveling with your CGM
When flying, TSA is very familiar with insulin pumps and continuous glucose monitoring systems. Just show them the device that you are wearing, tell them exactly what it is and show them your monitor. Ask that the monitor or sensors not be put through the x ray machine because they may become damaged from the x rays. The following excerpt was taken from Dexcom's website regarding this important information:
X-Ray Machines
Receiver, Extra Sensors
Don’t put your Dexcom G5® Mobile CGM System components through baggage x-ray machines. Before your screening process begins, ask the TSA Officer to perform a visual inspection of the receiver and your extra sensors. Place all Dexcom G5® Mobile components in a separate bag before handing over to the Security Officer. For other medical supplies, such as medications, meters, and strips, check manufacturer’s instructions or the TSA website.
Click here to download our "Notice of Medical Device" letter. This can be filled out by your physician and presented to airport security to better explain your Dexcom CGM System.
Use of AIT body scanners has not been studied and therefore we recommend hand-wanding or full body pat down and visual inspection in those situations.
Can I Still Do Sports with a CGM?
The easy answer to this question is yes!!
The CGM is such a great tool to have when you are doing sports!
Number one, it is waterproof so you can even go swimming with it on. There is even research proving safety and accuracy while scuba diving.
Number two, because you risk fluctuations of your blood sugars while exercising, you will maintain your safety by wearing your CGM. After strenuous or vigorous exercise, you are at risk of a high blood glucose initially due to spurts of adrenaline, then low blood sugars for many hour afterwards; wearing your CGM will continue to keep you safe by alerting you to any deviations in blood glucose values.
Tips and Tricks with a CGM
Also, remember to try and calibrate when your blood glucose is >40mgdL and <400mgdL and to calibrate once every 12 hours.
The first few days or even week may be overwhelming on your new CGM system. You may start receiving alarms, both low and high alerts. This is actually a good thing, because you will be receiving this information before the low or high blood sugar actually occurs. Yet, receiving all these alerts, alarms and getting used to your new routine may be difficult until you have these new habits down pat.
Remember, you are not alone! There are many personal stories you can find online with tips on getting started. Here are a few links from patients just getting started sharing their first few days:
- My Overwhelming First Days With a Dexcom CGM
- If I Knew Then: Continuous Glucose Monitoring – Dexcom
- Keeping the Dexcom Stuck
Finally, one unique perspective from a twenty-something who does not have diabetes, but wore a continuous glucose monitor a week. They wore the CGM to gain a better understanding of what life may be like for someone living with diabetes.
I further suggest reading the following:
If you have questions, use your resources. You will have a user guide, and a great website with whatever brand CGM you choose. Hopefully you will also be working closely with a Certified Diabetes Educator (CDE). Keep in close contact with your CDE, especially during those first few weeks with questions. When you think of a question, write it down, so you have a list ready when you speak with or follow-up with your CDE in person.
The data all the CGM systems provide is really quite remarkable. You will be amazed the first time you print out your reports! If you don’t feel comfortable analyzing this data, set up an appointment with your CDE or endocrinologist. They will be able to help you identify trends which will allow your healthcare professional to make any adjustments necessary to your medications. That elusive, in-target Hemoglobin A1c is within your reach! Hope this article helps you how to use this device and post your comments below!
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on June 02, 2020