Approximately 81.1% of mothers breastfeed their babies when they are born. About half of those are still breastfeeding 6 months later.
There are many benefits for breastfeeding moms and babies if they are able to stick with it for at least 6 months. For moms with diabetes, there are even more benefits.
However along with the benefits, there may also be some challenges as well.
The following article provides information about the advantages of breastfeeding for all moms and babies as well as the things to look out for which are unique for nursing mothers with diabetes.
Contents
The perks of breastfeeding
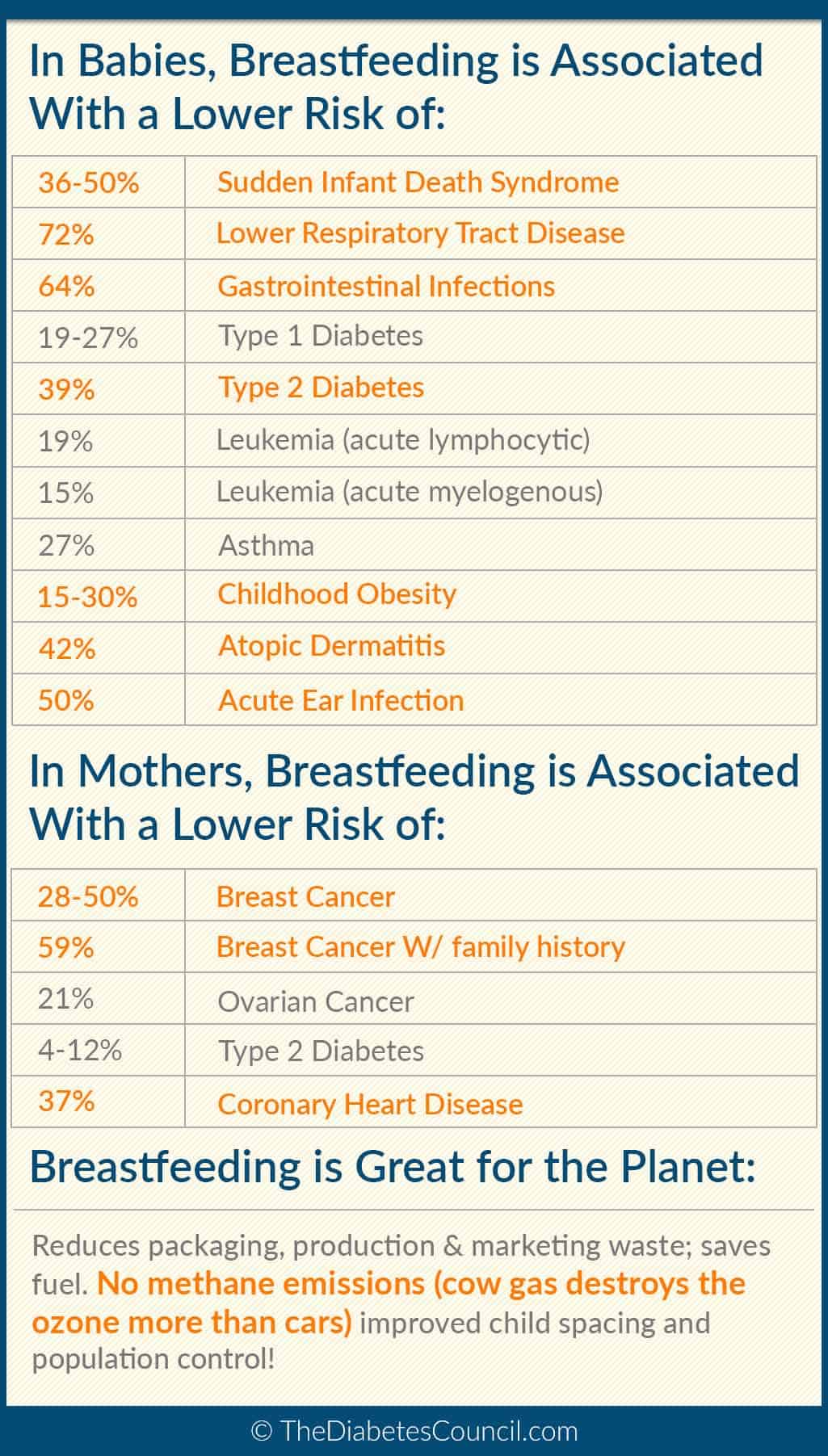
Breastfeeding is very beneficial for the nursing mother as well as the baby. It provides lifelong benefits and can decrease the risk of developing diseases and problems later in life for both of them. For mothers who have diabetes, it can also help them manage their disease and prevent further complications.
Benefits for all breastfeeding moms
Breastfeeding reduces the risk of several diseases for mothers that nurse for 6 months or longer.
These include:
- Heart disease
- Diabetes Mellitus
- Obesity
- Osteoporosis
- Rheumatoid Arthritis
- Ovarian Cancer
- Breast Cancer
- Uterine Cancer
The risk of developing these diseases can be reduced up to 86%! Breastfeeding also releases a hormone that is called Oxytocin. This hormone is responsible for decreasing stress and increasing mood, which can be very helpful to new mothers that need more rest and a boost of confidence.
One study found that for every 6 months that a mother breastfeeds, her BMI (body mass index) is decreased by 1% after she hits menopause. This is wonderful because an increased BMI can lead to many problems including heart disease and diabetes.
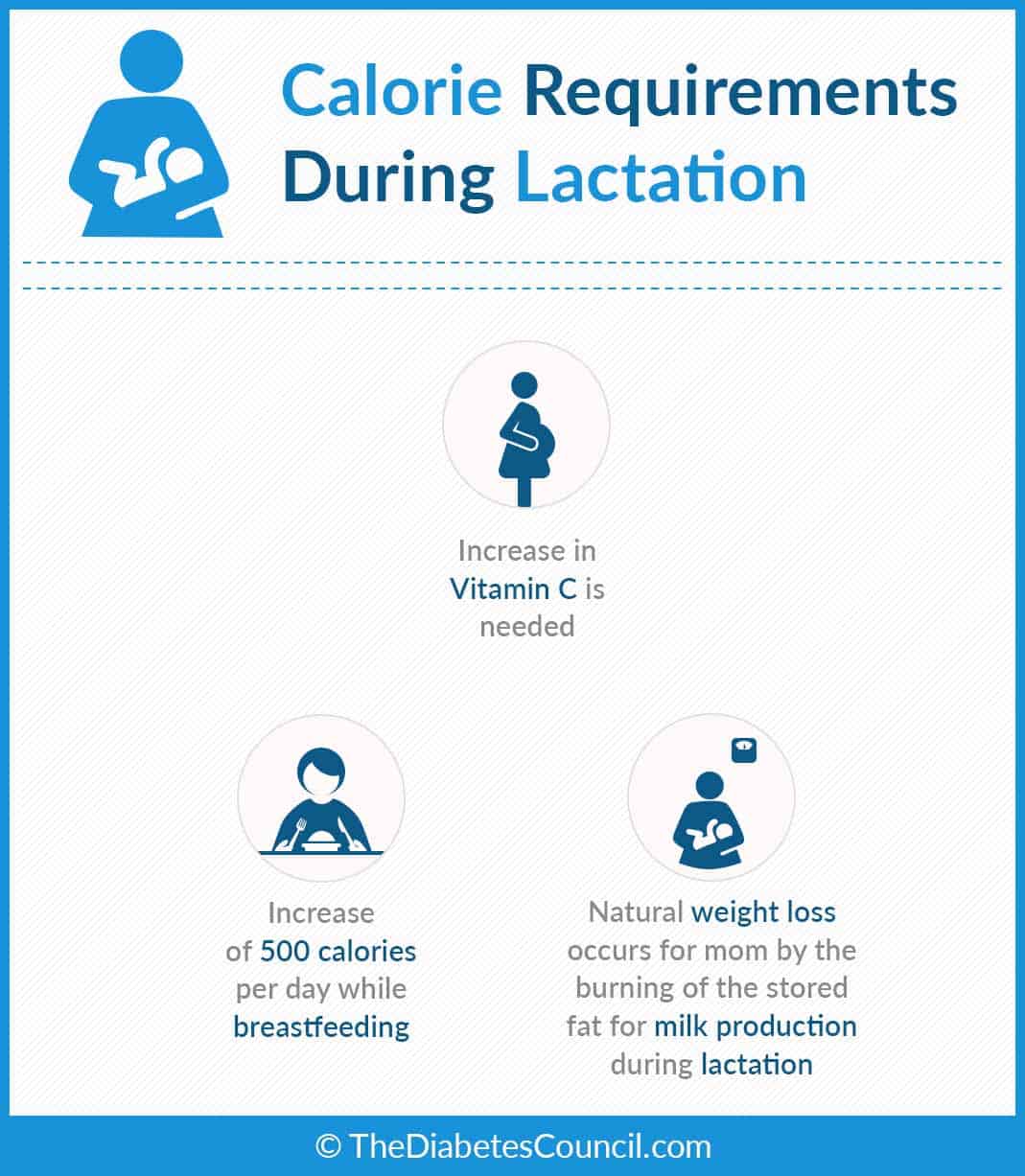
Breastfeeding also burns calories, and it can help the new mother lose the extra weight that was gained and stored during the pregnancy. Reducing the amount of extra weight is beneficial to prevent diseases and problems later in life. It is important to remember to eat enough calories so that milk production is plentiful.
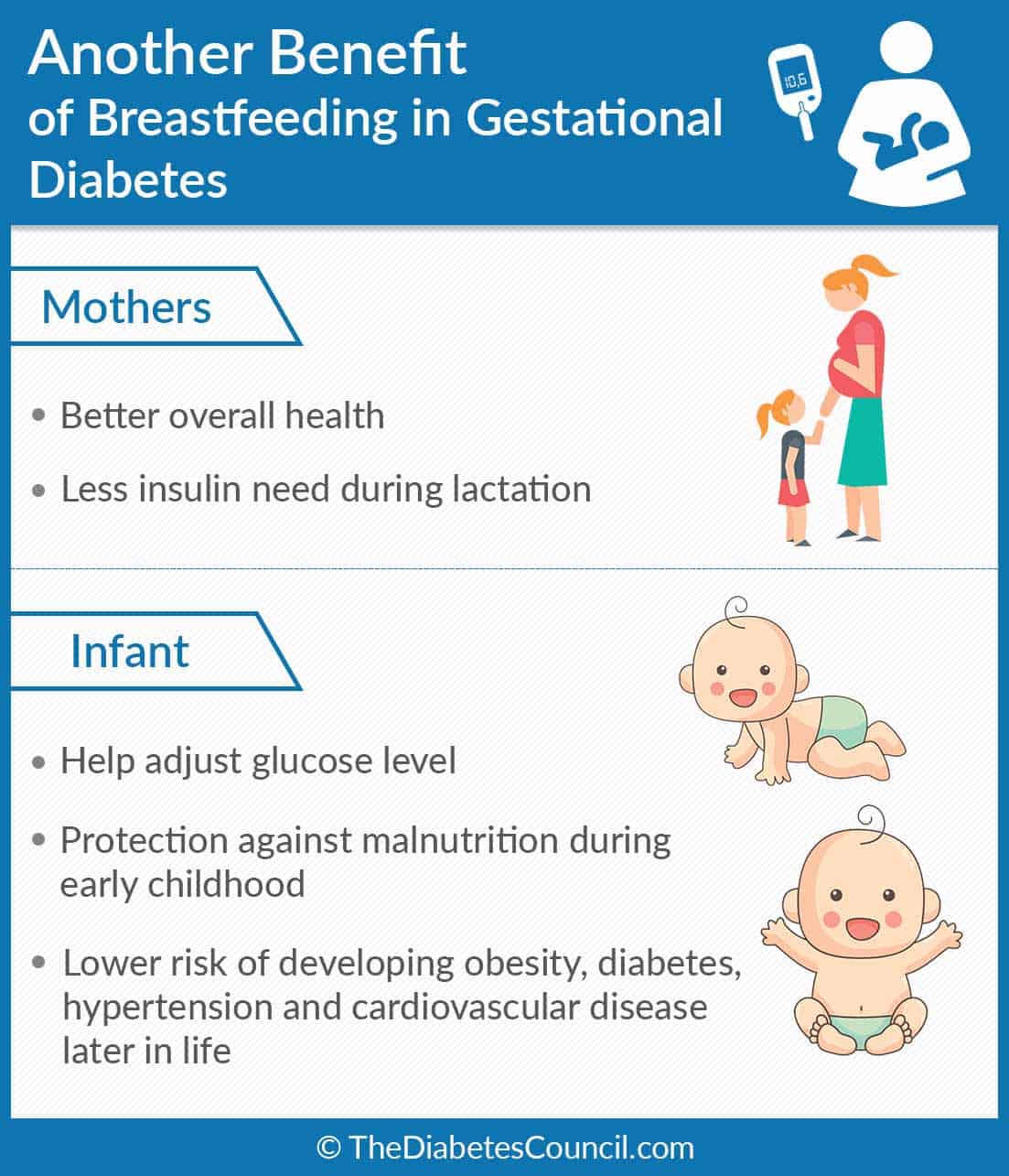
Additional benefits for moms with diabetes
Along with the benefits that are mentioned above, mothers with diabetes that nurse have a few additional perks as well. Because of the additional calorie burn that breastfeeding provides, they may not need to administer as much insulin as they typically would have before nursing. Also, breastfeeding may lengthen the time until their menstrual cycle returns, which brings about the hormonal changes that make good blood sugar control difficult.
Losing the extra weight that comes with pregnancy can help them have better control over their sugars and possibly not need as much medication or insulin. Always talk to your doctor before making any adjustments or changes to your medications.
For the baby
There are many benefits for the baby when they are breastfed. Breastfeeding reduces the risk of many disease in infants such as:
- Obesity
- Type 1 Diabetes
- Viruses
- Infections
- Jaundice
- Sudden Infant Death Syndrome
It provides them with antibodies that make their immune system strong. Breastfeeding also gives the baby more skin to skin contact with the mother, which gives them a sense of security when they are able to bond with their mother.
Can I breastfeed if I have diabetes?
You can most definitely breastfeed if you have diabetes. There are no risks to the baby, and the only risk for the mother is low blood sugar because of the extra calories and energy that it burns.
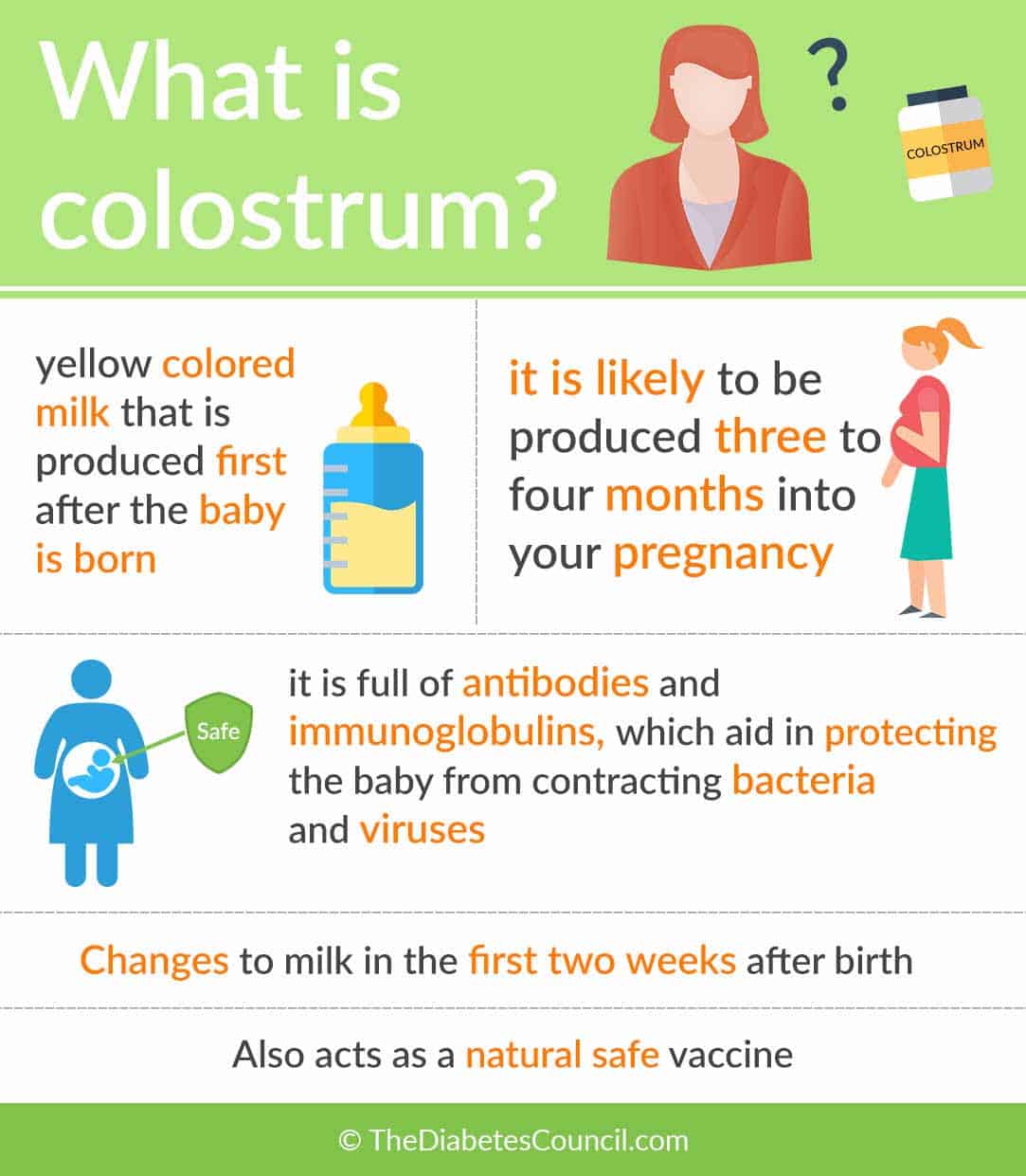
Talk to a lactation consultant about breastfeeding and make sure you educate yourself about all the benefits. You should also look into expressing milk prior to delivery (which is called colostrum harvesting). This milk removed before baby is born may prevent formula supplementation from being needed in the early days. Work with a lactation consultant before baby arrives to learn more about this great option.
Breastfeeding mothers with diabetes are at an increased risk for mastitis, which is an infection in the breast tissue. Make sure that you are feeding from both breasts and notify your doctor if you suspect an infection (symptoms such as fever, headache, chills, body aches, a sore breast or a hard spot in the breast).
Does breastfeeding reduce my risk of developing Type 2 diabetes?
Breastfeeding does decrease the risk of developing type 2 diabetes for both the mom and the infant. A study on breastfeeding mothers found that moms are 15% less likely to develop type 2 diabetes for 15 years after the birth of their last breastfed child.
For the infants, research has shown that children that are nursed have a 40% less chance of developing type 2 diabetes later in life. Breastfed babies are also at a lower risk for obesity, which is a huge risk factor for developing diabetes.
Breastfeeding alone is not enough to take away the entire risk of type 2 diabetes. Lifestyle modifications such as a healthy diet and exercise should still be practiced.
I recommend reading the following articles:
If I have diabetes, will I transfer diabetes to my baby through breastfeeding?
Breastfeeding a baby if you have diabetes does not give them the disease; it protects them! Having high blood sugar adds extra sugar that the baby will consume, which can cause an increase in weight. However, the risk of diabetes is lower for babies that are breastfed than for those that are not. Having great sugar control can help keep your milk just right for your baby.
In fact, in a study conducted 2008, it was shown that the longer a baby was breasted, the loser his/her chances were of developing Type 1 diabetes. As mentioned several times during the span of this article, breastfeeding protects the baby from acquiring infections and other risk factors that may lead to diabetes.
How does breastfeeding affect my blood sugar?
Breastfeeding burns calories. When calories are burned, extra glucose is used in the body. For moms with diabetes, breastfeeding can lower their blood sugar and they may not need as much insulin or medication as they did before they were pregnant.
Nursing mothers that take medication to lower their sugar should be aware of signs of low blood sugar. They include:
- Confusion
- Irritability, anxiety, or emotional changes
- Muscle weakness
- Mumbling
- Clamminess or sweating
- Drowsiness
- Hallucinations
To prevent low blood sugar, nursing moms should keep a snack in their diaper bag as well as one near the areas that they frequently nurse their babies. A snack should be eaten before each nursing session to make sure that the glucose level stays stable. My snack of choice was almonds and frozen grapes. They kept me awake while feeding, but also provided me with good nutrition.
Breastfeeding before the baby arrives
Mothers with diabetes may experience a delay in their milk production right after the baby is born. It is normal and expected. To help with this, it is acceptable to begin to collect colostrum before the baby is born. Colostrum is also called “liquid gold” because of its amazing antibodies that protect the new baby. It can be given instead of formula if baby's blood sugar is low or if the delay in milk production is becoming dangerous for the baby. By having the colostrum on hand, the amount of formula that the baby has to be supplemented with can be decreased or eliminated. Mother's who need to supplement should work with a lactation consultant to develop a feeding and pumping plan.
It is recommended to wait to begin collecting colostrum until 37 weeks of pregnancy. You should not use a breast pump. Only hand express. The following steps are a guide on how to do hand express correctly.
- Step one: Wash your hands, and apply a warm towel to your breast. You can also take a warm shower. This warmth helps the colostrum come out easier.
- Step two: Find a comfortable spot, and gently stroke the breast from the base to the nipple. Place your thumb above the nipple and your fingers below the nipple to make a C shape. (See the photo below for help!)
- Step three: Press in towards your chest, press your fingers together, and then push them forwards. (Below is a great video that demonstrates this.) Colostrum will begin to come out in very small amounts.
- Step four: Using a clean container, such as a medicine cup, collect the colostrum. You should store it in the refrigerator until you are ready to use it. Freeze the stored milk in small batches (1-3 teaspoons per container) after 5-6 days in the refrigerator. Remember to take this frozen milk with you when you give birth.
There are some concerns with hand expressing while pregnant. It can stimulate the uterus to contract, which can lead to a premature birth. This is why you should wait until after 37 weeks to begin collecting colostrum. If you do experience any contractions while hand expressing, you should stop immediately, unless you are full term and close to the baby’s due date.
Breastfeeding after the baby is born
After the baby is born, it is important that you begin breastfeeding right away. This sends the body a message to begin making breastmilk. For those with diabetes, this is very important because they tend to start making it later than mothers without diabetes.
Skin to skin contact is also very important for breastfeeding. It is the act of the baby and mother spending time together without any clothes on.
The benefits of skin to skin contact include:
- It keeps the infant’s temperature regulated
- It helps the baby adapt to the new world
- It helps the baby find the nipple to begin breastfeeding (they are guided by smell)
- It helps the mom make more milk
- It decreases stress and pain from the transition for the baby into the world
- It helps the baby sleep better
- It decreases postpartum depression for mothers
By providing skin-to-skin contact as soon as possible after birth, you are able to give your new baby and yourself these wonderful benefits.
When the baby is a newborn, you should be nursing anywhere from 8 to 12 times in a 24 hour period. It is important that you breastfeed this often for two reasons. First of all, the baby has a very small stomach and digests the breastmilk quickly. Secondly, breastmilk is made on-demand. The more frequently you nurse your baby, the more milk you make!
If you are able to pump in between feedings, it may be a good idea to store some milk for times when your supply is decreased or you have to leave the baby with someone else. Do not skip feedings when you pump. This can decrease your milk supply.
More tips on pumping can be found here: http://www.askdrsears.com/topics/feeding-eating/breastfeeding/while-working/19-tips-better-pumping.
There are some complications that can occur to mothers with diabetes that can hinder the beginning of breastfeeding.
Diabetes during pregnancy can cause an increase in the risk of:
- C-section
- Premature birth
- Jaundice
- Hypoglycaemia
All of these may delay the start of breastfeeding and may lead to the separation of mom and baby. Sometimes the baby needs extra medical care. Many babies are born with low blood sugar. This is because their body has been used to producing enough insulin to keep up with the high sugar of their mom while they were in the womb. To help with this low sugar, babies may need to be given formula, unless the mom has stored colostrum while she was pregnant.
Always use your resources when it comes to breastfeeding. I have breastfed two children, and without the support and advice from a lactation consultant, I don’t know what I would have done. There are also support groups that have meetings.
Check out http://www.llli.org/webus.html to see if there is a support group in your area.
As I mentioned above, breastfeeding has its challenges, but beneficial for both you and the baby. Make sure you are prepared well and have the support to help you on your breastfeeding journey.
How does diabetes affect my milk supply?
There are many things that can lower your milk supply such as stress, not eating enough calories, or not pumping or feeding the baby enough. These factors can be changed. Unfortunately one cause of low supply, which is diabetes, cannot be changed.
After the baby is born, the body recognizes that it is time to start making the real milk that will nourish the infant. It takes 48 to 72 hours (that’s just an average) for this milk to come in. For moms with diabetes, this can be delayed. If there is too much of a delay, then the baby could need formula until the mom is able to produce enough. If there is pumped colostrum, then it can be given instead of the formula.
After the initial let down of the milk, mothers with diabetes are still at a risk of having a low milk supply. One study showed that after the first week of breastfeeding, those with diabetes still had less milk than moms without.
Giving formula to babies increases the risk that they will refuse to breastfeed. For this reason, it is important to try to avoid giving formula. The ultimate goal though is to have a healthy baby, whatever it takes. A fed baby is best.
There are supplements that are marketed to help increase milk supply. Fenugreek, one of the popular ones, should not be taken because it can change your blood sugar. Be sure to check with your doctor and lactation consultant before taking any supplements.
I mentioned stress being a cause of low milk supply and I want to mention it again. Not only is it stressful having a new baby in the house and adjusting to that, but it is also stressful trying to manage your diabetes with all of the changes. When you are stressed, your body stops producing oxytocin. This hormone is responsible for helping the milk release when you are breastfeeding. Relax as much as possible, and avoid things that will cause stress. (I know you are thinking yea right!) Ask for help from people if they offer. Don’t stress about little things, like a messy house or dirty clothes. Focus on your health and the health of your new little baby.
How does breastfeeding affect my diabetes?
Breastfeeding moms should make sure that their blood sugar levels do not drop too low. Breastfeeding uses up extra calories, which also uses up glucose. This risk is even higher for moms that use insulin. Be sure to check your blood sugar before and after your nursing sessions. You should also have a well balanced snack with each feeding.
Along with lowering the blood sugar, it can also lower your weight. You burn approximately 400 to 500 calories a day while breastfeeding. For those with type 2 diabetes, this can overall help your blood sugar control. Make sure that you are eating a diet that is nutritious and that provides enough to support you and your baby. Not eating enough can lead to a decrease in milk supply. A steady diet of protein and carbohydrates is recommended.
During the baby’s growth spurts, they will eat much more than they typically do. You need to make sure that you are paying attention to your blood sugar and that it is not dropping because of the extra calories that you are burning. Your insulin needs may be less at this time as well and you may need to increase the amount of food that you are eating to keep up with the needs of your baby.
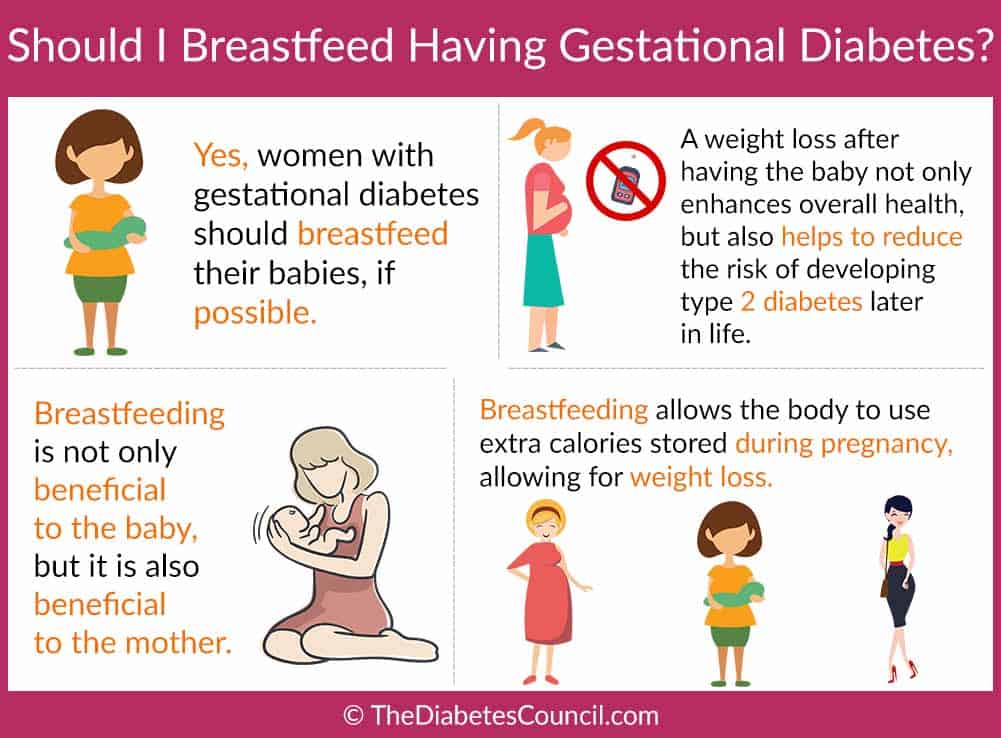
How does breastfeeding affect gestational diabetes?
Gestational diabetes is the term used for a mother that is first diagnosed with high blood sugar levels while pregnant. Up to 9.2% of pregnant women have gestational diabetes. What happens is that during pregnancy, the extra hormones lead to an increase in the sugar in your body. If your body cannot keep up and make enough insulin, then your blood sugars will be elevated. 90% of the time, the mother’s blood sugar levels will return to normal after the delivery of the baby.
This does not happen overnight, and may take a few weeks for it to regulate. Sometimes, having gestational diabetes causes the blood sugar levels in the new born to be low. Breastfeeding helps with raising the levels by providing easily-absorbed glucose.
Babies that are born to mothers with gestational diabetes have a higher risk of obesity. Breastfeeding these infants can lower that risk up to 50%, which can in turn reduce the child’s risk of other diseases later in life such as heart disease and diabetes. By breastfeeding, you can also lower your own risk of developing diabetes later in life. Since nursing burns extra calories, you can lessen your body weight and your risk.
What medications for diabetes can I take while breastfeeding?
The two major medications that are used for nursing mothers are Metformin and insulin. Although, there are some medications that you are not supposed to take while you are nursing because they can cross through the breast milk and affect the infant, these two are safe.
Metformin is a pill that basically tells the liver to stop making glucose and helps the body use insulin more effectively. It can be safely taken while breastfeeding. Studies have been done showing that it does cross through the milk into the infant, but it is in very small amounts. Also, it has not shown to cause any complications to infants that have been exposed to it. (It is very hard to run studies like this because of the possible harm to babies so not many have been done!)
Insulin does not cross into the breastmilk because it is too large. If any did, because it is a natural occurring hormone in the baby, it would simply be digested in their stomach without any problem.
Be sure to talk to your doctor about any medications that you are taking. You should also consult with a lactation consultant about any medications that you are taking while nursing.
Tips for effective breastfeeding
Breastfeeding can be difficult for a new mother without diabetes. (Trust me, I’ve been there!) Adding the extra stress and complications that go along with diabetes can make it seem almost impossible.
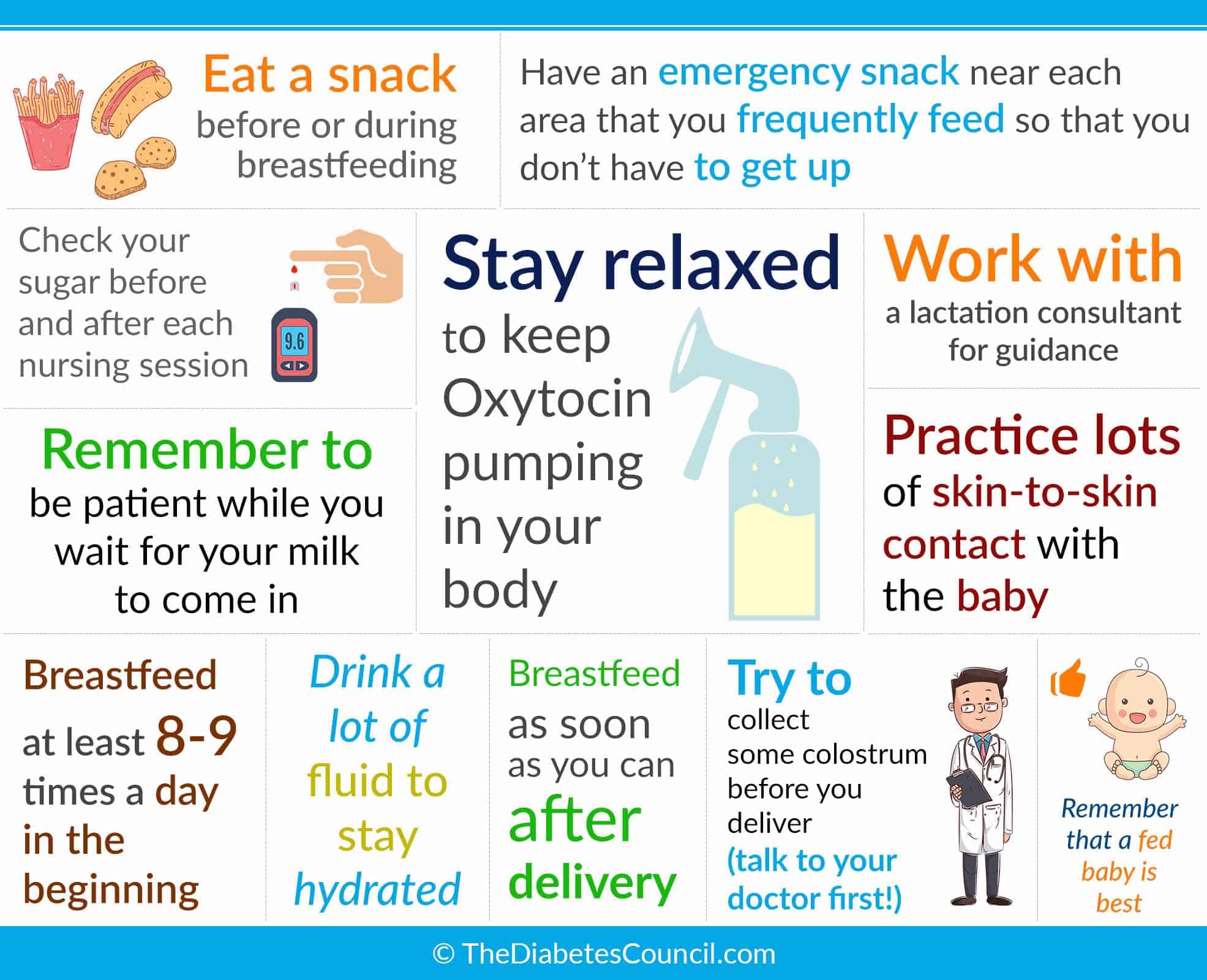
Some tips to make breastfeeding with diabetes easier are:
- Eat a snack before or during breastfeeding
- Check your sugar before and after each nursing session
- Have an emergency snack near each area that you frequently feed so that you don’t have to get up
- Remember to be patient while you wait for your milk to come in
- Stay relaxed to keep Oxytocin pumping in your body
- Work with a lactation consultant for guidance
- Practice lots of skin-to-skin contact with the baby
- Breastfeed at least 8-9 times a day in the beginning
- Drink a lot of fluid to stay hydrated
- Breastfeed as soon as you can after delivery
- Try to collect some colostrum before you deliver (talk to your doctor first!)
- Remember that a fed baby is best
FAQS
Get all the answers to the most frequently asked questions (FAQs) regarding breastfeeding and diabetes.
Why is it important to breastfeed a baby if you have diabetes?
- Colostrum plays a hand in stabilizing the baby’s blood sugar after birth.
- It helps the mother in the weight loss journey post birth.
- The body’s need for insulin is lowered.
- Oxytocin, the happy hormone, is released when a mother is breastfeeding. This ensures the physical and emotional well-being of a mother.
How often should the baby be fed?
Newborns are supposed to be fed on cue at least every 3 hours in the first few days which would make it about 8-12 times a day. At 1 to 2 months old, the baby should be fed 7-9 times a day. With time, they will nurse lesser and lesser.
How can I know if my baby is having a low blood sugar level?
Right after the baby is born, the hospital will take his/her blood sample to measure their blood sugar levels. If the baby’s blood sugar levels remain under 2.0 mmol, he or she will be given expressed milk and artificial milk to help raise the levels.
Is it possible for my baby to have hypoglycaemia after birth?
If you had poor control over your blood glucose, it is likely that your baby might experience hypoglycemia in the first 12 hours after his/her birth. It is important to give your baby skin-to-skin contact and frequent nursing to help increase his blood sugar levels. Colostrum is the best solution to help your baby overcoming this.
Further reading:
Do I need to re-adjust my diet after the birth of my baby?
You will need to readjust your calorie intake especially because nursing burns calories for mothers. You may need to increase your calorie intake by 500 calories (above your pre-pregnancy diet, this equates to approximately 2 healthy snacks per day) during breastfeeding. This also helps in regulating the blood sugar levels.
Breastfeeding is an amazing thing that you can do for yourself and for your baby. However, not everyone’s body will allow them to breastfeed, and sometimes things happen that hinder breastfeeding. If you are unable to, don’t think that you are letting your baby down. You are doing your best (And they grow fast, so soak up the baby snuggles!) If you have any advice or support for other mothers that are nursing or considering it, please share it with other readers in the comment box below!
TheDiabetesCouncil.com would like to thank Kate Cropp ARNP, IBCLC, MSN, Director of Lactation Services at Nashville Birth and Babies for taking the time to review this editorial. If any of you moms have any comments post them down below!
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on May 24, 2020
References
- https://www.diabetes.co.uk/diabetes-medication/metformin-during-pregnancy.html
- http://www.lllc.ca/thursdays-tip-breastfeeding-if-you-are-diabetic-or-insulin-resistant
- http://www.diabetesincontrol.com/breastfeeding-and-diabetes/
- https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/1746-4358-7-20
- https://www.idf.org/sites/default/files/attachments/article_489_en.pdf
- http://care.diabetesjournals.org/content/30/Supplement_2/S161
- https://www.laleche.org.uk/diabetes-and-breastfeeding/
- http://diabetesstopshere.org/2012/08/28/breastfeeding-and-diabetes-whats-the-connection/
- https://www.ncbi.nlm.nih.gov/pubmed/17968982