As an individual with diabetes, you may have experience moments where you feel like you are losing complete control over your emotions and a little thing can make your blood boils.
And if you have a love one who suffers from diabetes, you may probably have witness them slipping into a state where they have flew off the handle and you simply cannot reason with them.
Does diabetes directly cause these aggression fits? The answer to this question can be quite tricky. In order to answer this question, this article will talk about how blood glucose level is closely related to self-control and aggression (often interchangeably known as will power).[accordions id="5494"]
Contents
- Relationship Between Blood Glucose Level and Self-Control
- Physiological Effects of Blood Glucose Fluctuations
- Role of Insulin in the Brain
- Hypoglycemia and Its Effects
- Problem with Recurrent Hypoglycemia Episodes
- Accidental Insulin Overdose
- How to Treat Rapid-Acting Insulin Overdose
- Hyperglycemia and Brain Inflammation
- Problem with Recurring Hyperglycemia Episodes
- Aggression in People with Diabetic Ketoacidosis
- How to Avoid Ketoacidosis?
- Beware of Quick Treatment Complications
- Faulty Fight or Flight Misfire
- Is One Type of Diabetes More Prone to Anger Bursts?
- Are Males with Diabetes More Prone to Violence?
- Psychological Stress on Individuals with Diabetes
- Stress from the Uncertainty
- Facing Stigma of Diabetes
- Stress from Not Receiving the Right Diagnose and Care
- Deadly Combination of Social Rejection and Blood Glucose Swings
- Self-Blaming Turns into Lashing Out at Family Members and Friends
- Frequent Incidence of Domestic Violence
- Family Member Perspective on Diabetes Aggression
- When Enough is Enough?
- Importance of Self-Care to Lessen Aggressive Outbursts
- Add Continuous Glucose Monitor System as Part of Treatment
- Plan for Outburst Situations
- How to Help if Your Love One Is Suffering from Mood Swings
- How to Spot If Your Love One Is Suffering from Clinical Depression?
- How to Handle the Aggression Situation
- Tips to Avoid Slipping into the Unwanted State
- Conclusion
Relationship Between Blood Glucose Level and Self-Control
Blood sugar can make people do crazy things. According to a recent scientific study on the link between low blood glucose level and relationship clashes (Bushman et al, 2014), being hungry makes an individual generally cranky and act more hostile to others. In the study, couples who are hungry tend to have a much higher tendency to exhibit aggression towards each other and become more impulsive in their reactions.
This phenomenon is often referred to “hangry” (meaning feeling angry when you are hungry). If this irritable state can happen to any healthy person who experiences a change in their blood glucose level, imagine the ordeals individuals with diabetes frequently go through on a daily basis. However, do not jump to the conclusion that diabetes leads to aggression. In fact, scientists find a more direct correlation between blood glucose level and self-control.
I recommend reading the following articles:
- Guide to Thiazolidinedione (TZDs) for Type 2 Diabetes
- Experts Share Their Best Tips On How to Cut Calories and Lose Weight
- Continuous Glucose Monitoring: Everything You Need to Know
- Top Must Have Diabetes Supplies
- If I Have Diabetes, Will I Have to Stop Eating Sugar?
In a way, you can visualize self-control as a muscle that requires a lot of energy to sustain so that it does not become ineffective quickly. This energy source comes from the glucose in the blood. So what kind of activities can wear out this “muscle”? Any daily activities that require self-discipline such as forcing yourself to get out of bed early to exercise, resisting from having a soda drink or another cookie with your meal, stopping yourself from smoking, dealing with stressful situations at work and at home, and abstaining yourself from road rage.
As you can see, self-control plays a crucial part in restraining inappropriate and aggressive behaviors. So when people are low in glucose, the self-control mechanism cannot function properly to prevent these outbursts of hostile actions. In a research study, individuals who have drunk a glucose beverage prior to the experiment react less aggressively than those who have drunk a placebo beverage without glucose. Researchers have also found that states in the United States that have the highest amount of diabetes cases tend to have the highest rate in violent crimes. Similarly, countries that have a higher rate of glucose deficiency tend to have a higher rate in violent crimes and murders. All these findings points out that poor glucose metabolism leads to low self-control resulting in higher tendency of aggressive behaviors.
Physiological Effects of Blood Glucose Fluctuations
Although we acknowledge that both type 1 and type 2 diabetes cause detrimental effects on the physical health, lesser information is available to discuss how the disease can cause physiological changes to the brain and take a serious toll on the mental health on people who suffer from diabetes. In the past, neural scientists have noticed that the neural blood vessel functioning drops significantly due to diabetes.
This physiological change lowers cognitive skills and hinders on the ability to perform daily activities. This change also leads to an increase in blood inflammatory markers and C-reactive protein (2 important indicators for risk of developing dementia), as well as a general increase of cortisol secretion and higher blood pressure. What is more important is that recent clinical cases have proven that extreme fluctuations in blood glucose level produce the most damage in the brain and contributes to the sudden onsets of aggressive behaviors. That means hyperglycemia and hypoglycemia can both be responsible for triggering these temper tantrum episodes.
Role of Insulin in the Brain
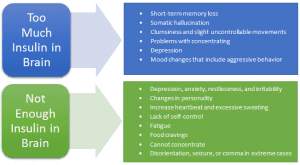
One factor that many people fail to acknowledge is that insulin actually has several crucial jobs in the brain that is responsible for controlling food consuming and various cognitive functions such as memory formation and self-control. Believe it or not, there are insulin receptors in the olfactory bulb and thalamus.
Aside from regulating food cravings, the thalamus plays a vital role in self-control, sensory information filtering (visual, auditory, touch, and smell), arousal, alertness, and wakefulness. So either too much or too little insulin in the brain can cause the thalamus to not function properly.
Without sufficient insulin in the brain, the thalamus will not be able to properly regulate self-control of emotions and food cravings. In extreme cases of insufficient insulin in the brain can lead to coma. On the other hand, too much insulin in the brain can cause amyloid protein buildup (also known as brain plaques). The accumulation of the plaque increases the chance of memory loss, and developing dementia, Alzheimer’s disease, and Huntington disease.
Hypoglycemia and Its Effects
The brain depends on glucose as the essential fuel. When there is not enough glucose in the brain, the neurotransmitters will fail to properly transmit chemical signals to the neurons. Consequently, hypoglycemia results in poor attention span and faulty cognitive functioning. A lot of individuals with diabetes have experience hypoglycemia at some point in their journey of treating the disease.
Sometimes the condition is cause by simply not having enough blood glucose in the body. Other times, it is cause by skipping a meal, accidental insulin overdosing, excessive alcohol consumption, long periods of intensive exercise or physical activities, illnesses, certain hormone deficiencies due to adrenal and pituitary gland problems, intake of certain medications, or even insulin overproduction due to pancreas tumor. It is important to note that each person experience the symptoms in variations. Early signs of hypoglycemia can include:
- Tingling feeling around the mouth and limbs
- Heart palpitations
- Feeling tired and/or hungry
- Easily Irritable and/or agitated (similar to people who are in the “hangry” situation)
- Mumbling and crying out during sleep
- Sweating and/or pale skin
- Shakiness in coordination
If the hypoglycemia condition is more serious, these symptoms can occur:
- Confusion
- Nausea
- Blurred vision
- Lack of concentration and difficulty in doing daily routine tasks
- Dizziness
- Rapid heartbeat and/or angina pain
- High blood pressure
- Exhibit behaviors similar to being intoxicated with slurred words and clumsy movements
- Episodes of seizures
- Become unconscious
For people who are sensitive to the low blood glucose level condition, they may become delusional and even aggressively violent. When others try to assist them or treat them of hypoglycemia, they can become abnormally combative. If you are one of these individuals, you should know your warning signs of hypoglycemia and seek treatment before your condition deteriorates into a situation where you and your family members can get seriously injured. If your hypoglycemia condition is left untreated in a timely manner, you are increasing your chance of brain damage and heart attack.
Problem with Recurrent Hypoglycemia Episodes
Recurrent hypoglycemia is a common complication for both type 1 and type 2 diabetes. It has been shown that this problem can lead to impaired memory, changes in cognitive reasoning, increase risk of depression as well as other mood disorders.
It as been suggested by many researchers that recurring experience of low blood glucose can affect or even damage the amygdala (the portion of the brain that is mainly responsible for the fight or flee mechanism and controlling the secretion of cortisol). Another problem is that in face of an aversive stimulus, the amygdala will stimulate an increase of glucose metabolism and elevate the cortisol level in the body.
This may push the hypoglycemia state into an even more dangerous state. The elevated amount of the stress hormone can also explain why individuals who suffer from recurrent hypoglycemia have a higher chance to become aggressive when they experience low blood glucose. Over the time, the overworked amygdala will constantly demand more glucose to function properly. As you can see, this can cause a vicious cycle between hypoglycemia and amygdala malfunctioning.
Accidental Insulin Overdose
Sometimes you may overcompensate on your insulin injection and become hypoglycemia. Symptoms of insulin overdose can include:
- Anxiety, irritability, and restlessness
- Depressed mood
- Changes in personality
- Profuse sweating and inability to concentrate
- Tingling sensation
- Disorientation and unsteady movements
- Hallucination
- Seizure
- Comma
How to Treat Rapid-Acting Insulin Overdose
Depending on how quickly you have realized the problem, here are several ways to treat an insulin overdose:
- If you discover the error 20 minutes or more after the insulin administration, take some fast-acting glucose (e.g. sugary drink or glucose tablets) as soon as possible. Afterwards, gradually take in a sufficient amount of slow-absorption carbohydrates to counter the overdose. Remember not to take in too much glucose all at once or else you may suffer from brain swelling from the intense blood glucose fluctuation.
- If you discover the error within 20 minutes, administer small amount of fast-acting glucose follow by small amounts of slower-absorbed carbohydrates. If the overdose is not severe, you may not need to take the fast-acting carbohydrate. But remember not to eat any fatty food as it slows down the metabolism of carbohydrate.
TIP:
In general, each unit of insulin requires about 10g of carbohydrate to balance out the effect. When you are treating an insulin overdose, it is safer to have too much carbohydrate than not having enough. While you are treating the overdose, test your blood sugar level frequently to make sure the level is stabilizing.
NOTE: If the overdose amount is large, immediately treat with fast-acting glucose tablet. Call your physician or the emergency hospital helpline for further assistance.
Hyperglycemia and Brain Inflammation
Although hypoglycemia is known for causing violent behavior, hyperglycemia can trigger aggressive outburst as well. Even though glucose is a necessity for the proper functioning of the brain, too much glucose can be deadly. Having hyperglycemia can also make you uncomfortable, antsy, and grouchy.
Health studies have found that frequent hyperglycemia episode in type 2 diabetes women are associated with a general lower quality of life and higher frequency of depression. Clinical studies have shown that extreme high blood glucose can cause damage to the hippocampus and leads to cognitive problems. During hyperglycemia, patients exhibit a common symptom of having lower verbal skills as well as lower overall IQ scores when compared to their performance in normal circumstances. In extreme cases, hyperglycemia can actually sever connections within the brain to produce brain atrophy and neural cell deaths.
In addition, the condition can cause restriction of blood flow in the brain to cause cognitive impairment, hallucination, and temporary inflammation reaction. This short-term inflammation can trigger an onset of impulsive aggression and hostile behaviors such as road rage and domestic abuse. Here are some early symptoms of hyperglycemia attack:
- Mood swings
- Easily irritable
- Tearfulness
- Difficulty concentrating
- Generally cranky
- Personality changes
- Complain about being tired
- Frequent urination
- Sudden sense of thirst
- Blurred vision and decreased visual acuity
- Headache
- Problem with reasoning
- Problem with speech
It is important to note that not all individuals with diabetes will exhibit aggressive behavior during episodes of hyperglycemia. But if you or your love ones does suffer from such problem, it is crucial to know of the specific early symptoms of high blood sugar level.
If you or your love one detect any of these symptoms, it is the safest precaution to perform a blood glucose test and treat the problem as soon as possible. If the hyperglycemia condition is too severe, contact your doctor or the emergency hospital hotline for immediate medical assistance to prevent ketoacidosis and other complications (e.g. kidney damage, nerve damages, development of eye diseases such as glaucoma, heart problems such as heart attack or stroke).
Problem with Recurring Hyperglycemia Episodes
If hyperglycemia occurs frequently, the recurrence of the inflammation state can produce psychomotor retardation, depression, appetite loss, and slower metabolism. Recent clinical studies have found abnormal elevated amount of blood glucose has a toxic effect on neurons due to several reasons.
The first reason is that it causes an increased production of other enzymes and proteins. One of the most dangerous protein to accumulate in the brain is the amyloids. In abnormal high amounts, it can build up in the brain and become what is known as “plaques”.
During an episode of hyperglycemia, the increased amyloids can prevent memory formation and decrease cognitive functioning. When high blood glucose becomes frequent, the amyloids will actively block the neurons from functioning properly and eventually cause the affected neural cells to die off. Consequently, the problem greatly increases the chance of developing Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and dementia.
Another problem with recurring hyperglycemia is that the increased amount of blood glucose level will also increase amount of cortisol secretion and cause an elevation of blood pressure. These diabetic individuals are prone to be easily irritable and have a tendency to exhibit poor working memory and short term memory. Over the time, if an individual is exposed to high blood glucose level repeatedly, these complications can drastically increase the chance of developing vascular dementia or Alzheimer’s disease. In addition, repeated hyperglycemia episodes have shown to significantly increase the risk of brain aneurysm.
Aggression in People with Diabetic Ketoacidosis
Diabetic ketoacidosis is a life-threatening complication that occurs when an individual accumulates a high level of ketones in the body. These are the common causes to the problem:
- Consumed too much glucose and fail to treat hyperglycemia. This can happen to individuals who do not keep to an eating schedule and have a tendency to binge eat.
- Not enough insulin is the most common cause of high ketone level. For individuals who require constant changes in their treatment regimen, this is often the main cause of ketoacidosis. Another common reason for not enough insulin is insulin resistance.
- Taking certain medications that affect the blood glucose level and insulin level. An example is corticosteroids used for treating infections.
- Exercise too much without adjusting insulin dosage. A sudden increase of physical activities may cause an influx of ketones in body.
- Serious infections can increase the amount of ketones in the body and subsequently lead to ketoacidosis. Illnesses that cause high fever, diarrhea, and/or vomiting have the highest risk of triggering ketoacidosis.
Although ketoacidosis happens much more often in people with type 1 diabetes, it can also occur with type 2 diabetes individuals as well (especially children). For many people, violence and hallucinations are not part of the reaction of ketoacidosis. Many people have the tendency to act catatonic from the confusion and extreme lack of energy to move. However, for the glucose fluctuation sensitive individuals, they may become impulsive and aggressive.
Many times these patients actually exhibit these psychotic symptoms shortly after being treated for ketoacidosis and regained consciousness. Many doctors have suggested that it is the sudden blood glucose swings due to the treatment is the cause of the temporary aggressive psychotic behaviors. Because of the sudden change in blood sugar, it may trigger a condition of cerebral edema (the brain swells from the fluid buildup in brain cells). It occurs most frequently in children with type 1 diabetes.
How to Avoid Ketoacidosis?
To avoid going down the vicious cycle of experiencing this complication, the best way to avoid ketoacidosis is to spot the symptoms and put an early stop to the problem by treating the condition as soon as possible.
Early symptoms includes:
- Frequent urination
- Extreme thirst and/or dry mouth
- High ketone levels in urine sample
- High blood glucose level
- Feeling heavy and tired
- Flushed skin
- Abdominal pain
- Nausea and/or vomiting
- Breathing problem
- Breath smells “fruity- ”
- Abdominal and back pain
- Lethargy
- Mind fog and/or difficulty concentrating
Another way to avoid ketoacidosis is to actively engage prevention habits. Usually, your physician would recommend daily ketone tests if your blood glucose level is 240 mg/dl or more. But if you know that you are prone to ketoacidosis and aggression tendencies during these situations, you should tests your ketone level several times throughout the day. At the same time, eating regularly, keep yourself hydrated, keep your immune system up to avoid getting sick, and stay away from caffeine and alcohol.
Beware of Quick Treatment Complications
As mentioned earlier, sudden big changes in blood glucose level can be deadly. A problem that is rarely mentioned is the effect of adjusting your blood glucose too quickly. This change can actually cause your brain to swell and suffer from temporary inflammation state (it is especially common in children who are newly diagnosed with diabetes).
The swelling can cause the brain to misfire and bring about aggressive behaviors. Although you should treat your conditions as soon as possible, you should be aware that taking all the insulin and medications too quickly can lead to complications that may make you agitated physically:
- The medication and insulin can lead to a drop in your potassium level (also known as hypokalemia) and impair the functioning of your brain and nerves. You may experience brain fog, fatigue, and confusion.
- The sudden fluctuation in your blood glucose level and the rapid adjustment can make your brain swell (a condition referred to as cerebral edema). This complication can cause hallucination appears more often in children than adult.
Instead of making all the adjustment at once, you will want to administer the insulin in several doses so that you can gradually adjust to the changes. Have a talk with your doctor and
Faulty Fight or Flight Misfire
Another issue that many people may have overlook is the change in cortisol level and blood pressure changes because of the onset of blood glucose imbalance and the treatment given too aggressively and too quickly. When your blood glucose level swings into abnormal level, your body automatically respond by increasing the cortisol level. So when you pair the physiological stress, the onset of all the physical discomfort, elevated blood pressure, and impaired thinking (and sometimes hallucinations), you create the perfect scenario of becoming aggressive and hostile.
Is One Type of Diabetes More Prone to Anger Bursts?
In the past, some researchers have tried to establish a link between diabetes and violent crime such as robbery, rape, and murder. Obviously, the claims are highly flawed.
But based on reports of patients behaving viciously towards others, we can see that some diabetic individuals are more prone to violent acts than others. The question everyone may wonder is whether one type of diabetes is more prone to trigger the onset of temper tantrums and sudden rage behaviors.
Although there are many more clinical case records of type 1 patients exhibiting aggressive behavior and violent acts towards other people, there is not a direct correlation between temporary rage and type 1 diabetes. As we have discussed earlier, type 2 diabetes patients can fall into a sudden rage as well. According to clinical studies, type 2 diabetes with frequent hyperglycemia episodes tend to have a higher risk of developing depression. In fact, they also have a higher tendency to exhibit psychiatric disorders than those with type 1 diabetes. Instead of pointing fingers at either type 1 or type 2 diabetes patients, we must establish several facts:
- Long-term diabetes (both type 1 and type 2) causes serious damage to the brain and disrupts the functioning of neurons.
- Unique sensitivity to insulin and blood glucose fluctuation is a key to the onset of aggressive behavior.
- Intense blood sugar swings cause by treatments can cause an onset of psychotic episode.
- As mentioned earlier, the amount of insulin in the brain can play an important role in anger bursts.
- Cortisol and blood pressure fluctuations can play a role in contributing to the rage factor. And similar to insulin sensitivity, each person reacts differently to the change.
- The patient’s control of their blood sugar level is an important contributing factor. Those who suffer from a lack of control and experience frequent fluctuations tend to have a higher tendency to exhibit hostile behavior and verbally abusive behavior.
- Each person’s psychological stress has to be taken into account of whether they can become more susceptible to become depressed, anxious, and hostile.
Are Males with Diabetes More Prone to Violence?
No. Anyone can exhibit aggressive behavior given that they are sensitive to blood glucose level and insulin fluctuations, feeling anxious and depressed, suffering from hallucination, and sensing that their current situation is threatening. As a matter of fact, some women have shared their outburst experience on the forum.
Many of them are small size women who tried to fight off their spouses or paramedics that are twice their size and showed superhuman strengths. Although amusing in hindsight, it is terrifying for anyone to go through that experience themselves and a tremendously stressful situation for their family members who have to suffer through the biting and scratching.
According to clinical case studies, children are actually most susceptible to exhibit violent behaviors during severe hypoglycemia, hyperglycemia, and ketoacidosis incidents. This is because they are more sensitive to the blood glucose fluctuation, and they are prone to cerebral edema and electrolyte imbalance. The children’s less toleration of pain and discomfort may also contribute to their tendency to lash out.
Psychological Stress on Individuals with Diabetes
Aside from the physiological relationship between blood glucose level and aggression, many people overlook the psychological factors that may contribute to the problem. As a matter of fact, diabetes can set up the perfect foundation for anger issues. Just the diagnosis result of having diabetes can trigger the loathing question, “Why me?” The uncertainty and fear why this is happening to you, whether you can get better, what you need to know about the disease, and what lifestyle changes you need to make all add up to a massive emotional burden.
As the medication dosage can be a trial and error adjustment routine, you can feel completely hopeless that no matter what changes you make, you do not seem to feel better or lose any weight. In addition, any lifestyle habit changes qualify as stress factor in life. The sudden need to make so many changes when you are not feeling well can make you feel like you have been thrown a curveball in life. All these factors can make you feel anxious and depressed.
Stress from the Uncertainty
Uncertainty in life and what lies ahead can be daunting. Many people with diabetes struggle with a lot of fear:
- Fear of what you do will affect your blood glucose level,
- Fear of when the next hypoglycemia or hyperglycemia may occur,
- Fear of experiencing complications when you are out in public,
- Fear of losing your job due to disclosing your condition to your boss and coworkers,
- Fear of not receiving medical help in a timely manner and result in brain damage, coma, heart attack, or even death, and
- Fear of causing an embarrassing situation in which you may harm yourself, your love ones, or even strangers who come to your aid. All these worries can deter individuals from enjoying social events and become easily depressed,
- Fear of rapid health deterioration and how your life will become,
- Fear of asking for help.
Clearly each person has their own levels of fear when they are diagnosed with diabetes and learning more about managing their symptoms. However, those who perceive their fears as more life threatening will have an increased chance of being moody and angry in general. For older patients who have recently been diagnosed with type 1 diabetes, the fear of asking for help and clarify how to use certain equipment is a common cause of hostility towards friends and family members. Those who are not technology-inclined can find their situation overwhelming.
They may try to ignore the issue, refuse to follow the doctor’s instructions and check their blood glucose regularly, and they may try to deal with the psychological stress in their own way by engaging in binge drinking, chain smoking, and excessive drinking. All these activities only make the problem roll into a bigger snowball.
Facing Stigma of Diabetes
Many, if not almost all, individuals with diabetes have come across this situation where someone tells them that they cannot eat certain food because it has sugar in it or they can “get well” by simply losing a few pounds. There is also the stigma diabetes is the result of people who pig out on food, always sit in front of the television and never exercise, and simply being lazy. Another major misconception is that the patients are responsible for being overweight. What people do not know is that underlying health problems can be the cause of the weight gain instead.
Yet individuals with diabetes have to constantly defend themselves from the social rejection and prejudice. Under such social pressure, it is very hard to stay positive. There are certainly moments where one feels that they loathe themselves, the disease, and the society. After constantly feeling being judged by others and trying to defend themselves in face of the peer pressure, many diabetic individuals may decide to emotionally shut down from the society and keep to themselves. Under such social isolation, these individuals are at the highest risk to suffer from loneliness, social anxiety, anger, and depression.
She took it harder than I did, I think. I have always been obsessed with my weight. Because I was overweight as a kid, and it really affected my self-esteem and self-image. So after about a year of control my levels perfectly, I started purposefully not injecting because I was afraid I would gain all that weight again, and I was willing to do anything to keep it off. It all went downhill from there because the not injecting turned into me eating excessive amounts of food without injecting, among other things and it led to me being hospitalized last year with DKA.
Stress from Not Receiving the Right Diagnose and Care
The regular patient tend to put their trust in their doctors’ hands figuring the doctors are always right. However, with a busy schedule and overwhelming number of patients to see every day, your doctor may overlook certain symptoms, give the patients the “standard” initial treatments, and even misdiagnose the problem based on their previous experience with diabetes.
One of the common problems is misdiagnosing a patient as type 2 diabetes when they actually suffer from type 1 diabetes, or vice versa. Consequently, the treatments does not seem to work no matter how hard the patient stick with the directions. At the same time, the patients unintentionally withhold certain information may lead to misdiagnose or problems with the treatment plans.
Deadly Combination of Social Rejection and Blood Glucose Swings
When the physiological problems of blood glucose fluctuation mix with the psychological traumas of social rejection, it can make any patient more anxious and cranky. It is even worse when the patient feels that their concerns are not being paid attention to by their physicians and family members.
In many diabetes forum, many members have expressed that they feel completely lost and isolated in the initial stage of treating their health problems while the brain fog and inability to concentrate make any changes and following directions make all the negative feelings amplify in their mind. According to health studies, individuals who are perceiving a situation as stressful and hostile, their reaction to rejection will be much more intense and hostile versus individuals who perceive the same situation as non-threatening. In addition, those who are rated as more sensitive tend to react more aggressively towards rejection than people who are less sensitive.
Self-Blaming Turns into Lashing Out at Family Members and Friends
Self-blaming is often a common issue for diabetes individuals. After being diagnosed of the health problems, they often think that they responsible for letting themselves get so unhealthy.
Whenever their blood glucose swings out of control, they feel that they are responsible for what happened and they should have done a number of things to avoid this situation. So when family members or friends make a negative comment how they should have done a certain things or certain lifestyle changes should be easy to accomplish, it is almost like kicking a person after they fall down. Fueled with psychological stress and pain, the individuals see the situation as threatening and stressful. When combined with the blood glucose fluctuation, the increased cortisol secretion, elevated blood pressures, and the psychological need to defend themselves, these individuals can quickly become combative and begin lashing out at their family and friends.
Frequent Incidence of Domestic Violence
Many people with diabetes have shared their nightmarish experience of themselves or their love ones going through one of these delirium episodes. In almost all these stories, the diabetic individual regards the helper as someone who is trying to harm or kill them (e.g. alien trying to abduct them, spy trying to kill them, zombie attempting to eat their brains, ghost trying to suck the soul out of their mouths).
As a result, the individual fight back in the most vicious way that includes any violent maneuver you can imagine. A lot of these stories also have a common ending where the individual is arrested for domestic violence. These experiences are stressful and damaging to spousal relationships. It makes both parties constantly fear of the next violent attack. For the diabetic individuals, they feel embarrassed about how they behaved and shameful of what they have done to their love ones. As much as they have no intention of harming the people around them, they cannot make a promise that such situation will not happen again in the future.
Family Member Perspective on Diabetes Aggression
My husband has recently been diagnosed with type 1 at the age of 42. This means a complete lifestyle change and having to deal with needles, testing and trying to understand what the doctors tell you to do. He was given 2 pens and told to get on with it! Unfortunately and with good reason, my husband if finding it really hard to cope.
He struggles to manage his levels because he won't test regularly, he doesn't eat 3 meals a day to sustain his levels and what he does eat is a load of crap!! He spends most evenings lately hyperglycemic and this makes him aggressive and hard to be around as he just wants to pick an argument. He will go off in our car ( which I desperately try to stop but get screamed at) and I won't be able to contact him to find out where he is and if he is safe. He will return late, say he has been asleep and doesn't remember why he has left.
My son manages his diabetes ok but now and again (after sports or alcohol) he has no warning hypos and can become very aggressive. He has just text me to say he had one in work. He played football last night and I was not at home to make him some food. He knows he has to alter his novomix on occasions like this. When he has hypos at home I give him glucogel, this works pretty quickly. My concerns are if he has aggressive hypo when outside on a night ect. What would happen? I have a fear that someone will beat him up or he will be arrested as he does become quite frightening. He has never hurt me but he is a 6' 2 tall and he hits himself in his head or he will throw things and punch the walls. He never remembers when he comes out of it and is always remorseful that he has frightened me. I feel so sorry for him but I have to pick the right time to talk to him about it. He lost his career in the Royal Navy when diagnosed, it took him so long to come to terms with the fact he has this bloody awful illness.
My son was diagnosed 4months ago.
He seems to be suffering from this uncontrollable rage since his diagnosis and it is really taking a toll on us. We don’t know what to do for the best.
It is so hard because I feel so sorry for him and wish I could take it all away. But at the same time, he has to know his behavior is not acceptable either. He has just started to see the psychologist.
It really is tearing us all apart.
For the spouse and family members, living with such an individual can be extremely stressful both physically and psychologically. They are trying to help but it seems that all their suggestions and reminders have fallen onto deaf ears. Even worse, they have to face a very angry spouse who become verbally combative and unpredictable. It is as if someone else has replaced their spouse with another person overnight. Over the time, the family members can feel extremely helpless that they cannot offer the appropriate help. The repeated abusive situation can even make the family members become anxious, depressed, and exhibit symptoms of PTSD.
When Enough is Enough?
Everyone has a right to get angry to express their feelings and worries. However, it is never okay for anger to be expressed through violence whether it is physically or verbally. If the actions hurt or scare the spouse or family members, this behavior becomes domestic abuse.
Physical domestic abuse includes any physical contacts such as pushing, shoving, grabbing, slapping, hitting, and any other actions that results in bodily harm. Verbal abuse is when a person threatens, intimidates, scares, and/or belittles their spouse to a point that causes the spouse to feel threatened for their personal safety and that they are under constant psychological stress and trauma.
Whether the patient fully intents the behavior or not, if you feel that you can no longer handle the abusive situations, you must speak up and tell someone you trust whether the person is a friend, your family physician, the patient’s medical team, a counselor, a social worker, or even law enforcement if necessary. If you feel uncomfortable telling people around you of the problem, you can always call the domestic violence hotline for assistance.
United States National Domestic Violence Hotline: 800-799-SAFE (7233) or 800-787-3224 (TTY). They are available 24/7.
I am 32 and my partner is 33 we have two children together 2 and a half and six months. He has had type 1 diabetes since he was six years old.
He has never really looked after himself particularly well in that he does not do blood tests unless he is asked and then only reluctantly. Before we had children, he did not even have a testing machine. He only goes to diabetic appointments if I make him go and he always underplays the severity of his hypos. He has hypos where he needs intervention and he is unaware what’s happening at least twice a month on average, mostly during the night. He has never been offensively aggressive until this week but he is often very defensively physical when we try to give him sugars and he seems to have superhuman strength during these episodes. He gets annoyed if I tell anyone he has diabetes and he never tells me about hypos at work when they happen, or his parents’ house or anywhere. He seems to always be in some state of denial about his health problems.
Last Sunday the hypoglycemia condition went to a new level. He woke me by grabbing me by the hair shouting bi**ch and punching me in the head repeatedly. I could not get through to him or stop him and he severely beat me. I thought I was going to die and all I could think was to keep him away from the children, the youngest had been sleeping in the bed next to me and she took a knock though thankfully she is fine. I managed to get away, unlock the front door and bang on our neighbors door that is right next door, I think the cold air may have brought him round to some extent because he seemed to realize then that he was low and something was happening. By this point, I had had punches all over my head and large clumps of hair ripped out where he was grabbing me. fortunately our 2 year old didn’t wake up when all this happened because I was screaming for help and he was punching me, no idea how we could ever explain that if she had seen it.
Do not accept that the behavior will go away eventually because it usually becomes worse. Talking about the problem and actively seek for help is the only way to find a solution to the diabetes anger attacks. If your love one was in denial of their health problems and they possess a threat to others in the family, this is a wake up call for the individual to take their health more seriously for both their benefits and for the safety of the rest of the family. However, if the person continues to be in denial, you must make the initiative to prevent further violence from happening. It is a rough line to walk, but you cannot help the individual if you are seriously injured yourself.
Importance of Self-Care to Lessen Aggressive Outbursts
Individuals with diabetes have a lot on their plates. Many people have shared their stories on forums. In many stories, the individuals state that the most frequent episodes of aggressive behavior actually occur before they are diagnosed with diabetes or in the very early stages of treating their blood glucose level.
But once they nail down their regiment and become better at their management skills, these outbursts become rare occurrence. Although they may still experience moments where they become grumpy and irritable, they are still reasonable and manageable.
Add Continuous Glucose Monitor System as Part of Treatment
For patients who are having a tough time levelling their blood sugar or suffering from insulin insensitivity, even when they follow everything as instructed by their physicians and do everything in their power to prevent blood glucose fluctuations, there are always unexpected situations that can trigger hypoglycemia or hyperglycemia. A solution for this problem is to use a continuous glucose monitor system to keep track of blood glucose level and alert of any unstable activities.
In a study of implementing the device as part of treatments for type 1 diabetic children who are sensitive to blood glucose fluctuations. The parents of these children all have reported severe behavioral changes and temper tantrums due to hyperglycemia. After wearing a continuous glucose monitor to keep track of their blood glucose level, these children have a greatly decrease their tendencies to experience fluctuations in their blood glucose levels.
This also results in much less tendency for the children to exhibit aggressive behavior. Adults who experience violent behavioral changes due to blood glucose fluctuation have also noted the great benefits of using continuous glucose monitor systems. In almost all cases, they are relieved that they no longer need to constantly worry about their blood glucose level and they can finally concentrate on other things in their lives. As some of these system can be synced to smart devices, family members and spouses can also feel less stressed out knowing that the patient is safe and only a phone call away from help.
Plan for Outburst Situations
It is never the individuals’ intention to be aggressive, but accidents happen. If you worry for the safety of your love ones, you, your family members, and your medical team should have a thorough plan on how to manage the situation. If you are the person who suffers from such tendencies, share with them of your own experience, whether you have certain hallucination during the outburst, and what are the certain things that triggers your sudden hostility. Communication is the key.
How to Help if Your Love One Is Suffering from Mood Swings
Diabetes is like having a mold problem in the house. One person can clean the mold all they want in hope to get rid of the problem. But unless the rest of the family help by changing certain habits to inhibit mold growth (e.g. open window to air out bathroom after showering, not leaving wet socks in laundry baskets, taking half-eaten sandwiches out of schoolbags…etc.), the mold will persist and keep coming back.
If you wish your love one to stop suffering from these terrible mood swings, blood glucose fluctuation, and physiological brain complications, you need to be part of the team as well. That means you need to change with the team. If your love one has taken the initiative to eat healthy and cut out donuts from their diet, do not bring donuts into the house late at night to tempt their self-control. That can only end with breaking the new habit or a cranky spouse. Embrace a healthier life with them and treat the opportunity to start a healthier lifestyle as a whole family.
And instead of being part of the society and dumping your love one down, listen to them when they are having a hard day. Some phrases that often set off an individual with diabetes are:
“Well at least you are not dying from cancer”,
“You can’t be feeling that sick. You are just being lazy”,
“Just stop eating that candy”,
“Told you not to eat that. It’s your own fault”,
“I can eat whatever I want. I’m not the one suffering from diabetes”,
“Stop whining. I’m tired of hearing you complaining about your problems”.
For the individuals with diabetes, the world can be a very lonely place. They are often being labelled as needy, hypochondriacs, and drama queens in the society whenever they voice their needs or their health problems. You do not need to offer any advice. Just lend them your ears will often be enough. By establishing the trust between you two, they will be much less likely to perceive you as part of the threat when they are going through blood glucose mood swings. They are also much more willing to listen and follow your suggestion.
If you truly wish to help, instead of offering direct suggestions such as “why don’t you eat more vegetables?” or “why don’t you start walking 3 miles a day to jumpstart the exercise routine?”, offer a more open-ended question like “Can I help you with some housework?” or “Is there anything I can help to make it easier?” These questions can open up communication and encourage them to speak about their needs.
How to Spot If Your Love One Is Suffering from Clinical Depression?
Being depressed can truly make everything in life seems less bearable. For people with diabetes, it can actually cause a lot of other health complications and make the disease even harder to beat. At the same time, it makes the anger cycle much tougher to break.
I have type 2 diabetes and got really depressed about things that were going on in my life and often felt like ending.
I am feeling very depressed today. No motivation to do anything yet so much to do. I am sick and tired of boring house jobs yet still can't get stuck into my hobbies. As for food.... I hate thinking about cooking a meal and even when I do eat I am giving up half way through.
If you sense that your love one is becoming depressed, you may want to voice your concern so that they can receive proper medical treatment and guidance as soon as possible. Here is a list of symptoms of depression:
- Feeling sad or empty almost every day
- Dramatic decrease interest in their hobbies
- Significant weight loss or weight gain
- Significant increase or decrease in appetite
- Difficulty falling asleep or sleeping too much
- Feeling sluggish and tired nearly every day
- Feeling worthless and engaging in self-blame nearly every day
- Moody, agitated, and tearfulness nearly every day
- Trouble concentrating or making decisions nearly every day
- Thoughts of dying, suicide, or plans to commit suicide
If the individual exhibits 5 or more of these symptoms for at least 2 weeks, your love one should seek help as soon as possible. Medical research have shown that professional counseling is a highly effective treatment for diabetic individuals who suffer from clinical depression. Although diabetes is often labeled as a physical disease, it is also a psycho-social problem that can benefit with routine therapies and group support sessions.
How to Handle the Aggression Situation
When you are dealing with someone who is going through a hypoglycemic or hyperglycemic attack, you must understand that they are in an altered state of mind at the time. Researches studies that found that patients act according to their perception of the “threat” present. If they feel threatened in their current situation, they are more likely to lash out at you and people in the surrounding. To avoid the onset of the “fight” mechanism and push them into the hostile state, here are some tips that may guide you to safely help them to treatment:
- Access the situation. Is the individual being aggressive and delusional? If they are in such a state, and you feel uncomfortable in handling the situation, call for emergency paramedic help. Let the paramedics know ahead of time that the individual is suffering from diabetes, appears to be aggressive, and need immediate medical attention. This will allow the control center to plan for proper assistance. In some cases, they may also send for police back up should the paramedics be unable to restrain the patient. If you are concerned what the police may do, here is usually what happens if police have to step in as the last resort:
- They will arrest the patient just so they can put a handcuff or restraining strap on the individual and prevent them from resisting help.
- They will then allow the paramedics to administer medical treatment necessary for the patient.
- Once the individual recovers from the treatment and the paramedics confirm that the patient is no longer combative, the police will remove the restraining device and “de-arrest” the person.
- There will not be any police report of this incidence.
- Even though the situation is life-threatening, use a calm tone when communicating with the individual.
- Avoid using blame or shame comments that may further agitate the individual.
- Do not crowd the individual.
- Do not touch the individual until you have their permission.
- Make sure you know how to properly treat the individual of their condition. It can become even more disaster for the patient to swing from very high blood glucose level to very low blood glucose level or vice versa as the extreme fluctuation will bring about a temporary swelling of the brain and may cause the individual to become even more delusional or succumb to coma.
Tips to Avoid Slipping into the Unwanted State
If you know that you have a tendency to hypoglycemia or hyperglycemia, and that you are likely to experience hallucination and become combative, you should talk with your physician and medical team how you avoid and deal with these situations.
- Do not wait. Out of politeness and convenience sake, you may not speak up when you know that hypoglycemia or hyperglycemia is kicking in. Only you can speak for your own needs, and your medical needs should be your only priority at the moment.
- If your child suffers from these tendencies, be sure to let the school and the teachers know of the conditions and how important it is to treat the symptoms before the condition further deteriorates. At the same time, educate them of what to do when your child becomes delusional and/or aggressive.
- Always have your medication and glucose tablets on hand to treat your symptoms.
- Wear your medic-alert bracelet at all times. In case you are going through a delusional, aggressive state, the medical team can detect your problem much faster.
- Join a support group whether it is a community group or an online forum. It is by sharing your experience with others that you can work out the psychological stress and break the anger circle. You will be amazed by the number of management tips you can learn from others who suffer from similar problems. Many individuals have noticed sharing their stories and laughing about it can be the best solution to breaking the anger cycle.
- Keep an anger diary and record any activities, discussion topics, certain foods, and specific thoughts that make you agitated. As mentioned earlier, certain rejections can trigger an onset of hostility reaction. If you know what pushes your buttons, you can find ways to deal with the issues. To take this one step further, share your diary with your medical team and your love ones. You may feel embarrassed at first about sharing these information, but it is important for your family members to understand what you are going through. And by discussing about these issues, all parties can learn more about each other. Not only will this exercise help you to be less stressed out and work out your “demons”, you will also help your family members to learn how to help you and feel less helpless in the situation.
- Learn breathing techniques to change your perspective. As mentioned earlier, your perception of the threat is an important trigger to your outburst. Instead of letting your emotions and thinking unhinge, develop a series of step to calm yourself down once you detect an early warning sign.
Here is an example guideline:
- Take a deep breath.
- Slow down your breathing and focus on the inhaling and exhaling.
- Try to sit down in a quiet place away from stimulating triggers (loud noises, bright lights, lots of people talking).
- Lean back and straighten your spine. Continue breathing slowly.
- Remind yourself to focus on treating your blood glucose level.
- Get a drink of water and focus on the sipping motion.
- Continue to sit and remain silence after the treatment until you feel like yourself again.
- Channel the anger to work for you. Make a list of how anger is holding you back from properly treating the disease. If you hate how diabetes has robbed you of enjoying life, use that energy to beat back diabetes. If you hate how the society typecast individuals with diabetes, join the American Diabetes Association to fight the prejudice or blog about all the misconceptions. The ways you can fight back against diabetes is limitless.
Further reading:
Conclusion
We hope that this article may have answered many of your concern with diabetes aggressive behaviors. If you have any personal stories and/or tips to share, please leave us a comment. We and other readers will be delighted to hear from you. By standing together, we are one step closer to beat diabetes. Don't let stereotypes cloud your judgement on diabetics.
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on June 02, 2020
References
- Adelson, Rachel. Hormones, stress and aggression – a vicious cycle. 2004; 35(10): 18.
- Bushman, B. J., DeWall, C. N., Pond, R. S., & Hanus, M. D. (2014) Low glucose relates to greater aggression in married couples. PNAS.
- Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012;42(5):484–491.
- Chung, Chen-Chih, et. al. Inflammation-associated declines in cerebral vasoreactivity and cogntion in type 2 diabetes. Neurology. 2015; 85(5): 450-458.
- Li L, Hölscher C. Common pathological processes in Alzheimer disease and type 2 diabetes: a review. Brain Res Rev. 2007;56(2):384–402.
- Mahan LK, Escott-Stump S (2000). Krause’s Food, Nutrition & Diet Therapy. 10th Ed., WB Saunders Co. Philadelphia; Reuters (2010)
- McCrimmon RJ, Ryan CM, Frier BM. Diabetes and cognitive dysfunction. Lancet. 2012;379(9833):2291–2299.
- McNay, Ewan. “Recurrent Hypoglycemia Increases Anxiety and Amygdala Norepinephrine Release During Subsequent Hypoglycemia.” Frontiers in Endocrinology 6 (2015): 175. PMC. Web. 10 Feb. 2017.
- Pfundmair, Michaela, et. al. (2015) Sugar or spice: Using I3 metatheory to understaned how and why glucose reduces rejection-related aggression. Aggressive Behavior (41)6: 537-543.
- Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. Jan 2006;27(1):24-31.
- Raison CL, Miller AH. Malaise, melancholia and madness: the evolutionary legacy of an inflammatory bias. Brain Behav Immun. Jul 2013;31:1-8.
- Romero-Canyas, Rainer, et. al. (2010). Rejection Sensitivity and the Rejection-Hostility Link in Romantic Relationships. Personality (78)1: 119-148.
- Stewart R, Liolitsa D. Type 2 diabetes mellitus, cognitive impairment and dementia. Diabet Med. 1999;16(2):93–112.
- Strachan MW, Deary IJ, Ewing FM, Frier BM.. Recovery of cognitive function and mood after severe hypoglycemia in adults with insulin-treated diabetes. Diabetes Care (2000) 23:305–12.10.2337/diacare.23.3.305
- Tabibnia, Golnaz, et. al. Common prefrontal regions activate during self-control of craving, emotion, and motor impulses in smokers. Clinical Psychological Science. 2014; 2(5): 611-619.