Here are the three questions we asked:
1. What diabetes diet mistakes do you see newly diagnosed people with diabetes make?
2. What tip(s) would you give someone who wants to stick to their diet and keep their blood sugar under control, however at same time be able to enjoy their time during the weekend or an outing with friends/family??
3. Share one of your favorite diabetes friendly recipe and tell us why its your favorite for people with diabetes.
And here are the answers we got.
Disclaimer: We at TheDiabetesCouncil recognize that both Type 1 diabetes and Type 2 diabetes are different in many ways, including treatment options as well as the diet choices and food options used. Please know that this article was established in the best interests at helping everyone who has to live with “All types” of diabetes. While some of the answers listed below may not work well for type 1 or type 2, please just use this as an educational and information source to help navigate you in choosing various food options and diet options that work well for you. Our team is dedicated to helping provide the best possible information concerning all types of diabetes on the internet. We work diligently to ensure all information provided is up to date and informative. We definitely appreciate comments, concerns and questions from YOU, our audience because you are the reason that we do what we do. Living with diabetes of any type is challenging and you are true heroes.
1. Kris Gunnars

A1: Not realizing that even healthy carbs can raise blood sugar levels. High-carb foods that are healthy for non-diabetics may not be healthy for someone with diabetes. This includes foods like whole grains.
A2: It's best to eat your protein, fat and veggies first, but keep high-carb foods to a minimum. Make sure to track your blood sugar levels to see how different foods affect you.
A3: A stir-fry with eggs and veggies, fried in coconut oil or extra-virgin olive oil.
2. Sharon Palmer

A1: They may be confused about what foods they can eat, and may be fearful about eating some foods which are actually healthy for them in balance, such as carbohydrates and fruits. They may be tempted to follow fad diets, and may overlook the importance of weight loss and exercise.
A2: I think it’s important to find a lifestyle that works for you. You can enjoy delicious, healthful foods and not feel deprived. It’s a matter of balancing your diet with lots of whole foods. I think one of the most important things one can do is to shift their style of eating and cooking to be based on more whole plant foods: whole grains, legumes, vegetables, fruits, nuts, seeds, healthy fats (such as EVOO), and less amounts of highly processed foods, such as baked goods made with refined flour, foods and beverages with refined sugars, and refined snack and dessert foods. Once you start eating and cooking this way, then you can really enjoy the flavors of foods in their natural form. So, for example, a delicious menu might be a vegetarian chili served with fresh coleslaw, whole grain cornbread, and an apple crumble for dessert. That is a meal plan based on whole plant foods—rich in fiber and health protective compounds—that will satisfy you and help you control your diabetes as well as lower your risk of heart problems.
A3: This recipe for Tortilla Soup from my book Plant-Powered for Life is completely plant-based. It’s filled with beans, vegetables, tomatoes, spices, and herbs. It’s a great, hearty one-dish meal; just serve it with a salad. This combination of fibers in the beans and vegetables will help slow the absorption of glucose in your bloodstream, and make you feel full for longer.
3. Nicole Osinga

A1: I think there's a notion that people who are newly diagnosed with diabetes think they have to completely cut out carbohydrates. While carbohydrates have an impact on blood sugar, it is the timing, amount and quality of carbohydrates that matter the most. You don't need to completely eliminate carbs!
A2: I would say either 1) Don't be afraid to 'customize' meals at restaurants and 2) always be the one bringing the healthy food to the potluck. For the first tip, I tell clients to keep ¼ their plate to starchy veggies/grains/starches, ¼ protein and ½ greens. Don't be afraid to ask for substitutions at restaurants to fit this model of healthy eating - i.e. sub out the rice for a side of extra steamed veggies or salad if you're already getting a starchy veggie with your meal. Also at potlucks, be the one bringing the greens! Fill half your plate with them and there is usually some starch and protein to make up the other half of the plate.
A3: I love the salmon, quinoa and broccoli recipe - the perfect balance of everything! Tasty and easy to make too.
4. Anna Cortesi

A1: One of the biggest mistakes newly diagnosed diabetics make is skipping meals and snacks. They do not realize the importance of eating regularly so that their blood sugar levels do not drop too low. I always advise clients not to leave their stomach empty for more than 3 hours throughout the day.
A2: I would advise them to always eat a small snack with low glycaemic index before going out.
A small wholegrain toast with cottage cheese, a low fat yogurt with some fruit or a warm vegetable soup can help slow down their hunger, thus help them not to over-eat when food is around. This way they can always keep their blood sugar levels under control and avoid dangerous ups and downs.
A3: One of my favorite diabetes friendly recipes is my rainbow chickpea salad with lemon and dill. It is an amazing, refreshing recipe, packed with protein, healthy fats, vitamins and fibre that can fill anyone up within minutes, and of course help stabilize blood sugar levels.
Rainbow Chickpea Salad (for two)
½ cup thinly sliced green onions
1 cup shredded carrots
½ cup diced celery
2 cups cooked chickpeas
1 cup halved cherry tomatoes
1 cup shredded cucumber
½ cup fresh dill
1 avocado chopped in cubes
Pinch of ground black pepper
¼ tsp Salt
½ cup fresh lemon juice
2 tbsp extra virgin olive oil
5. Maeve Hanan

A1: I often see people with newly diagnosed diabetes unnecessarily cutting out starchy carbohydrates or fruit from their diet based on the fear that these foods might affect their blood sugar level. Although both of these are broken down into simple sugars, this is needed to fuel the body and starchy carbs and fruit also provide many other nutrients which are needed in moderate amounts for a healthy balanced diet.
A2: I would recommend ‘preparing to succeed’ by planning balanced meals for the week, having healthy snacks on hand and not keeping too many tempting treats in the house. But it is also important to enjoy treats in moderation without feeling guilty for this, remembering that for blood sugar control it’s best to have sweet treats after a meal as this slows the absorption of sugar into the blood.
For those with type 1 diabetes who aren’t currently using an insulin pump, I would also recommend considering this as an option due the accuracy and flexibility this allows; so that your diabetes can work around you rather than the other way around.
A3: I’m a big fan of quick and easy healthy meals such as this vegetable stir-fry which is also a well balanced meal and is high in fiber which is useful for stabilizing blood sugar levels.
Here is a great recipe that serves 2.
Stir-fry 1 onion with 1-2 crushed garlic cloves, then add any fresh or frozen vegetables you have in the kitchen (for example: carrots, peppers, spinach, broccoli, green beans), throw in 50g of unsalted cashew nuts, a splash of low salt soy sauce, a dash of chili powder to taste and serve with wholegrain noodles.
6. Ashley Koff RD

A1: They think they need to avoid all "sugar" and confuse that with avoiding or trying to avoid all carbohydrates and/or eating artificial sugar replacements.
A2: Better nutrition comes from making better not perfect choices more often - what that means for better blood sugar is paying attention to better nutrient balance (Carbs, protein, fats & non-starchy vegetables) as well as making better quality choices, consuming better quantities with better frequency. I teach them that your family will benefit from eating the way that you do too - better blood sugar is a better health win for us all - diabetic or not. So it really comes down to those better not perfect choices - if you want fries then you don't have the bun of a burger and you don't add ketchup and sweet sauces, you could have a burger in lettuce wrap with mustard and you could dip your fries in some mustard or mayo or have them plain (if they don't taste good plain then they aren't worthy anyway). If you want a beer or wine then have 1 but you need to skip dessert even a few bites and so on.
A3: Better Avocado Toast (Socca) - especially great for diabetics because better nutrition better be delicious - and this is! You get fiber, plant protein, and plant essential fatty acids from the beans and the hemp hearts.
When breakfast turns into brunch (as in, where did the morning go?!), I shift from pancakes to savory garlic/red pepper avocado Socca. You can still top this with a pasture-raised organic egg but you don’t need to as garbanzo (chickpea) flour as well as the hemp heart toppers I added into the batter pack plant protein power as well as fiber and essential fatty acids.
Serving size:1
Ingredients for Socca:
¼ cup garbanzo flour (or puréed dried garbanzo beans)
1 ½ Tbsp warm water
1 ½ Tbsp olive oil
2 Tbsp Manitoba Harvest Hemp Heart toppers (garlic onion)
¼ rip avocado
1 pinch salt
½ tsp red pepper flakes
1 Tbsp cooking oil
Directions:
Combine all Socca ingredients in a mixing bowl with a fork. Use cast iron pan, add oil and bring to medium heat. Spoon in batter. Wait until golden brown edges, flip, press to flatten a bit and remove when both sides appear golden brown.
Place on your plate and top with mashed avocado then sprinkle red pepper flakes and salt. Enjoy better nutrition!
7. Joel Fuhrman

A1: They don’t realize that it is not sufficient to avoid high glycemic carbohydrates and sweet foods; but also oil, which is fattening and can derail weight loss success at weight loss. Most fats should come from nuts and seeds in recipes and dressings, instead of oil. They also often try to reduce calories without enough attention towards consuming nutrient-rich foods, such as green vegetables.
A2: Bring their own food to outings and get-togethers so they are not tempted to eat junk food and commercial baked goods. They should plan what they should eat in advance and not leave it to chance or emotions.
A3: Black bean brownies are my favorite, because they remind everybody to add beans to everything, since they have the most resistant starch and fiber of all carbohydrate rich foods and their regular consumption lowers the glycemic effects of other foods too. Eat bean soups, bean chilies, bean burgers and bean dips and even bean deserts.
Black Bean Brownies (serves 12)
Ingredients:
2 cups black beans, drained
2 tablespoons raw almond butter
1 teaspoon ground vanilla bean or extract
5 pitted Medool dates
½ cup natural non-alkalized cocoa powder
1 teaspoon ground chia seeds
(from The Eat To Live Cookbook)
Directions:
Blend until smooth and bake at 200 degrees for 1.5 hours
8. Amy Goldsmith

A1: The biggest mistake I see is that people get diagnosed and get very little information about nutrition and exercise from their PCP or endocrinologist. They think they need to avoid 100% carbohydrates and run the risk of hypoglycemic events. They get very overwhelmed with doctor appointments so they try to find information on the internet. There's too much misinformation on there. Every newly diagnosed patient should see a dietitian and most insurances cover it.
A2: Success with diabetes is understanding how your body uses its macronutrients, how much you need, and being aware of how you react to certain foods. Once this is understood it's all about planning. It is absolutely okay to go on an outing with friends/family. Most, once educated, will be able to come up with an appropriate meal, pack snacks, or make suggestions of where they can go that best fits their nutrition plan.
A3: Oven Pork Stew with Sweet Potatoes and Shallots.
This is a great recipe from the American Diabetes Association. Easy to make and tasty.
9. Maye Musk

A1: They don't seem to understand how serious it is to follow a healthy diet. They have to plan ahead to eat well. Complications from diabetes and side effects from the drugs need to be avoided.
A2: You can have fun with friends, but if you need to lose weight, eat half portions and take the other half home, or eat later as a snack. You are at risk for diabetes, you can't let things go. It's not fair, but that's how it is. I'm 68, and on diet all the time. My other option is to overeat, gain weight, and increase my risk for nutrition-related diseases.
A3: I always recommend bean soup. Buy a variety of beans, soak them overnight, boil them, and then add plenty of vegetables. Have one cup before a meal or as a snack. This will be 1 Carb serving. It's high in essential nutrients, including fiber, filling and delicious.
10. Jessi Haggerty

A1: Since people with diabetes often hear that the condition affects their blood sugar levels, they automatically think they should eliminate all sugars and/or carbohydrates. But the truth is, if you have diabetes or not, your body needs carbohydrates for energy. So don't go eliminating sugar just yet! Make sure to work with a dietitian to help you control blood sugar levels through a balanced diet where all foods can fit!
A2: Like I said above, all foods can fit, and sugar is certainly not the enemy. Pairing carbohydrates (like sweets, pasta, bread, etc) with a food that also contains fat and protein (meat, eggs, cheese, nuts and seeds all fall into these categories) can help regulate blood sugar levels and prevent too high of a spike. So whether you are enjoying a dinner at home or a holiday party, you can easily find a way to add some high fat and protein foods to your meal.
A3: Orange Sesame Chicken! This is one of my favorite Chinese food dishes, but most take-out places use sauces that are very high in sugar. And while sugar doesn't need to be avoided, I like to have my chicken with a side of rice (a carbohydrate). So, I make a healthier sauce (with just as much flavor) and serve it over broccoli and rice.
11. Lori Zanini

A1: Individuals newly diagnosed with diabetes often look at only the grams of sugar on a food label, instead of total carbohydrates as well. Currently, the sugars are calculated into the total carbohydrates, so it's important to take note of both. If a product has 0 grams of sugar (which is great) it still doesn't necessarily mean that it will not raise blood sugar levels. Generally, it is recommended women consume 30-45 grams of total carbohydrates per meal while men consume 45-60 grams of total carbohydrate per meal. Always follow up with your personal dietitian/diabetes educator to customize your specific dietary needs.
A2: First of all, it's important to note that eating to control blood sugar levels is simply a healthy diet and anyone can benefit from eating this way, not just those with diabetes. Focus on what you are drinking, make sure you consume plenty of water and stay hydrated. Additionally, ensure you are eating a lean protein at every meal and snack since protein not only helps keep us satisfied, but also helps stabilize blood sugars. And also just as important, enjoy your time with your family and friends and enjoy the food you eat while being mindful of the portions.
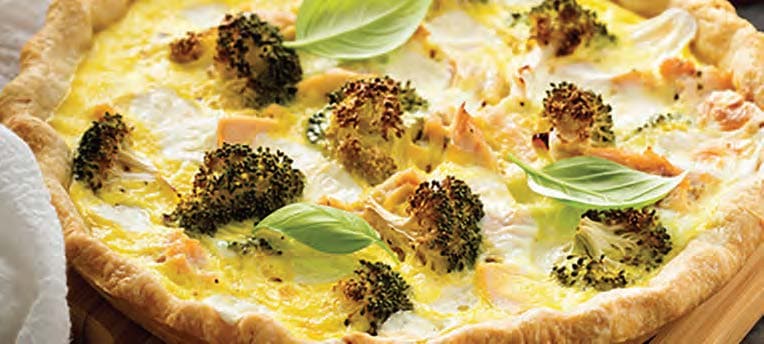
A3: I have a very popular Broccoli Basil Quiche Recipe in my free 7 day diabetes meal plan. It's one of my personal favorites because it's a great high protein way to start your day and I love it because it's a healthy version of a food that many people think is 'off limits' when you are trying to improve your blood sugar. It also teaches individuals how to use common ingredients to make more diabetes-friendly dishes.
Broccoli and Basil Quiche
Serves 8 / Prep Time: 20 minutes / Cook Time: 55 minutes
Dubbed an anticancer vegetable due to a special enzyme named sulforaphane, broccoli is at its best in early summer and then again in fall. This nutrient-packed brassica shines in this simple morning quiche that shows off its finer sides. To speed things up on a busy morning, assemble the quiche the night before and cook it in the morning, or if preferred, you can even cook it over the weekend and heat it up for breakfast in the oven or microwave.
For the almond flour crust:
1 cup almond flour
¼ teaspoon salt
½ teaspoon baking soda
3 tablespoons extra virgin olive oil
For the quiche:
1 cup finely diced broccoli
4 scallions, diced
½ cup sundries tomatoes, diced
¼ cup roughly chopped basil leaves
4 eggs, lightly beaten
1 cup plain, unsweetened almond milk
⅛ teaspoon salt
¼ teaspoon freshly ground black pepper
⅛ teaspoon garlic powder
To make the almond flour crust:
1. Preheat the oven to 350°F.
2. In a large bowl, combine the almond flour, salt, and baking soda. Toss to combine.
3. Pour in the olive oil in a stream, stirring as you pour. Continue stirring until the dough comes together. Add 1 to 2 tablespoons of water, as needed, to hold the dough together.
4. Transfer the dough to a 9-inch pie dish. Press the dough into the pan’s bottom.
5. Bake for 15 minutes, until the dough is golden brown. Remove from the oven and let cool completely while you make the filling
To make the quiche:
1. In a mixing bowl, toss the broccoli, scallions, tomatoes, basil and flour. Add the eggs and milk. Season with salt, pepper and garlic powder. Pour into the prepared baking shell.
2. Cook for 35 to 40 minutes, until the center is set. Remove from the oven and let rest for 5 minutes before cutting.
Prep Tip: Frozen broccoli can be used in this recipe as well. Remove the broccoli from the freezer and let rest at room temperature for 10 minutes before carefully chopping the broccoli. Use as directed above.
Nutrition Info (1 piece):
Calories: 177; Total Fat: 15g; Saturated Fat: 2g; Cholesterol: 82mg; Sodium: 317mg; Carbs: 7g; Fiber: 3g; Sugar: 2g; Protein: 7g
12. Mindy Black

A1: The common mistake I hear from most newly diagnosed DM patients is that they cut out ALL carbs. This statement is immediately followed by how deprived they feel and how they do not think they can reach acceptable blood sugars. I love to be able to show them you can still include carbohydrates in your life! You must learn balance and portions, but it is not an all or nothing disease.
A2: PLAN ahead. Be in control of your circumstances. If you know you are going to a restaurant with people, do your research. Call ahead, talk to a manager, and look online. Do whatever it takes to find what you can safely order. Realize you are in control of your order, and you can modify anything on the menu. If having a cookout or potluck, bring something you know fits your needs; possibly eat a snack beforehand to control timing of medications and hunger.
A3: I love using spaghetti squash as a pasta alternative. Missing spaghetti? Try this:
Serves 2
Ingredients: 2 spaghetti squash halved, 1 jar marinara sauce, 8 oz. ground turkey breast, 2 handfuls cherry tomatoes- halved, 3 zucchini- chopped, salt & pepper to taste.
Directions: Wrap spaghetti squash in saran wrap and place flat side down in microwave. Microwave for ~10 minutes until soft. While microwaving, brown turkey breast- set aside. Sauté zucchini and cherry tomatoes in 1 tbsp. olive oil. Add marinara sauce and turkey breast to mixture. Heat on low until squash is ready. Scoop seeds, and use a fork to pull "spaghetti". Toss with marinara mixture, & serve. You can add shredded Parmesan to the top if desired. Total time: ~15 minutes
13. Ashley Acornley

A1: The biggest issue I see when counseling a newly diagnosed patient with diabetes is that they assume (or have been told by their primary care doctor or a friend/family member) that they are no longer allowed to eat carbohydrates. I also hear often that patients can no longer eat any “white foods.” While many “white foods” can include refined grains and sugars and should be limited, it is not true that all carbohydrates and white foods should be eliminated. Carbohydrates are essential for energy and without them, our body wouldn’t function properly and our blood sugar would bottom out. The key is to find an appropriate balance of healthy carbohydrates in the diet, and to balance that with plenty of protein, fruits and non-starchy vegetables.
A2: I typically provide my newly diagnosed patients with a calorie level that is healthy for them to reach their goals, and carbohydrate levels to stick to per meal and snack. I teach them basic carbohydrate counting, and provide them with a sample meal plan to review portion sizes, food pairing, and timing of eating. All of these things combined comprise a healthy lifestyle. So, if someone is going out with friends/family, I would advise them to look over the menu ahead of time, monitor their portions, and estimate their carb intake to make sure they are still close to their goals.
A3: I love the blog Skinnytaste; it has a low carb section where I can find some interesting recipes. I love using cauliflower as a carbohydrate substitute. It provides more fiber, veggies, and vitamins in your day, and can blend well together to make rice, crusts, and breads. On their blog you can find recipe for “cauliflower rice.”
14. Nichola Whitehead

A1: Cutting out sources of refined sugar (sweets, biscuits and cake etc) but forgetting about refined carbs such as white rice, white pasta and white bread which also break down into glucose. All carbohydrates break down in to glucose and so portion size is key for both sugary and starchy sources.
A2: My philosophy is the 80/20 rule; i.e. make sure to eat healthily for at least 80% of the time. If you know that you have a weekend event coming up then make sure that the week leading up to eat is a healthy one packed with whole foods and perhaps go for a walk after you go out to burn off any excess glucose!
A3: I love this recipe Crushed Ryvita Salmon as it is low carb as well as being packed with heart healthy omega 3 fatty acids.
15. Pamela Fergusson

A1: The number one mistake people make is not getting enough fiber. People often try to avoid fruits and vegetables, thinking that there is too much sugar, but the reality is that they need the nutrients from fruit and vegetables for a healthy diet. Instead, it is useful to cut back on highly processed foods, especially those with added sugar. Increasing the fiber in your diet through health portions of vegetables, fruits, nuts, seeds and whole grains is an important part of blood sugar regulation and achieving and maintaining a healthy weight.
A2: The key to being able to enjoy outings is a little planning. Take the time to research which restaurant to visit. Look for one that doesn't just tell you the calorie count and grams of carbohydrates on the menu, but focuses on whole foods. This may mean that everyone tries out a new place. Focus, not just on how the food tastes, but how does it makes you feel afterward. Start a new tradition of being active with friends and family. After dinner, go for a walk or go skating or bowling.
A3: This lentil stew is easy and a delicious way to get your fiber.
Ingredients:
1 cup dry lentils
3 ½ cups vegetable broth
1 (14 ½ ounce) cans of peeled Italian tomatoes ( cut up)
1 cup peeled chopped potato
½ cup chopped carrot
½ cup chopped onion
1 tablespoon dried parsley
1 tablespoon dried basil ( crushed)
1 garlic clove ( minced)
1 dash pepper
Directions:
1. Rinse and drain the dry lentils.
2. In a saucepan combine the lentils, vegetable broth, tomatoes, potatoes, carrots, parsley, basil, garlic, and pepper.
3. Simmer for 45-50 minutes until lentils and vegetables are tender, stirring occasionally.
Based on: http://www.food.com/recipe/easy-lentil-stew-191459
16. Cheryl Mussatto

A1: The mistake I see that most of those newly diagnosed with diabetes make is not getting into a regular, consistent routine of balancing their diet and exercise with their work and play. It is very important to not skip meals, try to eat around the same time each day with about the same amount of carbohydrates at each meal and to make exercise their best friend. If they practice this, they are well on their way to achieving better blood sugar control.
A2: The key here is to plan ahead. Stick mainly with healthy carbohydrates of non-starchy vegetables, fruits, and whole grains. Keep portion sizes small of any desserts or sweets and never consume alcohol on an empty stomach. It would also be advisable to get in some extra exercise both before the event and again the next day afterwards to help use up excess glucose from most likely starchier foods that were eaten.
A3: Here is also a link for a favorite diabetes recipe of mine - http://www.bettycrocker.com/recipes/cheesy-chicken-skillet-dinner/71734c1a-d6ac-4b4b-b9c2-4b22eb6967de
17. Angela Lemond

A1: I would say the biggest mistake is not getting a referral to a registered dietitian nutritionist (RDN) that specializes in diabetes self-management. They would go through very practical ways to manage diabetes including the start of a targeted constant carbohydrate nutrition plan. People often think they need to stop eating carbohydrates, but that is absolutely not the case.
A2: A constant carbohydrate plan gives a person a "budget" of carbohydrates at meals and snacks. When a person goes out, the choices may not be as healthy but they can still be in proper doses to not exacerbate glucose levels.
A3: I think my shrimp stir fry on the grill is great for those with diabetes. It is very nutrient-rich with a lean protein and it includes a whole grain (brown rice) -- the dish is balanced and high in fiber. A fresh and easy dish that is very flavorful.
18. Sarah B. Krieger

A1: For type 1: they are told there is a honeymoon phase—usually, approximately a year (true), so eat what you want—just aim to eat at the same times and check your blood glucose.
For type 2: try to eat the same time each day (doesn’t matter what) and take your medication at the same time each day
A2: Plan ahead! If you know you are going to a restaurant or eating a meal you do not plan, eat your best around those meals. Choose vegetable-centric meals as best as possible with lean protein (chicken breast, beans, lean beef or pork) and a handful of carbs at restaurants. Look at their online menu or app before heading out so you know what to expect.
A3: Everyone has favorite meals, but a Caprese salad satisfies many palates. Kids, adults and anyone aiming to get more fruit/vegetables in a meal with flavor enjoy this. Layer fresh tomato slices with fresh basil leaves and mozzarella slices. Drizzle with a dark balsamic vinegar and a slighter less drizzle of olive oil. Sprinkle with the best sea salt and fresh black pepper.
19. Gillian Mconnell

A1: Cutting out carbs completely because they think they will raise blood glucose levels. When in actual fact, carbs at each meal, especially complex carbohydrates like wholegrain pasta and bread are released more slowly and help keep glucose levels more steady, instead of experiencing potential peaks and troughs in levels when carbs are avoided.
A2: Tips - always eat regular meals, never skip meals which can lead to not only dips in blood glucose levels, but also leads to overeating at the next meal or cravings for sugary foods later that day. Watch your portions, I can't emphasize this enough. It's often not the food itself that raises blood glucose levels, but the quantities the food is eaten in. Eating several pieces of bread in one go or too much fruit in one go or too much of any food in one go will contribute to a sharp rise in blood glucose levels. Spread fruit throughout the day always and focus on having more veg than fruit in the diet, so stick to 2 - 3 portion of fruit per day and 4 - 5 portions of veg per day.
A3: Salmon with bulgur wheat and mixed peppers and a balsamic vinaigrette dressing - why because I love the vibrant colors and all the flavors go lovely together. It makes for pleasurable eating! It's high in fiber and antioxidants and the fish provides a weekly dose omega-3 fatty acids!
20. Amanda Li

A1: Hands-down the number one diet mistake or misinformation among newly diagnosed people with diabetes is the notion that all CARBS are BAD and that they should avoid them like the plague! I've seen so many people come in and afraid to eat in fear that their blood sugar levels will be too high after a meal. It is definitely important to explain to people the importance of carbohydrates and how to plan meals accordingly, via portion control, strategic carbohydrate selection, and macronutrient balancing. Another common diet mistake I encounter frequently is not understanding how to read food labels correctly. For example, focusing on the grams of sugars only, versus looking at the total carbohydrate and fibre content of a food.
A2: During meals, load up on the vegetables. If you're eating out, you can always ask for an extra side of steamed veggies or salad to go along with your entree or even swap out your side for the vegetables. If it's a potluck or dinner party, offer to bring a vegetable dish to the event which ensures that you have at least one option to fill half your plate with. My rule of thumb always is that for each mouthful of starchy carbohydrate you eat (i.e. potatoes, rice, bread, quinoa, pasta); you eat 2 mouthfuls of non-starchy vegetables (i.e. green beans, broccoli, cauliflower, lettuce, asparagus, etc.). This ensures that you eat a high-fiber meal which will keep you feeling satiated and help manage your blood sugars.
My second tip would be to sign up for the clean-up team 🙂 Of course that is if it is a dinner party. If you are eating out, then instead, get up off your chair and start working the room, mingling and chatting with other guests. The key here is to get moving rather than sitting, as exercise will stimulate your body to uptake glucose more readily after a meal.
Lastly, if you are going to order an alcoholic beverage, stick to straight-hard alcohols such as vodka, gin, whisky or tequila, and you can mix it with a non-caloric beverage including club soda, diet coke to increase the volume of the beverage. Limit to 1 drink if possible though! Moderation is key 🙂
A3: Before I share my favorite "diabetes friendly" recipe I have to admit that I really do not like that term at all... The reason being is that all foods and recipes can be "diabetes friendly" so long as you know how to control and balance your portions appropriately. With that being said, I do have a recent recipe that a lot of my clients absolutely love, since it swaps out potatoes for a lower-carbohydrate containing vegetable, which means they can enjoy more of it 🙂 This recent creation is: Pan-Seared Arctic Char with Brussel Sprouts and Whipped Cauliflower Mash. It sounds fancy but boy is it easy to make! I absolutely love teaching people how to prepare fish because it's such a simple protein of choice to prepare once you learn the cooking fundamentals. Not to mention, the flesh of fish cooks really fast, unlike proteins such as chicken or pork, so a meal can be prepared in matters of minutes. Here's a quick video tutorial on how to prepare the entree in less than 15 minutes:
21. Jill Weisenberger

A1: It sounds logical to decrease sugar intake if you hear that you have high blood sugar. So many people focus on this to an extreme or focus on this without paying much attention to other aspects of diet. While it sounds logical to put your energies in cutting sugar, diabetes is really more complicated than that. Diabetes is defined by high blood sugar, but type 2 diabetes is really a problem of insulin resistance, which is related to heart disease and some types of cancer too. Thus, diet and lifestyle strategies that reduce insulin resistance and help prevent chronic disease are paramount. If someone is focusing just on sugar, they might stop eating health-boosting fruit and drinking milk (12 grams of sugar per cup) and eat a boatload of rice or a plateful of bacon. The rice is low in sugar, but it has 90 grams of carbohydrate in 2 cups. Those 90 grams contribute to blood sugar. The bacon is low in carbs, but meals rich in saturated fat worsen insulin resistance. This same person might be fearful of beans and lentils because they are rich in carbs. But diets rich beans and lentils are associated with less heart disease and good control of blood sugar.
A few sessions with a registered dietitian nutritionist who is also a certified diabetes educator can be invaluable. This is the person to help you create your best diet, based on your labs, your food preferences, your budget, your goals, etc.
A2: A healthful diet leaves room for fun. Don’t plan a diet that is so restrictive that you can’t stick to it.
I remind people of two things: First, food doesn’t drop off the face of the earth, so you don’t have to eat it just because you see it. Wait until the time is right. For example, you don’t need to dig your hands into the popcorn and candy just because your friends are doing that. Popcorn and candy are easy to get, so you can get them another time.
Second, you are always faced with choice points. Try to recognize them and respond from a place of kindness and not a place of punishment. When your friends are digging into the wings or French fries, recognize that this is a choice point. Instead of reacting and digging in too, make a decision about eating them. You can decide to eat them or not, but recognize that it’s a choice. If you choose to eat them, then enjoy the living daylights out of them and don’t allow feelings of guilt to seep in. If you choose not to eat them, then recognize that this is about self kindness and empowerment. Use kind and empowering words, even if only in your mind. “I can't eat that” isn’t empowering. “I choose not to eat that” is empowering.
A3: Here’s a great recipe: https://jillweisenberger.com/chocolate-dipped-apricots/.
I’m a fan of desserts with benefits. The dark chocolate has disease-fighting flavonoids and the apricots have lots of health-boosting phytonutrients. 3 pieces is a mere 15 grams of carbohydrate.
22. Doug Cook

A1: While the reason for it is understandable, people with diabetes have been lured into thinking that fat is bad and low fat is best given the increased risk for CVD that is associated with diabetes due to the overall metabolic disruption with insulin and glucose metabolism. As such, many with diabetes try to go for a low fat diet but it's quality that matters; high fat foods like nuts, seeds, fatty fish, avocados, fuller fat milk are highly nutritious and satisfying which can help with satiety and slowing blood sugar swings. The gold 'trio' I mention is fat, protein and fiber. Together they work best to keep hunger in check. This combination happens without thinking about it when a variety of foods are eaten together - think the plate method for example. Low fat foods like tuna is one thing, but package/processed foods can be problematic since they can be higher in total carbohydrate and added/free sugars.
I am not a fan of the glycemic index, for me it should never have left the lab/research setting. People avoid carrots as the example that's used all the time thinking a typical serving of carrots sticks will raise blood sugar and or are too high in 'sugar' because of its GI - I'd rather talk about food versus resorting to a number that has a large amount of variance since the GI can be affected by so many factors.
A2: 1. Plan. As the saying goes, people don't plan to fail but they often fail to plan. They need to think ahead about how they will manage the situation; where they might be eating, the types of foods (if it's a pot luck), and as part of his/her education, learn how to strategize whether that's smaller serving of dessert without denying oneself, eating more low starch vegetables to off-set higher starchy foods etc. I like to make it client centered; if they have Type 2, relatively well controlled with oral meds etc it's not as critical as a Type 1 or Type 2 on insulin where blood sugar control is more sensitive to insulin dose and amount of food/alcohol eaten. Planning is the best way to balance the needs of their diabetes and the need for socializing and psychological well-being.
A3: I don't have specific ones on file but it would be Mediterranean-style based/or one that's modest in starch foods and rich in a variety of plant and animal based foods; the recipes would be rich whole foods, include fattier foods like fatty fish, nuts, seeds, avocado, avocado or olive oil, fiber rich foods like chickpeas, lentils, plant foods rich in viscous fibers like okra, eggplant, oatmeal etc.
This recipe is perfect - it has eggplant, walnuts, and lots of flavor and would make a perfect side to a protein rich food like fish, chicken, beef or pork or other meats.
23. Lindsey Pine

A1: Many newly diagnosed patients don’t make an appointment with a Registered Dietitian and think they can figure it all out on their own. Patients also often think they can’t eat any carbs, which is completely false. A Dietitian can help develop an individualized plan that works with the patient’s lifestyle. I even see people who’ve had diabetes for years and they still don’t have a plan.
A2: Plan, plan, plan! If you have a good plan in place, you’ll be able to enjoy yourself much more. Prior to the event, find out what is on the menu or what the host is serving. That small amount of research will help you decide on your food choices in advance or let you know if you need to bring some of your own food.
A3: I love appetizers and enjoy bringing dishes that are delicious and diabetic friendly such as this Shrimp Cocktail with Smoky Romesco Sauce. Using shrimp instead of crackers as a dipper makes this a low carb dish.
http://tastybalancenutrition.com/recipe/shrimp-cocktail-with-romesco-sauce/
24. Brynn McDowell

A1: I often see the following mistakes in newly diagnosed diabetes patients: Eliminating all carbohydrates from their daily meals or not spacing out their carbohydrate intake though out the day. Ensuring you are eating your recommended daily amount of carbohydrates and spacing them out equally throughout the day will help regulate blood sugar levels so you avoid those highs and lows.
A2: My tip to give someone who wants to keep his blood sugar under control but at the same time be able to enjoy time with friends on the weekend is to have a game plan. Figure out beforehand approximately what time you will be eating and how many carbohydrates you should have at each meal throughout the day. If you are at a party with food, take a look at the options and make a plan. Remember to fill up on vegetables and lean proteins and then add in your carbohydrates based on your plan. Having a game plan takes the stress out of activities and allows you to enjoy your weekend while still keeping your blood sugars under control.
A3: One of my favorite diabetes friendly recipes is this Mediterranean Power Bowl. It is so simple to make and the flavors are amazing! The quinoa offers protein and carbohydrates, paired with fresh vegetables and heart healthy fats, it's a complete meal. It's also easily transportable, making it a great work lunch or meal to have on hand when hunger strikes.
25. Shauna Lindzon

A1: With a new diagnosis comes fear of carbohydrates. I find that when people are newly diagnosed they tend to try to avoid foods that are high in any type of carbohydrate. They will focus on eating foods high in protein and not concentrate on eating complex carbohydrates. Unfortunately, they will be getting less fiber in their diet and run the risk of constipation or uneven blood sugars.
A2: I would teach them that all foods can fit. Complex carbohydrates such as foods with oats, different types of flour, and fruits can be enjoyed on a daily basis. A good tip is to have the food highest in sugar after they have eaten their meal. For instance a berry cobbler that is enjoyed as a dessert won't raise their blood sugar as quickly as if it was eaten on its own.
A3: My massaged kale, butternut squash lentil salad is a healthy and delicious recipe. It is loaded with vitamins, minerals, protein, fiber and phytonutrients. It has the extra bonus of fresh ginger which is anti-inflammatory.
Massaged Kale And Roasted Butternut Squash Lentil Salad
6 servings
Ingredients:
1 lb (about 2 cups) ½ - ¾ inch butternut squash cubes
¼ cup olive oil
½ tsp kosher salt
2 tbsp white wine vinegar
2 tsp maple syrup
1 tsp Dijon mustard
1 ½ tsp finely minced fresh ginger
1 clove garlic, finely minced
1 large bunch kale, stems removed, torn into bite-size pieces (about 8 cups)
1 ½ cups cooked brown lentils (or one 15-ounce can, rinsed and drained)
Directions:
1. Preheat oven to 425°F. Spread the squash out on a parchment lined baked sheet. Drizzle with 1 tbsp olive oil and sprinkle with ¼ tsp salt. Roast for about 25 minutes or until brown on the outside and soft on the inside. Set aside to cool.
2. Stir together the remaining olive oil, vinegar, maple syrup, mustard, ginger, garlic and
¼ tsp salt in a large bowl.
3. Add the kale to the bowl with the dressing and massage the dressing into the kale.
4. Add the cooled squash and the lentils and toss to coat.
5. Season with extra salt if desired.
26. Jennifer Koslo

A1: The biggest mistake I see in the newly diagnosed is drastically cutting back on carbohydrates regardless of their nutrient density. Many will eliminate all fruits and drastically reduce or eliminate all grains.
A2: A tip for weekend outings is to plan ahead and if possible look up menus beforehand in order to scout out healthy choices. Decide what you want to splurge on in advance, whether it is a cocktail or a breakfast buffet and be choosey. Don't aim for perfection but do aim to strike a balance. Then allow yourself those small indulgences by eating strategically and loading up on healthy foods first, such as choosing a broth based soup and salad as a starter to take the edge off of hunger before eating higher calorie foods. Sharing entrees is another way to enjoy eating out while staying on track. Finally, schedule a longer workout using the weekends to stay in calorie balance and to refresh your routine.
A3: A favorite recipe is cauliflower fried rice as it is a healthy take on a familiar favorite and is a good example of how favorite foods can be included in their diet - I like to tell clients to think in terms of what they can add to their diets instead of what they need to eliminate.
Ingredients:
5 cups roughly chopped cauliflower (about 1 medium head)
¾ cup egg whites
2 cups broccoli (fresh or frozen)
1 cup sugar snap peas
1 cup frozen peas
1 cup chopped onion
1 cup chopped red pepper
1 tsp garlic
1 Tbs sesame oil
2 Tbs teriyaki sauce
Instructions:
1. Working in batches, pulse cauliflower in a blender until reduced to small rice-like pieces.
2. Bring a large skillet or wok sprayed with nonstick spray to a medium heat. Scramble egg whites until fully cooked, 3-4 minutes. Transfer to a large bowl, and cover to keep warm.
3. Remove skillet from heat; re-spray and bring to medium-high heat. Add veggies and ¼ cup water. Cover and cook for 3 minutes. Add onion, garlic, and sesame oil. Cook and stir until veggies have softened, about 6-8 minutes.
4. Add scrambled egg whites and teriyaki sauce. Cook and stir until hot and well mixed, about 2 minutes.
Makes 5 servings.
27. Ann Louise Gittleman

A1: I see many newly diagnosed diabetics who don't realize that including more healthy fats in the diet (i.e. coconut oil, olive oil, nuts, and seeds) will help to normalize blood sugar levels without resorting to drastic measures.
A2: I would remind those newly diagnosed with diabetes that both protein and healthy fat foods can be generously enjoyed on a diabetic diet. Filling up on guacamole, natural cheeses, and toasted nut mixtures will be helpful in regulating blood sugar as will high fiber-filled seeds like chia, flax, and hemp which also keep blood sugar on an even keel. Choosing fresh or frozen fruits for dessert with a little non-sweetened whipped cream or coconut cream is also highly recommended.
A3: This snack is high in fiber and healthy "smart" fats that provide satiety and crush cravings for sugary treats.
Toasted Sesame Guacamole
Ingredients:
3 large avocados
1 leek, white portion, chopped
1 teaspoon fresh lime juice
½ teaspoon low-sodium, wheat-free tamari sauce
½ teaspoon toasted sesame oil
2 teaspoons toasted sesame seeds
2 tablespoons cilantro, chopped
Sea salt to taste
Toasted sesame seeds:
1. Heat a heavy skillet on medium heat.
2. Pour in a layer of sesame seeds.
3. Stir constantly until the seeds turn lightly golden and release their warm, nutty aroma.
4. Set aside to cool.
Guacamole:
1. Halve, pit, and scoop out the avocados into a bowl.
2. Mash with a fork until the desired consistency.
3. Stir in the leek, lime juice, tamari, sesame oil, sesame seeds, and cilantro and season with the sea salt.
Flaxseed Crackers
1 cup ground flax seeds
4 teaspoons Fat Flush Flavored Blend Chapter 10)
½ cup vegetable broth
Directions:
1. Preheat the oven to 275°F.
2. In a large bowl, mix the dry ingredients.
3. Add the broth and let sit for 1 to 2 minutes.
4. Stir the mixture with a fork until the seeds start sticking together, about 5 minutes.
5. Spoon the mixture onto a lined cookie sheet and cover with wax paper.
6. Using a rolling pin or drinking glass, roll the mixture flat and out toward the edges of the cookie sheet; remove and discard the top wax paper.
7. Score the dough lightly into 16 crackers, using a pizza cutter or fork.
8. Bake the cracker mix for 1 to 1½ hours, until the crackers lift off the cookie sheet and crack apart easily.
28. Samantha Cassetty

A1: Oftentimes people are very concerned with sugars without recognizing that the total carbohydrate content of the diet is key.
A2: I always encourage people to bring something they can eat if they’re going to a party or family gathering. More than ever, it’s easy to find delicious recipes that happen to also be nutritious. Also, remember that the gathering is about conversation, connection, community, etc. Focusing on the social aspects of the event does not depend on what you are or aren’t eating
A3: One thing I’m loving right now is my weeknight go-to: Shrimp with smoked paprika cooked in garlic oil. I’m a working single mom so weeknight dinners have to be easy! I make this without even chopping the garlic!
Saute a few whole garlic cloves in about 1 Tbsp. extra virgin olive oil over medium heat until fragrant and browned. While garlic is cooking, toss 1 pound fresh or frozen deveined shrimp in 2 tsp. smoked paprika and ¼ tsp. salt. Remove garlic cloves from skillet and turn to medium-high. Add shrimp to skillet, cooking about 2 ½ minutes on each side until opaque throughout.
I’ll serve this with a side salad and a veggie, like roasted Brussels sprouts or sautéed spinach. What makes this great is that it’s low in calories and carbohydrates, but rich in flavor. The combination of protein from the shrimp and fiber from the veggies makes it a satisfying meal. Plus, people with type 2 diabetes are at a higher risk of heart disease and the omega 3s in shrimp help benefit the heart.
29. Rebecca Bitzer

A1: Many individuals who have recently been diagnosed with diabetes are overwhelmed, and they instantly cut out anything white, or even all carbohydrate foods. However, our bodies need carbohydrate because our brain uses that glucose to function. By consuming smaller portions of carbohydrate, paired with veggies and a good source of protein, individuals with diabetes can better manage their blood sugar. Bread, potatoes, and pasta are allowed, but it is very important to be aware of portion sizes and trying to choose whole grains when possible.
A2: Eating out is possible with simple substitutions. The goal is to first start with a balanced plate. Choose baked or grilled proteins, over fried, and ask for a double helping of non-starchy vegetables. I would advise them to eat slowly, and as soon as they feel full and satisfied, ask for a box to take the rest home, rather than continuing to pick at it for the duration of the meal. If it’s a special occasion, and the group wants to get dessert, share with the table and have just a few bites to satisfy that sweet craving.
A3: I love our almond crusted chicken! The almond coating gives the chicken a crispy texture without requiring batter and a deep fryer. Even better, the almonds are a heart healthy addition. This could also be made into chicken tenders for a kid-friendly spin.
30. Loren Cordain

A1: I am not a clinical practitioner, but a nutrition researcher from Colorado State University. Frequently, type 2 diabetic patients are unaware of the glycemic index and glycemic load of foods. Breads and refined cereal grains, even some whole grains, maintain high glycemic loads which worsen blood glucose and insulin control.
A2: When dining out try to choose a high protein main dish (salmon, fish, poultry, beef, pork, seafood [crab, shrimp, lobster etc.] with a salad and steamed veggies. Avoid bread, potatoes and sweet deserts and choose fresh fruit instead. Enjoy a glass of dry wine or a cocktail, as there is substantial evidence to show that moderate alcohol consumption has no adverse effect upon glucose or insulin metabolism.
A3: The recipe below comes from my new cookbook, "Real Paleo Fast & Easy", Houghton, Mifflin Harcourt, 2015. All recipes in this book are therapeutic for type 2 diabetic patients and contain no added sugar, refined cereal grains or salt -- only fresh foods. This recipe is delicious!
Asian Ground Pork And Lettuce Wraps
Makes 4 servings
Ingredients:
1 tablespoon sesame seeds
1 tablespoon coconut oil
½ cup minced shallots
2 tablespoons minced fresh ginger
2 cloves garlic, minced
2 teaspoons salt-free Chinese five-spice powder
1 pound ground pork
1 cup finely chopped red sweet pepper
½i cup finely chopped no-salt-added water chestnuts
6 scallions, sliced
1 head Bibb lettuce, leaves separated
Wafer chestnuts give the ginger- and garlic-infused filling for the lots of crunch. Be sure to use only canned water chestnuts that have no added salt or other non-Paleo ingredients.
Direction:
1. In a dry large skillet toast the sesame seeds over medium heat about 3 minutes or until golden brown and fragrant, stirring often. Remove sesame seed to a plate; let cool.
2. In the same skillet heat the coconut oil over medium-high heat. Add shallots, ginger, and garlic. Cook and stir 4 minutes or until onions are translucent. Stir in the five-spice powder; cook about 30 seconds or until very fragrant.
3. Add pork and sweet pepper to skillet; cook until meat begins to brown. Stir in water chestnuts. Cook 8 minutes or until the pork is no longer pink. Stir in scallions.
4. Divide pork filling among lettuce leaves. Sprinkle with toasted sesame seeds.
31. Lindsay Pleskot

A1: Thinking they have to avoid carbs altogether, including fruit! Not all carbs are created equal and we need them for energy. Plus by balancing meals with protein and fat, it slows rhetoric rate that carbs will increase our blood sugars so it is more about the portion, balance and frequency of eating than just carbs alone.A2: Moderation! Keep portion size in mind. If it's half the size it will have half the impact on your blog sugars. Get rid of the all or none mentality. This is what sets people up to fail. Also, practicing mindful eating can be really helpful. When they are enjoying their favorite treats to really pay attention to the taste, texture and overall enjoyment of the food. This will lead to increased satisfaction and help with portion control. It can also help to tune in and pay attention to whether they really actually want the food or are just eating it out of habit.
A3: This Lemon Pesto Rainbow Chickpea Pasta is one of my favorites. I love sharing it as a diabetes friendly recipe because many people with diabetes assume they can no longer eat pasta. Again, it all comes down to portion and balance of the meal. Because it is packed with veggies mixed right into the dish, as well as fiber and protein rich chickpeas, it is much better for blood sugar control than typical pasta dishes. I would suggest serving this with a nice fresh salad on the side to make sure you're getting that half plate of vegetables that our blood sugars love!
32. Summer Blankenship

A1: Unfortunately patients are often given the "quick and easy" advice that don't tell the whole story and make managing diabetes seem like a quick fix. For example you'll hear patients say "I can't eat white food" or "I just can't eat sugar". But really eating well with diabetes is going to be a journey towards improving your overall diet quality (more vegetables, lean protein, portion control, exercise, water, etc) and living a healthy lifestyle that includes REAL food in reasonable amounts. I also hate to see patients think they can't have any carbs and end up on very low carbohydrate or ketogenic diets! That's just not necessary and can actually be dangerous! The key is portion control of carbohydrate foods and testing your sugar at home to know if you're in control.
A2: Unfortunately most Americans use food as their only outings with friends. I challenge my patients to find activities that don't involve food to be their fun time with friends - go hiking, walk the beach, country line dancing, art classes, or even cooking at home etc. But if you are going out to eat I encourage you to keep it all in perspective. The goal of living well with diabetes is to manage your blood sugar into a healthy range most of the time to prevent long term complications such as heart attacks or vision changes. Occasional excursions into higher than usual range for special occasions are okay. My advice would be though to really be able to say "that was worth it" and to really be picky about what actually counts as a special occasion. And then enjoy every bite and don't feel guilty! When we tell patients they "can't" do x-y-z then they cheat all out and regret it the next day. The trick to eating "unhealthy" foods and still controlling blood sugar is all in the portion control.
A3: I'm a big fan of cauliflower fried rice - its low carbohydrate and low calorie and counts as a veggie! Especially now that I've been able to find bags of frozen already riced cauliflower at the grocery store. So, in a wok or skillet with non-stick spray or olive oil I mix 1 cup of riced cauliflower, ¼ cup peas and carrots, 3-4 oz of chopped cooked chicken, 2 tbsp low sodium soy sauce, and Salt Free Asian Seasoning blend to taste. Cook until hot/not frozen, and then cook in 1 egg before serving.
Finding substitutions for favorite foods, like cauliflower for white rice, makes controlling carbohydrate intake more enjoyable.
33. Sue Mah

A1: A common “mistake” or misconception is that they must cut out all carbohydrates and sugars. In fact, wholesome carbohydrates can be included as part of a healthy, balanced diet.
Another very common reaction is that the newly diagnosed person may feel fearful of what to eat or not eat. This highlights the importance of providing education and resources to help the patient manage diabetes and still enjoy food!
A2: The best advice is to talk to a registered dietitian for personalized tips that suit the lifestyle and food preferences of the patient. The dietitian can discuss carbohydrate counting and how this will help the patient keep blood sugar under control.
A person with diabetes can still enjoy many of his/her favorite foods with careful planning.
One important tip is to watch portion sizes. For example, one cup is about the size of your fist and is a serving of leafy green salad. A serving of lean meat is about the size and thickness of your palm.
Another tip and key skill is reading labels/ingredients lists. Take time in the grocery store to read food product labels and compare the sugar content. Look at the ingredients list to determine if the food contains added sugars (e.g. look for words such as glucose, fructose, sucrose, honeys, molasses, etc.)
Add more fiber to your diet. Swap out white rice and replace with brown rice. Have whole fruit instead of juice for extra fiber and less sugar. Keep the skins on fruit and vegetables whenever you can.
Enjoy ¼ cup of pulses (beans, peas, lentils, chickpeas) every day. Research from Dan Ramdath at the Guelph Research and Development Centre at Agriculture and Agri-Food Canada showed that eating just ¼ cup of pulses daily can lower blood sugar levels by 20%! Plus pulses are packed with fibre!
Finally, regular activity is key for a healthy lifestyle. Exercise combined with healthy food choices can help a patient better manage his / her blood sugar levels.
A3: This is a recipe for Chicken Lettuce Wraps. The wraps are made with extra lean ground chicken and a variety of vegetables (mushrooms, water chestnuts, red peppers). Instead of bread, the wraps are served in lettuce.
34. Layne Lieberman

A1: People with diabetes cut out sugar and replace sugary foods (like sodas, cakes, cookies and ice cream) with artificially sweetened versions instead of including more wholesome and natural foods. They may make the mistake of choosing artificially sweetened high-fat desserts over fresh fruit. Another common mistake is not realizing that portion size matters, even when eating healthy foods. For example, to increase fiber one may switch from white pasta to 100 percent whole-wheat pasta, without measuring an appropriate portion size.
A2: According to my book Beyond The Mediterranean Diet: European Secrets Of The Super-Healthy, planning is most important for a healthy diet and lifestyle. Always carry healthy snacks like dry roasted unsalted nuts, fresh fruit and carrots. Schedule timing of meals according to the day's activities - whether it means making a restaurant reservation or mapping out when and where you are going to eat --always have a plan.
A3: My tofu meatball recipe is a winner, even for meat-eaters. It's a healthy twist on comfort food, easy to make, heart-healthy, economical, vegetarian and most importantly, it's delicious.
35. Dionne Detraz

A1: A healthy first step I often see people do is switch all their white (refined) foods to whole grain versions (brown rice, whole wheat bread, whole wheat pasta, etc). Although this is great, the mistake that's often made is because it's whole grain they assume they can eat as much as they want and then don't understand when their blood sugars are still running high. Portion control is equally important to switching out refined carbs with whole grains.
A2: Two things. First, skip the bread and chips before the meal. Second, be mindful of alcohol consumption. Alcohol is tricky because it can actually drop blood sugars too low. I suggest that people keep their alcohol consumption only with food and to include some carbohydrate in their meal to help balance out any lows incurred by the alcohol.
A3: A simple grilled salmon with roasted veggies and salad. The protein and healthy fats in the fish are great at stabilizing blood sugars along with increasing satiety. The omega-3 fats can also help improve insulin sensitivity. The fiber in all the veggies helps with feelings of fullness along with blood sugar balancing. For folks who aren't used to preparing fish we might just start with a big salad and canned tuna or salmon. They still get the protein/fat benefit but don't have to actually prepare the fish.
36. Ajita

A1: The most common mistake I see is people assuming that it is just sugar, sweets/ chocolates, cakes, pastries and cool-drinks that they need to avoid. They don’t realize that all carbohydrates (bread, rice, pasta, potato etc), fruit, vegetables and dairy like milk and yoghurt also affect blood sugar as they have a significant amount of carbs in them. The other things they miss is portion sizes , even though they choose low GI/ wholegrains/ fiber containing foods the portions that they eat is still very important for good glucose control. 100% fruit juice is also a frequent mistake that I see – it is a concentrated source of natural sugar and easily pushes blood sugar levels up. Majority of diet plans that I analyze also fall short of protein. Protein is essential to keep blood sugar stable, control cravings and to promote satiety. I correct protein portions at meals and snacks for my clients.
A2: You need to be educated on foods that affect your blood sugar and carbohydrate counting is essential. I teach my clients how the different food groups affect their blood sugar and which groups stabilize their blood sugar. They are also thought how to count carbohydrates which is essential for me – when they know how many carb’s per meal and snack they have then they can make educated food choices and swap foods out to keep the carb’s in correct proportion. This also allows them to have some variations into their dietary plans to prevent becoming bored.
A3: Diabetics usually have a challenge with dessert options. This recipe is called:
Ajita’s Protein Popsicle’s
Ingredients:
125 – 150ml low fat milk
150 – 200ml water
Add 2 scoops Easy Protein Plus Meal Replacement (25g whey protein, no sugar)
½ - 1 tsp chia seeds (optional)
1 Tsp sugar free peanut butter (optional)
Directions:
Blend all the ingredients. Pour into Popsicle moulds.
Enjoy once frozen!
37. Holly Clegg

A1: Diabetes is chronic and people don’t react to a diagnosis with the immediate changes they need too. If they adjust their lifestyle initially, it can help prevent other issues later. Another reaction is people get overwhelmed and think they can never eat what they like again and begin cutting out all carbohydrates and their favorite foods. Portion control, moderate sugar, and low fat are not just guidelines for diabetics to keep in mind, but for everyone’s health, as it really is the healthiest way to eat. There’s no need to completely change your meals, just how you prepare them.
A2: You shouldn’t have to choose between fun, good food and your health, that’s why my passion has always been to create healthy recipes that never sacrifice flavor! With a few simple adjustments, anyone, even those with diabetes, can enjoy yummy food anytime. A couple of tips to tackle those weekend issues would be to have a plan. Be aware of your personalized, dietitian approved meal plan and what foods fit into your healthy diet. Look up restaurant menu’s ahead of time to find out what choices fit into your meal plan. If having a get-together, sign up to bring a healthy dish, one you know fits into your meal plan such as a vegetable tray or a green vegetable side dish. So many trim and terrific recipes are diabetes friendly and delicious so I promise no one will know - your secret is safe with me!
A3: It has to be my Peanut Butter Cookies, and you won’t believe they are diabetic, and honestly, this is my favorite cookie. Every time I give out the recipe it becomes someone else’s favorite peanut butter cookie. If you don’t like the crunch, you can leave out the peanuts and use creamy peanut butter. Confession! I eat cookies from my freezer every night, so when making a batch of these peanut butter cookies, I usually double or triple the recipe to fill up my freezer.
Peanut Butter Cookies from KITCHEN 101 cookbook
Yes, these simple ingredients create a dynamite peanut butter cookie. Sometimes I add chocolate chips too! Makes 30 cookies
Ingredients:
1 cup crunchy peanut butter
½ cup light brown sugar
1 egg
½ teaspoon baking soda
¼ cup chopped peanuts
Directions:
1. Preheat oven 350°F. Coat baking sheet with nonstick cooking spray.
2. In large bowl, combine peanut butter, brown sugar, egg, and baking soda until well combined. Stir in peanuts.
3. Place dough by teaspoonfuls on nonstick baking sheet and press down with a fork to form ridges. Bake 12–14 minutes or until lightly browned.
Nutritional info per serving:
Calories 73, Calories from Fat 57%, Fat 5g, Saturated Fat 1g, Cholesterol 6mg, Sodium 59mg, Carbohydrates 6g, Dietary Fiber 1g, Total Sugars 4g, Protein 3g, Dietary Exchanges: ½ other carbohydrate, 1 fat
Terrific Tip: Use a lightly floured fork to keep fork from sticking to the cookie batter when you make ridges in the cookies.
38. Martha Mckittrick

A1: People are very confused on what to eat. Many of them get very nervous and cut out all carbs. They listen to advice from friends, etc. (“don’t eat carrots, no carbs at all”)
Some people don’t realize that carbs are found in fruit and milk. Most people don’t understand the concept of carb counting - that you can incorporate sweets into your diet on occasion. They become overly focused on cutting back on carbs that they forgot about the concept of a nutritious diet. They may eat too much fat and meat in their quest to limit carbs. Other people have no concept of how many carbs are in foods (like a bagel or order of pasta in a restaurant) they also don’t understand how important losing weight (if overweight) and participating in regular exercise is in helping them control their blood sugar.
A2: Planning ahead. Find out what will be served. Don’t let yourself get too hungry. Have a light snack with protein before you go. Ask if you can bring a healthy side dish. Look at the menu ahead of time to plan what you can eat. Survey your options once you get there so you can make the healthiest choice. If no healthy choices, just stick to small portions. Maybe start with a protein options as studies have shown that eating protein before carbs may help lower the glycemic .
A3: 2 of my favorites that my patients love are zucchini noodles (in place of pasta) with turkey meat sauce AND cauliflower fried rice made with onions, peppers, garlic, soy sauce, ginger, hot mustard, eggs, a little sesame oil and cauliflower rice. It tastes like real fried rice. Both of these recipes contain minimal carbs and calories
39. Olin Idol

A1: In an effort to avoid refined carbohydrates and sugars, they are often advised to include animal protein at every meal. They do not realize it is the fat in animal source foods that over time blunt the cells to insulin, hindering insulin's ability to escort the sugars into the cells, allowing sugars to build up in the blood. In almost all Type II diabetes, a lack of insulin is not the issue. It is the inability of insulin to transport the sugars into the cells where they are needed for energy due to the animal source fats.
Animal protein is harmful to the kidneys and is inflammatory leading to free radical damage. We all need an alkaline forming plant-based diet, rich in fiber to support the body's innate self-healing.
Most Type II diabetics find that when they adopt a 100% whole food, plant-based diet, blood sugars normalize in just a few short weeks. Type I diabetics find that in doing so, they often require only about one-quarter to one-third the insulin needed on an animal based diet.
A2: Adopt a whole food plant based diet. Most chefs will accommodate special dietary request if you simply ask. If in a situation where this is not an option, choose a nice salad, request it be made with Romaine or leafy lettuce. Get a side dish of a healthy vegetable.
A3: Steam Swiss Chard, Kale, or Collard greens with one or two cloves of garlic and add various herbal seasonings of choice.
These green foods are rich in antioxidants, fiber; they are alkaline forming, nutrient dense and low in calories. Some of the healthiest foods we can eat.
40. Michelle May

A1: Understandably, people who find out they have diabetes are scared and may be tempted to try a very drastic diet that is not realistic. While they may see short-term results, a rigid, restrictive diet can trigger feelings of deprivation and cravings, leading to bingeing and guilt. This is really no different from the yo-yo dieting they may have struggled with their whole lives—I call it the eat-repent-repeat cycle. However, diabetes is a chronic disease that requires a sustainable, flexible approach like mindful eating. For example, many people with diabetes believe that they “shouldn’t” eat sugar or “can’t” have carbs. While it is true that a person with type 2 diabetes doesn’t process carbohydrate as efficiently as they once did, they can experiment with different “doses” of carbohydrate with their snacks and meals to figure out how to keep their blood sugar in the target range. (From Eat What You Love, Love What You Eat with Diabetes.)
A2: Don’t diet! The research has proven that most people can’t “stick to a diet” long term so I recommend that people start by examining their relationship with food so they can create an eating pattern they can live with. This Eating Cycle Assessment will help you determine whether you struggle with overeating, restrictive eating, or a combination (as many people do): http://amihungry.com/eating-cycle-assessment/. Then, by learning to use nutrition information as a tool instead of a weapon, mindful eating will help you make decisions that don’t require deprivation. Using awareness and curiosity, you are able to learn about how carbohydrates affect your blood sugar so you can made choices that are satisfying, pleasurable, and help you manage your blood sugar.
A3: I love this delicious, nutritious recipe because it layers fresh flavors and interesting textures. Prepare and eat the salad mindfully, touching and smelling each ingredient, and fully experiencing each bite.
Spinach Orzo Salad with Lemon Dressing
Servings: Makes 10 cups
Carbohydrates: 10 grams per 1 cup serving
Ingredients:
Lemon Dressing
½ cup canola oil (may substitute olive oil)
2 tablespoon lemon juice
2 tablespoons of minced fresh basil leaves (or other fresh herbs)
Ground pepper and coarse salt to taste
Spinach Salad
6 cups of fresh spinach leaves, chiffonade
½ cup of fresh basil leaves, chiffonade
1 cup of dry orzo pasta, cooked per package directions, cooled
2 cups cherry or grape tomatoes cut in half
¼ cup of sliced black olives
2 tablespoons of toasted pinenuts
Directions:
1. Combine dressing ingredients using a hand blender (also called an immersion blender) and refrigerate for at least 2 hours to allow flavors to blend.
2. Toss all salad ingredients with the lemon dressing right before serving.
Note: Chiffonade (a term meaning “rags”) is a simple way to cut strips of spinach, basil, or other flat leaf herbs. Stack 4-5 flat leaves, roll them tightly, and cut ¼ inch slices from the roll.
You can find more recipes at http://amihungry.com/mindful-eating-resources/i-am-hungry-recipes/
41. Sally Marchini

A1: My number one mistake that I see newly diagnosed (and even not just newly diagnosed) people with diabetes making is not having a proper understanding of the foods they’re choosing and how those affect their BGL control. I’ve had type 1 diabetes for 40 years now and it wasn’t until I was diagnosed with coeliac disease on top that I decided to make a career change and study dietetics for my own benefit but also to help others. I had NO IDEA that a dietitian could have taught me so much about making the management of diabetes so much easier. Understanding the relationships between the insulin, activity levels and profiles of various foods and learning to put them into context in our lives completely revolutionised my diabetes control. I only wish I’d been referred many years earlier to see a dietitian.
A2: It is so important to enjoy time with friends and family, and there’s no reason why people with diabetes should feel limited in this respect. Regular checking of BGLs helps you to know how you’re travelling, and of course allowing insulin when needed. And, it’s important to remember that we’re not aiming for a straight line of BGL readings, and that even people without diabetes have blood glucose fluctuations. We just need to bear in mind on these occasions to check and correct as is possible and get back to our routine when the situation allows. Diabetes isn’t a game of perfect, so few slightly higher readings than usual over short periods of time aren’t going to cause long term damage.
A3: Gosh, I love variety in my diet for all the wonderful nutrients that variety brings. To choose one recipe is very difficult! I think probably it would have to be Minestrone soup, which is really a one-pot meal and is packed with flavour, nutrients, legumes and has a good balance of low-GI carbs and lean proteins and good fats to keep our hunger satisfied and our BGLs stable.
This is a very basic recipe for Minestrone, as it can be made with many varieties of ingredients. I hope you enjoy it!
Chop veggies into bite sized pieces – whatever veggies you have e.g. zucchini, carrots, broccoli, pumpkin, sweet potato, and cabbage.
Sauté onion and garlic and some lean bacon in olive oil. Add other veggies. Add 1 litre stock and 2 tins of tomatoes and a couple of tins of legumes (chickpeas or kidney beans are my favourites).
Add herbs, salt and pepper to taste.
Simmer for 20mins and add in some macaroni ten minutes before serving.
Serve with cheese grated on top.
42. Andrew Wade

A1: Most common is the attempt to completely eliminate carbohydrates. While some diets do include this as a potential source of management, oftentimes patients are on medications that require consistent intake of carbohydrate. This means instead of eliminating them, they need portioned and spread across the day to keep a steady level of blood sugar and as a result, energy.
A2: The key is portion and spread of food. You can still enjoy favorite foods, but the excess part of celebrating is what raises blood sugar and stresses the body. Learning to balance food enjoyment, fluid enjoyment, physical activity and socializing is key.
A3: Here is one of my favorite recipes:
Breakfast Recipe
½ cup Oatmeal
1 cup Berries
6oz Almond Milk
⅛ cup nuts
cinnamon
2 Tbsp Raisins
It is slow to digest, loaded with fiber and nutrients, and can be enjoyed hot or cold (overnight oats) depending on the season! Plus the toppings are easy to swap for variety.
I love the Lower Your Blood Sugar Bible. It is a great cookbook with entrees, sides, breakfasts, desserts and it is only $1 on amazon! Recipes include nutrition facts and most take 10 minutes or less.
43. Lauren Moore

A1: The biggest mistake I see clients making is when they decide to go on a diet! Diets are often associated with being short term “quick fixes”, are usually too restrictive and therefore unsustainable, and are often unbalanced and unhealthy. The best thing any client could do is to ditch the idea of a diet, and rather put all their focus on changing their eating behaviours to help optimise their blood glucose by choosing healthier foods and focusing on portions control, together with a regular exercise routine.
Another big mistake is when people go for the “all or nothing approach” and cut out a food just because it contains some carbohydrate. Don’t get me wrong, some foods need to go (processed, refined, sweetened, etc). But just because fruit or dairy contains carbohydrates doesn’t mean they need to be excluded – don’t forget that they contain many other important nutrients which are important as part of a healthy diet.
A2: Be prepared and plan in advance. By doing so, you can shop for healthy ingredients and snacks that you can take with to a social event. This way you won’t be stuck somewhere with no choice but to eat the unhealthy foods that are on offer, which will lead to elevated blood glucose levels. By taking healthy snacks to a party, such as nacho corn chips and guacamole dip, a big salad, or popcorn, you will have healthier options available to you which will help you to keep your portion sizes optimal.
Make sure to stay hydrated in these situations. Drink lots of water to help prevent you from picking mindlessly at snacks – the water will fill your stomach and help reduce your appetite.
Don’t go to a social event hungry. Often there is lots of time to snack before the main meal, and if you are already hungry when you get there you are more likely to snack on junk foods until the main meal is served. Eat a small, balanced snack before you leave for the party to help prevent this type of situation.
A3: Here is a recipe I like:
Chicken Casserole
Ingredients:
4 chicken breasts
1 onion chopped
2 green peppers chopped
1 chicken stock in 100ml boiling water
1 pack patty pans chopped
1 pack bokchoi cabbage chopped
2t split lentils
½t mixed herbs
½t mustard powder
1 tin kidney beans
Freshly ground black pepper
Directions:
1. Mix all ingredients together in a casserole dish
2. Cover and bake at 180°C for 1 hour
3. Remove lid and bake for a further hour
This recipe is so easy to make, you literally just place everything in the pot and leave it to do its thing in the oven. It is packed with fibre from the beans and vegetables, and your portions of veg and lean protein are included in one pot. This recipe also freezes really well, so is perfect for bulk cooking and portioning to freeze for use later on.
44. Susan M. Kleiner

A1: The first mistake is fear. Whether the diagnosis is type I or type II, fear is debilitating to a clear mind, the ability to learn and understand new information and change behavior. Emotion and irrational behavior take over.
The next major mistake is seeking out too many sources of information, rather than finding one certified and reliable source, and following that advice to discover the results.
Finally, jumping on a total elimination diet, e.g. no carbs. No one needs to do that, the data don’t support it, and most people “fail” and then give up, rather than working on incremental steady changes that they can sustain.
A2: Begin to work on connecting what you eat with how you really feel, both short and long term. While “forbidden” foods (there aren’t really any) may seem very appealing at first, once you gain the connection between what you eat and how you feel, you will find that you have more desire for the foods that keep you feeling good for the long term. Then those outings create less dissonance and you if you want to include sweets, for instance, you will be more easily satisfied with less indulgence, and actually prefer those foods that are on your plan and keep you feeling your best.
So while food plans and strategies are important at the outset, its mindfulness, and really mind work, that makes the difference in the long run.
A3: I am a big fan of soups. We know that hydration is key for health and feeling your best all day. Research is also clear that foods with more fluid volume help us stay in control of our diet. This recipe, from my book “The Good Mood Diet”, brings together healthy seafood protein, olive oil fat and a little carbohydrate and good amount of fiber from vegetables, along with important vitamins, minerals and antioxidants that support the systems in our bodies that drive metabolism, immune function, and cellular resilience. It’s also fast and easy!!
Good Mood Diet Manhattan Clam Chowder
The benefits of both vegetable soup and clam chowder with little fat.
Ingredients:
2 tablespoons olive oil
2 onions, diced
4 stalks celery, diced
2 leeks, washed and diced
1 large can chopped tomatoes in juice (28 oz)
1 small can tomato puree (10.5 oz)
3 cups diced peeled and cubed potatoes
1 tsp thyme
1 ½ quarts clam juice
20 oz canned clams,
2 tsp Worcestershire sauce
1-2 tsp Tabasco to taste
Salt and pepper to taste
Directions:
1. In a stock pot, Sauté onions celery and leeks in oil until tender,
2. Add tomatoes, tomato puree potatoes and clam juice
3. Cook 30 minutes or until potatoes are tender.
4. Add clams, salt, pepper, Worcestershire sauce and tabasco Heat until hot.
D5. o not boil it makes the clams rubbery!
Serves 10
* Good Mood analysis: Each serving contains 1 bread; 2 vegetables; 2 very lean protein; 1 fat; also 4 grams of dietary fiber
45. Kelly Jacqueline Ahearn

A1: Restricting total carbohydrate intake too much. It is wonderful that people who have been diagnosed with DM are in the action stage and ready to make changes, however whether it be from misinformation from non-reliant sources or miscommunication with their doctor some people tend to go from too many carbs to not enough. In the past I have had gestational diabetic patients come to me fatigued and very, very hungry. The key is educating the individual and the public that DM does not mean no carb, but instead "slow carb" (high in fiber) and often times LOWER carb than they were consuming prior to their diagnosis. An important thing to remember is that a "low carb" diet for some may actually be "normal carb" intake according to Nutrition standards, and which is why telling someone "everything in moderation," can mean something very different to them vs what it means to the dietitian or person saying that.
I also often see confusion around what exactly is a carbohydrate and which foods have them. Bread is the obvious one, dairy (milk and yogurt) is lesser known to contain carbohydrates. In today's world with all of the functional food products on the market it is important to communicate to the person newly diagnosed that even though via guidelines a piece of bread may be 1 carb serving to check the nutritional label as some low carb breads on the market contain only 5 grams vs 15 which is ⅓rd a carb serving. By educating and empowering the patient to read and understand the labels this will help to ensure they are consuming the correct amount of carb servings in a meal or snack for their specific needs.
A2: Bring your own dish: If you have a family and/or friend gathering and are well aware of what is about to be served up (chips, cakes, heavy dishes, etc.) then this is your chance to be the heathy influence. By bringing the salad to the table (literally and figuratively) you know that there is at least one thing that is a healthy choice for you to stay on track in the midst of less healthy options. I bet everyone will also dig in!
Do not go to the outing starving: I often see people starve themselves during the day to get ready for a big dinner. It is perfectly OK to eat LESS during the day, however to skip eating in general can set the body up for fatigue, and when it is time to eat the eyes are often bigger than the stomach. It is also taxing on the digestive system and the pancreas to eat a large amount of food in a small amount of time after a day of fasting. Eat a protein rich balanced snack such as a hardboiled egg with 1 piece of toast an hour or so before the dinner or event or nuts and an apple to ease into the scene. Don't skip lunch; however it is ok to have something much lighter.
Which leads me to this: EAT SLOWLY: This may be the hardest of these tips to follow. Studies and personal travels show that the French eat their meals leisurely filled with some of the best full fat cheeses, wines, and multiple courses. The French also have a lower rate of heart disease than Americans and a lower body weight. We cannot say that eating slowly alone is the only reason for this; however what some observations do show is that these longer meals spent with friends and family people actually consume less calories. It takes around 20 minutes for the stretch receptors in the stomach to tell the brain it is satisfied so small bites and longer meal times help these cues to kick in resulting in overall less food eaten vs eating a foot long sandwich at your desk before a meeting.
Move: Never underestimate the body's ability to move. It is a blessing and even 1 minute is better than spending that minus sitting. Research has shown that an after meal walk helps the body utilize some of the blood glucose (sugar) for energy therefore helping to keep blood glucose levels in check. Too cold or hot outside for a walk? Walk around your room, dance, circle your arms- ANYTHING is better than nothing. I just would not recommend eating and doing an intense activity such as run right away as this may be upsetting to the digestive system. Leisurely activity is best.
A3: Now that I have relocated to the UAE for 2 years to work and to help set up an outpatient clinic I am having fun enjoying the local cultural foods, especially the "Mezza," which are small plates of different dishes. Below is a recipe adapted from Michael Solomonov at Eating Well. I have made one change to make it more diabetic friendly.
* Cook 40 m
* Ready In 3 h 15 m
Recipe By: Michael Solomonov “Walnuts, red onion and dill make this roasted beet salad recipe a fantastic accompaniment to chicken or topping for hummus. If you can't find beets with greens attached, use 1 pound of beets and 8 ounces of chard leaves.”
Ingredients:
1½ pounds baby beets with greens attached (or pre cooked beets, stems removed)
1 head garlic
4 tablespoons extra-virgin olive oil, divided
¾ teaspoon kosher salt, divided
1 cup distilled white vinegar
2 tbsp Coconut sugar or nectar, Honey may also be used.
½ cup finely chopped toasted walnuts
¼ cup finely chopped red onion
¼ cup chopped fresh dill
Directions:
1. Preheat oven to 325°F.
2. Rinse beets well. Cut off the greens, and then cut the leaves off the stalks. Set the leaves and stalks aside. Remove excess papery skin from garlic head without separating the cloves, and then cut the head in half horizontally.
3. Toss the beets, garlic, 2 tablespoons oil and ½ teaspoon salt in a small baking pan, such as a bread pan. Cover with foil. Roast until tender, 1 to 1¼ hours. Let cool slightly.
4. Whisk vinegar and sugar in a medium bowl. Squeeze the garlic cloves out of their skins into the bowl. Peel and dice the beets; add to the bowl. Let marinate at room temperature for at least 2 hours and up to 1 day.
5. Finely chop the beet stalks and very thinly slice the greens; place in a large bowl. Scoop the beets from the pickling liquid with a slotted spoon and add to the bowl. Drizzle the beet mixture with ¼ cup of the pickling liquid. Add walnuts, onion, dill, the remaining 2 tablespoons oil and ¼ teaspoon salt and gently toss to combine.
Make Ahead Tip: Prepare through Step 4, cover and refrigerate for up to 1 day; finish Step 5, cover and refrigerate for up to 1 day more.
Walnuts, red onion and dill make this roasted beet salad recipe a fantastic accompaniment to chicken or topping for hummus. If you can't find beets with greens
46. Ellen Albertson

A1: Believing that only diet and food impact blood sugar levels. Many other factors play a role including stress, exercise/activity and sleep. Another big mistake is taking an all or nothing approach. They feel that unless their diet is perfect why bother. Or if they make a mistake and over eat they beat themselves up and want to quit. I encouraged them to take the Goldilocks’s approach and work with a nutritionist or wellness coach to find the diet (not too hot or too cold) that works for them. Another issue is focusing a ton of energy on what you can’t eat instead of focusing on being healthy and enjoying foods that are good for you. A final issue is newly diagnosed people usually don’t take the time to process the diagnosis. Often they want to dive right in and fix everything before having a chance to grieve. Taking time to process the diagnosis and offering yourself compassion for how you’re feeling is important. After processing the diagnoses they are ready to move into the planning and then action stages of change so they can live healthy lives.
A2: Rather than denying yourself, choose carefully and enjoy the 1 or 2 foods you love in moderation. Then fill the rest of your plate up with low calorie veggies. You should also bring a dish that you like that is low in calories so you have something healthy to enjoy. I also recommend having a snack prior to the event so you aren’t starving, slowing down and eating mindfully and enjoying all the nonfood fun from catching up with old friends to playing with your kids.
A3: I really like the recipe from our book: The Diabetic & the Dietitian: How to Help Your Husband Defeat Diabetes Without Losing Your Mind or Marriage for Veggie Burritos. They are high in fiber, easy to make, freeze beautifully and are great cold the next day for lunch. Plus, it’s family friendly.
Ingredients:
1 can (16 ounces) vegetarian low-fat or fat-free refried beans
1 1-pound bag frozen mixed vegetables
1 cup cooked brown rice
1 teaspoon garlic powder
1 cup salsa
4 ounces (about 1 cup) shredded reduced-fat Mexican
cheese blend
6 8-inch whole-wheat flour tortillas
Directions:
1. Preheat oven to 350° F. Coat a baking dish with nonstick cooking
spray.
2. In a large bowl combine refried beans, vegetables, rice, garlic
powder, ½ cup salsa, and ½ cup cheese.
3. Put 1 tortilla on a plate. Spread about 1 cup of the bean, rice,
vegetable, and cheese mixture in the tortilla, roll up, and place in
prepared pan. Repeat with remaining tortillas.
4. Spread remaining ½ cup of salsa over the wrapped tortillas and
top with remaining cheese. Bake in preheated oven until
cheese is browned, about 30 minutes.
Dr. Ellen is a Psychologist, Registered Dietitian Nutritionist and Certified Wellcoach®. She has 20+ years experience helping people go from stuck to satisfied and live balanced, vibrant, healthy lives. She’s the author of 4 books including, The Diabetic & the Dietitian: How to Help Your Husband Defeat Diabetes Without Losing Your Mind or Marriage. You can contact her at DrEllenAlbertson.com
47. Julie-Ann Muldoon

A1: People panic and read too much on the internet then stress themselves about the conflicting advice available- they try to run before they can walk. They embark on too many changes and then feel like they are failing. They also listen to too many goodwill friends and family which makes the new diagnosis even more stressful. Another mistake is going out to buy specialist expensive foods that are not required or recommended. With a new diagnosis people are very vulnerable and so they are relieved to speak to me about their fears and feelings and get correct information that is easy to implement.
A2: Top tips to eat well for blood sugar control and enjoyment: "focus on the positive and not the negative"
a. Eat regularly - do not skip meals: crucial if taking medication and also to stop being tempted by unnecessary snacks.
b. Ensure that the foods chosen follow a colorful collection of good quality choices. This therefore does not eliminate foods but focuses on the quality of ingredients and cooking methods employed.
If eating out, I recommend avoiding the fast food processed outlets and eat in good quality restaurants. Here, if wanting a fast food replica - you can still select the 100% beef, chicken, fish or bean burger (with/or) preferably without the bun, and select a large colorful salad and a few sweet potato chips. Avoid the unhealthy sides.
Eating when at home again it is all about focusing on good quality foods; healthy proteins like fish, chicken, pulses, eggs and plenty of vegetables and long acting carbohydrates. This allows for tip top health to be achieved and when eating out some tasty choices can be made!
c. I also recommend savoring and tasting each mouthful and enjoy the family and friend experience. the food is not the only pleasure to focus on. People can get too hung up about food avoidance and in fact when they come to see me it is often my job to encourage additional foods into the diet and thus more choice, more taste and more variety = more enjoyment.
d. If wishing to have a dessert: I suggest people are strong and think things rationally and not get upset as there are always options. With diabetes, raised blood sugars are really what you want to avoid. If it is a special occasion then sharing a pudding with someone after a meal can be doable depending on your medical situation. If blood sugars are not stable then avoiding a dessert may be the correct thing to do and have a little cheese and crackers/ tea or coffee and a square of dark chocolate and some almond nuts.
A3: Gosh there are hundreds of fab recipes that Diabetic people can enjoy. Nothing I feel is truly forbidden other than; junk (nutrient devoid foods), obvious sugar and hidden sugars.
A simple and effective recipe for feeling full and maximum taste include: 2 eggs scrambled on the pan with a large portion of wilted spinach and 4 cooked baby plum tomatoes.
This is a great meal any time of day. It can be eaten hot from the pan but also cooked and transported for lunch or on the go after a sporting activity. Young and old can enjoy this versatile filling meal.
Eggs are inexpensive and provide good quality protein. More than half the protein of an egg is found in the egg white along with vitamin B2. The whites are rich sources of selenium, vitamin D, B6, B12 and minerals such as zinc, iron and copper.
Spinach is high in niacin and zinc, as well as protein, fibre, vitamins A, C, E and K, thiamin, vitamin B6, folate, calcium, iron, magnesium, phosphorus, potassium, copper, and manganese. Tomatoes are also a good source of potassium, manganese, magnesium, phosphorous, and copper. Tomatoes also have dietary fiber and protein, as well as a number of organic compounds like lycopene that also contribute to the overall health benefits.
People with diabetes need to eat nutrients and what better way to get them than from this nutrient rich trio.
48. Sherry Greek

A1: A common mistake I see among those with newly diagnosed diabetes is counting carbs based on foods with nutritional labels, rather than choosing whole foods. It seems easier to count carbohydrates at meals when a label tells you the amount, but the nutritional adequacy of the food may be lacking. Being newly diagnosed with diabetes is overwhelming at first, but choosing whole food carbohydrate sources will do better for your body in the long road and lead to better outcomes.
A2: Go with a plan. Planning ahead will allow you to feel more relaxed when you are in the moment and want to enjoy time with your friends and family. If you're going to eat at someone's house, bring a dish you can easily count carbs for and allow some wiggle room for other people's food. If you are going out to eat, look at the menu online ahead of time so there's no worrying while you are out.
A3: Go with a plan. Planning ahead will allow you to feel more relaxed when you are in the moment and want to enjoy time with your friends and family. If you're going to eat at someone's house, bring a dish you can easily count carbs for and allow some wiggle room for other people's food. If you are going out to eat, look at the menu online ahead of time so there's no worrying while you are out.
49. Lily Nichols

A1: The number one mistake I see in newly diagnosed diabetics is not checking blood sugar levels. Maybe you’re afraid of poking yourself, you think it will hurt, or you’re nervous about seeing a high number. These are all common, however if you ignore or “conveniently forget” to check your blood sugar too often, your doctor will have no way of knowing how you are doing. Think of blood sugar numbers as information rather than something that is inherently "good" or "bad". You need this information to make decisions about what to eat and how to manage your diabetes.
A2: Eat mindfully. That means, regardless of what you eat, you savor every bite, you eat when you're hungry, and you stop when you're full.
A3: I like this recipe for baby broccoli with bacon because it's a delicious way to fit more vegetables into your life. Plus, who doesn't like bacon?! It's also naturally low in carbs, meaning it won't cause your blood sugar to go up.
50. Erin Macdonald

A1: I find that they don't balance their macros. Simply switching from white rice to brown rice is not enough. Reducing carb intake and increasing protein and healthy fats are much more effective for keeping blood sugar at a healthier level. Also, choosing plant-based carbs over refined, processed carbs is so important. All carbs are not created equal and those with fiber and antioxidants are much better for blood sugar control and inflammation. Lastly, meal timing is very important. Do not skip meals.
A2: First, make sure to have your routine in place. This would include staring the day with a high-protein breakfast, getting in exercise - both cardio and weight training, and consuming macro-balanced meals on a regular schedule. When eating out, decide what it is you really want to have. Is it pizza? Alcohol? You can make it fit as long as you consume a smaller amount and make sure to have other foods that contain fiber, protein, and fat to help balance our blood sugar levels.
A3: I love to make frittatas because you can put pretty much any combination of vegetables together and make a new flavor profile every time! In this one, I've added omega-3-rich smoked salmon, which adds a ton of flavor and is anti-inflammatory.
Smoked salmon and shallot frittata (serves 4)
Ingredients:
4 large eggs
3 egg whites
zest of 1 lemon
1 tbs. lemon juice
½ tsp. lemon pepper
¼ cup chopped shallot
3 oz. smoked salmon, chopped (make sure it's wild Alaskan salmon, not Atlantic salmon)
1 cup baby spinach
1 oz. goat cheese, crumbled
2 tbs. chopped chives
Direction:
1. Preheat oven to 350F. Coat a glass 9-inch pie plate with olive oil cooking spray.
2. In a bowl, whisk together the eggs, egg whites, lemon zest, lemon juice, and black pepper. Ad the shallot, smoked salmon, goat cheese, and baby spinach. Pour into glass baking dish and place in oven to bake for 23-25 minutes.
3. Remove from oven and sprinkle with chopped chives.
51. Katie Ann Lehn, RD

A1: Newly diagnosed diabetics often feel the need to remove all carbohydrates from the diet. While they’re on the right track by becoming mindful of carbohydrate consumption, there is no need to eliminate all from the diet. Carbohydrates are an important fuel source for our brain cells and also serve as a quick energy source, especially during exercise. Rather than eliminating all carbs, it would be more beneficial to eat a small, consistent amount with our three meals daily.
Another common diet change seen in new diabetics, is the use of artificial sweeteners. This includes Splenda, Sweet n Low, Equal, etc. Yes, artificial sweeteners will not raise someone’s blood sugar like sugar will; however, they are accompanied by risk factors of their own. Artificial sweeteners have been linked to increased cancer risk, negative alteration in our gut microbiome and have also been thought to further increase our bodies craving for sweets.
A2: Suggest activities that don’t revolve around food such as a hike, going to the park, playing a group sport (touch football, Frisbee, soccer), crafting or playing bored games.
Bring healthy food options to gatherings with family and friends. This way you know there will be at least one thing you’ll feel safe to eat.
Plan ahead. Make sure you keep to a normal eating schedule during weekend actives. Have a healthy snack option with you at all times in case of emergencies: nuts, dried/fresh fruit, natural jerky, fruit and nut bars without added sugar.
Create your own “Diabetes Care on the Go Kit” to have ready for a spur of the moment adventure. This could include: a blood sugar monitor, insulin (if prescribed), a water bottle, emergency snacks, and a cold pack (to keep the insulin at the right temperature).
A3: This is one of my favorite diabetes friendly dishes. Why? Because everyone loves it, not just those with diabetes! This veggie-tastic dish is rich in anti-inflammatories, like the flavonoid, quercetin from ginger. Reducing inflammation plays an important role in managing diabetes. Not to mention, it’s packed with flavor!
Szechuan Green Beans
Ingredients
1 pound fresh green beans
4 scallions
6 cloves garlic, roughly chopped
1 inch fresh ginger, minced
¼ to 2 teaspoons red pepper flakes (adjust for desired heat)
1 teaspoon whole peppercorns, divided
3 tablespoons olive or avocado oil, divided
Sea salt to taste
Directions:
1. Trim stems off green beans and place in a large bowl.
2. Thinly slice scallions, using the both the white and green parts. Set aside in a small bowl.
3. Mince garlic. Add to scallions.
4. Remove peel from ginger using a paring knife. Grate fresh ginger using a fine cheese grater or mince finely. Add to scallions and garlic.
5. Add red pepper flakes to scallion mixture.
6. Grind peppercorns.
7. In a medium skillet, heat 2 tablespoons oil over medium-low heat. Add half of the peppercorns and stir frequently, until aromatic, about 1 minute.
8. Add the scallion mixture and cook about 1 minute longer. Remove from heat and set aside.
9. Adjust oven rack to the highest shelf. Preheat the broiler to high.
10. Toss green beans in 1 tablespoon oil and season with salt and pepper.
11. Spread green beans out in a single layer on a foil-lined baking sheet. Broil until very lightly charred, about 3-5 minutes. Return to bowl.
12. Toss green beans in half of peppercorn mixture. Plate green beans and top with remaining peppercorn mixture and serve.
I had a difficult time choosing only one recipe so here is another! I love this recipe for diabetes because it encourages getting creative with unprocessed, carb dense foods. Parsnips are a less common carbohydrate choice and this quick & easy dish is a great way to try them out for the first time!
Garlic Rosemary Parsnip Fries
Ingredients:
1-2 large parsnips (or 2-4 smaller ones)
1 tablespoon avocado oil (or extra virgin olive oil)
3-6 cloves of garlic
2-4 sprigs fresh rosemary (or 2 teaspoons dried)
Salt and pepper to taste
Directions:
1. Preheat the oven to 400 degrees.
2. Line a baking sheet with parchment paper.
3. Cut parsnips into shoestring size pieces and place in a mixing bowl.
4. Drizzle the parsnips with oil and toss until they are coated.
5. Remove dry outer casing of garlic and chop finely.
6. Remove rosemary leaves from the stems and chop finely.
7. Sprinkle garlic and rosemary over parsnips and toss to combine.
8. Season with salt and pepper.
9. Bake for 15-20 minutes. Remove from the oven and toss the fries.
10. Place back into the oven and back for another 15-20 minutes, until they have reached your desired crispiness.
52. Rahaf AlBochi

A1: One of the biggest diet mistakes that newly diagnosed people with diabetes make is avoiding all carbohydrates- breads, pastas, rice, potato (“all things white”), and even fruits! They believe that they need to live on vegetables and meat to have good blood sugar control. That is far from the truth and as a Registered Dietitian and Diabetes Educator my role is to clarify this misconception. When people with diabetes avoid all carbohydrates they become at risk for great fluctuations in blood sugars, both low and high. It is important that people with diabetes understand that carbohydrates are part of a healthy eating pattern. Focusing on portion control and including foods high in fiber, such a whole grains, whole fruits, and vegetables will help with reaching good blood sugar control. Examples of whole grains are oats, whole wheat flour, brown rice, barley, freekeh, and quinoa, to name a few.
A2: One of the most important tips for people with diabetes who want to spend time with friends on the weekend is to avoid skipping meals. Aim for a meal every 4 to 6 hours so you maintain steady blood sugars and energy levels. Carry with you a power snack, such as a trail mix, protein bar, or fruit in case meals are delayed. If you are planning a dinner outing with your friends, make sure that you have a well-balanced breakfast and lunch, and possibly even an afternoon snack before your dinner outing. This helps you maintain good blood sugars throughout the day and at dinner because you are less likely to overindulge and risk high blood sugars. Also, if you are on diabetes medications make sure you bring them with you and set yourself a reminder so you don’t forget taking them.
A3: One of my favorite diabetes friendly recipes is this 7 Ingredients Blueberry Baked Oatmeal Cups. Many people don’t have time in the morning for breakfast so making breakfast ahead of time will help make sure that you don’t skip it. Eating a well-balanced breakfast is important for all people, especially if you have diabetes. Oats are an excellent breakfast food because they have a type of fiber called beta-glucagon, which has been shown to reduce cholesterol levels and improve blood sugars. These oatmeal cups are simple to make and taste delicious.
7 Ingredients Blueberry Baked Oatmeal Cups
Ingredients:
3 cups old fashioned oats
1 tsp cinnamon or nutmeg
1 tsp baking powder
4 tbsp honey
2 eggs
1 cup milk
1 cup blueberries, fresh or frozen
Time: 40 min
Servings: 12
Directions:
1- Pre-heat oven to 350oF
2- Combine the dry ingredients (oats, cinnamon, baking powder) and wet ingredients (honey, eggs, milk) in separate bowls, then mix the dry mix into the wet mix and stir.
3- Spray oil or wipe down a 12 cup muffin pan with oil to prevent mixture from sticking once baked.
4- Scoop the oat mixture into the muffin pan and top each muffin with blueberries.
5- Bake for 30 minutes or until the mixture thickens.
6- Store in airtight container for 3 days or in the fridge for 7 days or freeze for up to 3 months.
7- To eat, heat up in the microwave or enjoy as is!
53. Courtney Ferreira

A1: Common diet mistakes involve portion sizes. For someone who is not used to measuring foods and paying attention to portion sizes, adapting these habits can be challenging. When the new nutrition facts label rolls out in 2018 a lot the guess work will be taken out of determining nutrient content of packaged foods, but for now it can be tricky! People may assume that a cup of juice means one cup from their cabinet filled with juice, when in fact it means 8 fluid ounces, which isn’t much at all! It can be easy to underestimate the amount of carbohydrates being consumed if these foods are not measured diligently.
A2: Always have a plan! You are human; if you leave it up to yourself to make the decision in the moment when you might be hungry or tempted by what others are eating, then you are setting yourself up for failure. Preparation is what leads to success. If you are going out to eat look at the menu ahead of time and plan what you will have. It is okay to indulge here and there but treat yourself to foods that you really love, eat slowly and savor, and don’t stuff yourself. Oftentimes high blood sugar is a result of eating too much. You can get a taste of something delicious and carbohydrate dense without needing to clean your plate. If you are gathering at someone’s house, bring your own dish. Also, don’t be shy to ask about what is in a dish if you are unsure. Sugar is hiding in a lot of unknown places; it is okay to want to be educated about what is in your food to prevent surprise blood sugar spikes.
A3: Crustless egg bakes are loaded with protein, nutrients, and healthy fats and are extremely low in carbohydrates. Pair with a serving of fruit (example: small apple, half a grapefruit) for a perfectly balanced breakfast. This recipe is awesome because it will help you feel satisfied, stay full, and prevent blood sugar spikes and crashes. Stable blood sugar is the goal and a morning egg bake with a small amount of carbohydrate from fruit or vegetable will help you get the day started right!
Ingredients:
Butter for greasing the pan
Eggs (12 for six pieces, 8 for four pieces)
1- 6oz bag of fresh spinach, can use frozen
~½ c other veggies
salt and pepper to taste
optional: heavy whipping cream, cottage cheese
Directions:
1. Preheat oven to 375 degrees.
2.Grease baking dish (9x13 for 12 eggs, 8x8 for 6 eggs) liberally with butter.
3.Whisk all of the ingredients together. Pour into the greased pan and bake for 35-40 minutes or until the edges begin to brown and the middle is no longer watery.
4.Let cool for 10 minutes before slicing.
54. Mary Jane Detroyer, MS, RDN, CDN

A1: I have found a few things that clients who are newly diagnosed with diabetes often do. One is that they eliminate all starches and fruits only allowing themselves to eat protein and vegetables. Some just totally avoid fruit because they have been told to by doctors and others. A third is using fat free dairy products. When you have diabetes you should eat low fat but not fat free dairy because the fat helps to slow the way the milk sugars are absorbed.
A2: When going out to dinner check the menu before hand and determine what you will order that will not cause your blood sugar to sky rocket. If you are at someone’s home and the food is not your choice choose your portions wisely, don’t allow people to force you to have second helpings if you are satisfied. If you feel the meal may cause your sugar to go high you can discuss with your doctor, ahead of time, how to cover that meal with extra insulin or medication. Doing this once in a while is not a problem. Doing it regularly to allow yourself to eat too much or none supportive foods is dangerous.
Eat your protein and veggies before starch. Research shows that this can help to control BG better.
Eat mindfully, check into hunger and fullness cues and stop when you are comfortably full. Eat intuitively that means look at all the options on the table or the menu. What looks good to you. Weigh your options. Are you really craving the pasta and meatballs or would you be just as satisfied with some grilled fish, a steak or chop and having half a baked potato and veggies or skipping a starch with your entree and sharing a dessert with someone. It is not just the type of food that people need to consider but the amount of food that impacts the production of insulin and ability to quickly remove the BG after an overly large meal.
If you are on an outing bring foods with you that you know fit into your eating plan so that you won’t be overly hungry and go for the sweet, starchy snacks we all look for when our blood sugar drops. Nuts, fruit, cheese and whole grain crackers, the new beef, turkey and chicken jerky products, wasabi roasted dried edamame, roasted soy nuts.
I don’t know if this recipe is my favorite recipe for my clients with diabetes. I try to teach all my clients how to be able to eat all foods in a way to maintain their blood glucose levels. Once in a while it is okay to eat foods that might make the sugar go up but that does not result in elevated A1cs or complications if it is something happening at maybe one meal a week.
A3: Here is a great recipe:
Barley and Turkey Stew
Ingredients:
8 oz. turkey cutlets cut up in bite size pieces
8 oz. of mushrooms sliced (substitute zucchini, baby bok choy, eggplant or peppers)
1 small onion diced
4 large carrots sliced or diced
2-4 cloves of garlic, minced
2 Tbsp. basil, dried (may substitute other herbs like tarragon, thyme, marjoram, oregano or a mix)
½ cup dry barley
1 ½ cups low-sodium chicken broth
2 Tbsp. Worcestershire sauce
1 Tbsp. oil
Directions:
Sauté onion, garlic, carrots and mushrooms for 2-3 minutes over med-high heat. Add turkey and cook until turkey is no longer pink. Rinse the barley with water and add to pressure cooker with remaining ingredients. Cover and bring to high pressure and cook at high-pressure for 18 minutes. If using a regular pot cook for 45 minutes or until the barley is chewy. When cooking in a regular pot you might need to adjust the fluid up or down. Servings: 2 large or 3 smaller servings.
55. Ginger Vieira

A1: Suddenly fearing all carbs and consuming tons of alternative sweeteners: Alternative sweeteners are useful here and there for certain things but the research on how they really impact our bodies is still unclear and controversial. Instead of trying to eliminate all carbs in your diet, spend a few days really tracking how many carbs you currently eat and then thinking about what parts of the day and what meals you'd like to start improving by reducing processed carbs and including more whole foods, more healthy proteins and fats and non-starchy veggies.
A2: Micromanaging your child's diet: When a child is diagnosed with type 1, there's nothing more stressful a parent can do than to try and control everything that goes in their mouth. They can eat dessert (see below). They can go trick-or-treating. They can go to birthday parties. It's all about learning what approach to covering those treats with insulin works and what doesn't. Trial and error. And of course, lots of blood sugar checks when you're eating foods that have less certainty around them. Trying to control everything your kiddo eats is only going to backfire in a multitude of ways.
Thinking that you can't eat dessert again...unless you're being "bad": You can eat dessert as a person with diabetes! Type 1 or type 2! But the carbs in that dessert need to be accounted for and fit into the bigger picture of your day. If I know I'm going to a wedding on Saturday and I want to indulge in delicious cocktails and wedding cake, I can cut back my carb-consumption throughout my other meals on both the actual day of the event and even the day beforehand (and the day after), too. It's all about balancing the bigger picture. If having a small bowl of ice cream is one of your favorite treats in life, then make room for those carbs by reducing the carbs in other meals of your day.
Balance! There's nothing wrong with enjoying pizza and beer one night on the weekend if the rest of your week was in line with your nutrition goals. The goal is not 100 percent perfection. Even athletes have "treat-days." If you're in-line with your overall nutrition goals and diabetes goals during the week, and you're thoughtful about dosing your insulin and what "treats" you consume on the weekend, you can still be healthy and socialize with your friends and family. It's all about balancing the bigger picture in a way that works realistically for you.
A3: The "flaxseed muffin in a mug" is pretty awesome. The taste doesn't appeal to everyone but with butter or peanut butter on it, I think it's pretty awesome. It takes mere minutes to make, it's extremely low-carb after subtracting the fiber, and it's loaded with healthy fats and fiber and protein!
56. Vadym Graifer

A1: People newly diagnosed with type 2 diabetes face a choice that can influence their entire life. Remarkably, many of them don’t even know there is a choice. It’s a mistake to accept the commonly given verdict: “Diabetes is a chronic, progressive disease and your condition will worsen over time. So, cut some sugars but continue eating high carbs and take your meds, there is nothing you can do about it anyway.” I am exaggerating a bit here, but the underlying message is exactly this, even if the actual words aren’t this harsh.
The other choice is to realize that type 2 diabetes can be controlled, and in many cases reversed, by correcting one’s nutrition. I am not talking about an extremely limiting diet that would make you miserable. It’s about switching to real foods as opposed to manufactured concoctions that are stuffed with additives and, worst of all, added sugar and simple carbohydrates which harm our bodies in very real ways.
It’s in your power to implement time-tested patterns of eating that could return your blood sugar to a healthy range. This worked for many people; this worked for me. I described the whole approach and my journey that saw me lose 75 pounds and eliminate the need for medications in my book The Time Machine Diet.
A2: You don’t have to be “that guy” that rejects dessert citing his diagnosis. As long as it’s not an everyday habit and you keep a lid on quantities, you can apply some protective strategies to minimize the damage:
- Make sure that you eat something rich in fiber, protein or fat with your sweets, to slow down sugar digestion. Leafy greens, a vegetable, handful of nuts or a piece of cheese will work;
- Sneak in a tablespoon of apple cider vinegar diluted in a cup of water. It slows down digestion as well;
- Plan a physical activity after your dessert to quickly burn off the extra sugar. If your outing includes playing outside, all the better! Even a brisk walk will do wonders for your blood sugar.
Most importantly, make even your indulgences real food. Think homemade dessert with heavy cream, dark chocolate and whole fruit instead of an industrial creation consisting of partially hydrogenated oil, high-fructose corn syrup and a rainbow of flavorings, colorings and preservatives.
You don’t need to eat junk food to have a happy time with your friends and loved ones. Work out your food approach that is healthy and tasty, and let your friends and family discover what many of us, “T2Ds” did: Healthy can be delicious.
A3: There are all kinds of fantastic diabetes-friendly recipes. The most popular among them are those that replace formerly enjoyed foods with their healthy equivalents. One of such is a celery root, or celeriac, used as a potato substitute. At ⅓ of carbs and half the calories, it’s amazingly tasty. Peel and cut celery root in half-inch cubes. Pour 3 tbsp olive oil in frying pan and put it on high heat. Add celery root, stir to coat and add pressed garlic, salt to taste, and spice it up with dried rosemary, black pepper or other spices you favor. Fry for 5-10 min until golden. Add 3-4 tbsp water and cover. Roast for 20-25 minutes. Serve hot.
57. Jesus Hernandez

A1: In my previous experiences the most frequent mistake I’ve encountered is newly diagnosed individuals skipping meals. This will lead to a rollercoaster like effect on blood glucose levels which can lead to complications such as hypoglycemia.
A2: The number one tip I would recommend would be to plan ahead. For instance, when going out to dinner with friends and family look ahead at the menu for options that fit your dietary needs. Another example would be to carry quick and easy snack options in case your blood sugar drops throughout the course of the day.
A3: One of my favorite diabetes friendly recipes is Roasted Chicken and Sweet Potatoes from Eatingwell.com. This dish is the perfect balance of protein and complex carbs to help stabilize blood sugars and it packs a ton of flavor. It’s also pretty easy to prepare and makes great leftovers for lunch the next day. You can even make it in the crockpot!
58. Lisa Eberhart

A1: Portion size, especially things like rice or pasta, eating a larger portion than allowed. Not understanding or underestimating the impact juices and sugar sweetened beverages can make on blood sugar.
A2: Stick to whole foods, have more unprocessed foods like vegetables on the plate, if half the plate is vegetables you are probably doing pretty well. Drink water and only water. Weekends with family and friends should be active time, a time to move around, exercise walk, bike hike. Look at portion sizes. If out to dinner split the entree and either share or take half home for tomorrow’s meal.
A3: Cauliflower rice is VERY low in carbs and will have a minimal impact on blood sugar. It can be made into a stir fry that is delicious with some grilled chicken or fish.
You can make it or you can buy it frozen in bags in the frozen section.
1. Wash and thoroughly dry cauliflower, then remove all greens and cut into 4 even sections (see photo).
2. With a box grater, use the medium-sized holes (see photo - the side commonly used to grate cheese), or a food processor with the grater attachment, to grate the cauliflower into the size of rice, leaving any large, tough stems behind.
3. Transfer to a clean towel or paper towel and press to remove any excess moisture, which can make your dish soggy.
4. Once you have your cauliflower rice, it's easy to cook! Simply sauté in a large skillet over medium heat in 1 Tbsp oil. Cover with a lid so the cauliflower steams and becomes more tender. Cook for a total of 5-8 minutes, then season as desired
5. Use cauliflower rice in recipes that call for rice.
Cauliflower Fried "Rice"
Serves 4 to 6
Ingredients:
2-3 cups cauliflower rice
¼ pound (4 slices) thick-sliced bacon, optional
2 large eggs
1 tablespoon minced ginger
3 cloves garlic, minced
2 medium carrots, diced (about 1 cup)
1 cup corn, fresh or frozen
½ cup peas, fresh or frozen
4 green onions, thinly sliced
¼ cup cashews, almonds, or other nut
2 to 3 tablespoons soy sauce (or if gluten-free, 1 to 2 tablespoons tamari)
Directions:
1. Cook the bacon in a 12-inch skillet over medium heat until crispy. Transfer to a plate lined with a paper towel to drain. Wipe out the pan.
2. Place the pan back over medium-high heat. Whisk the eggs and pour them into the skillet. Quickly scramble the eggs. Transfer the eggs to a cutting board and roughly chop into pieces.
3. Wipe the skillet clean and warm 1 tablespoon of canola oil over medium-high heat. Add the ginger and garlic, and sauté until fragrant, about 30 seconds. Stir in the carrots and sauté until crisp-tender, 2 minutes. Stir the corn, peas, and cauliflower "rice" into the pan, mixing the ingredients thoroughly.
4. Lower the heat to medium, cover the pan, and cook until the cauliflower is tender, 5 to 8 minutes. Uncover and stir in the bacon, eggs, green onions, cashews, and 2 tablespoons soy sauce. Taste and add more soy sauce to taste. Serve immediately.
5. Leftovers will keep refrigerated for about a week.
59. Diana Rodgers

A1: The biggest mistake I see people with diabetes make is eating too little protein and too little healthy fat. Protein (especially in the form of meat) and healthy fats (like avocados and nuts) are your friends and can help control blood sugar spikes. I also see people constantly looking for diabetes friendly treats instead of making the decision to change their eating patterns to more of a “real food” way of eating, meaning less processed foods. Read this post for more on my thoughts about how diabetics should eat.
A2: Tips for enjoying family time on the weekends would be to bring a healthy option (like a protein dish) to eat to any gathering and not just hoping there will be a good option. Go to the party with a full stomach, and have a plan in your mind about what you’re going to eat while you’re there.
A3: Both of my cookbooks feature recipes that are perfect for those who are trying to prevent or control diabetes. A great way to start the day would be with my Tuscan Hash from Paleo Lunches and Breakfasts on the go http://sustainabledish.com/poached-egg-with-tuscan-hash-paleo-lunches-and-breakfasts-on-the-go/ and my Italian Braised Shoulder Chops are a fantastic comfort food that won’t spike blood sugar, and is a definite crowd pleaser http://sustainabledish.com/italian-braised-lamb-shoulder-chops-the-homegrown-paleo-cookbook/
60. Amy Gorin

A1: Many newly diagnosed patients think they have to severely cut back on carbs and/or remove all bread products from the diet. While people with diabetes do need to plan out their carbohydrate intake, they do not need to eliminate carbohydrates, which are an important macronutrient.
A2: You can definitely enjoy the time with family and friends! Make sure to continue to count your carbohydrates while you’re out. If you’re going to a gathering that someone is hosting at his or her house, then offer to bring a dish that is diabetes friendly, such as a plate of roasted vegetables.
A3: I love these Almond Pistachio Cocoa Bites because they are a super tasty and filling snack and deliver 5 grams of fiber (20 percent of the daily value) with no added sugar and just 12 grams of carbohydrates per ball.
61. Jodi Danen

A1: Many people think once they get comfortable with reading labels and measuring foods that they no longer need to do so and start guessing carb counts. Don't guess. Continue to read labels and measure foods watching for those hidden sources of carbs
A2: Have a plan in place before going, whether it is to a restaurant or party. If dining out, look at the menu online and decide what entree fits best into your meal plan, ask for substitutions if needed. Ask for sauces on the side, ask that they not serve the bread basket, and watch portion sizes. If attending a party and are not sure what will be served, bring a healthy dish to pass. Make simple choices when at the buffet table, go for whole foods such as shrimp, chicken, and fresh veggies which will not be loaded with salt, sugar or added fat.
A3: On of my favorite recipes is a Starbucks copycat recipe with a full serving of fresh fruit. Many coffee shop drinks are filled with added sugars and many people are looking for an alternative. This Strawberry Fizz is a fun option.
62. Chrissy Carroll

A1: People often fail to realize that sweeteners like honey, coconut sugar, and other proclaimed "natural" sweeteners are still sugar. I see it often in the online world with an abundance of recipes that claim to be "sugar free" yet include these ingredients. While there are some differences in the way that different types of sweeteners are processed in the body, I'd encourage anyone with diabetes to remember that these natural sweeteners still very much impact blood sugar.
A2: My first tip would be to think about social gatherings that don't necessarily revolve around food. Our society is often centered around dinner and drinks for socializing, but there are so many other activities we can engage in. Hiking, concerts, painting classes, fishing trips...there are so many options! One of my personal favorites is letting the inner child out at an indoor trampoline park.
Of course, if the plan is to go out to eat, there's no reason someone with diabetes can't enjoy a meal out. Try taking a look at the nutrition facts for the restaurant ahead of time to find something that fits your diet needs. Most chain restaurants have nutrition information easily available these days. If there's no info to refer to, a piece of lean protein (like a baked chicken breast or a grilled piece of fish) along with vegetables and perhaps half of a sweet potato is usually a wise choice.
A3: These thai lettuce wraps are a fabulous diabetes-friendly recipe. Using lettuce instead of tortillas reduces the carbohydrate count on this dish - it contains just 13 grams per serving - and adds a fresh crunch to the recipe. The cabbage apple slaw mixes sweet and tangy flavors to top the ground turkey. It all comes together wonderfully and at less than 300 calories per serving, it's a great portion-controlled option
63. Josée Sovinsky

A1: When it comes to diabetes, one of the biggest mistakes newly diagnosed people make is cutting out all sugars and carbs from their diet. Since diabetes involves having high blood sugars, I understand how people believe this is a positive approach. However, even with diabetes, our body needs sugar and carbohydrates for energy and optimal brain function.
A2: Living with diabetes shouldn't stop us from enjoying our lives. One strategy I suggest to clients when they eat out is to embrace mindful eating. This means asking yourself what you are hungry for, choosing foods that are both nourishing and pleasurable, savoring every bite, and trying your best to respect your fullness. It's also important to let go of any feelings of guilt or shame. You are allowed to enjoy delicious food!
A3: I love making apple oatmeal cookies (https://www.joseesovinskynutrition.com/blog/apple-oatmeal-cookies). This recipe is great for those with diabetes because the oats, whole wheat flour and apples add fibre which helps keep blood sugars from spiking. These cookies are very versatile: they can be a snack, a dessert or part of breakfast! Additionally, it's a perfect way to use those "not so fresh" apples and reduce waste. Enjoy!
64. Kim Melton

A1: The biggest mistake or misconception I see newly diagnosed people with diabetes make is that they believe that they have to completely restrict carbohydrates from their diet. The most common foods that come to mind are bread, potatoes and fruit. They also don’t realize that carbohydrates are also relatively high in foods like milk and dairy products.
A2: Eating and enjoying a meal out is possible if you follow these important tips:
- Timing. It’s helpful to know the time in which you will be eating in relation to the amount and type of insulin you use so plan ahead. You can often peruse the menu beforehand online to help you decide on the best choice.
- Know what’s in the food and if you don’t know, don’t be afraid to ask. It’s also ok to ask that less salt or butter be used in cooking.
- Ask for foods like salad dressings or condiments to be put on the side instead of in the food. Some condiments are loaded with sugar so they also need to be portioned out and used moderately.
- Be wary of serving sizes and stick with the same portion size you would normally eat and take the rest home. Many restaurants are notorious for heaping serving sizes that are two and three times what we would eat at home.
- Order foods that are not breaded or fried as they can add extra carbohydrates to your meal.
- Asking for substitutions is commonplace. Instead of fries or a loaded baked potato, see if you can get some vegetables in its place.
A3: Here is a favorite recipe from my website Spicy Chickpea and Spinach Curry. It is a good choice for diabetics because chickpeas are loaded with fiber and protein and have a lower glycemic index than beans and lentils. If you’re using a canned version, rinse them before using them to cut back on the salt. Also, anytime you can add some green leafy vegetables in your meals the better because they are loaded with important nutrients such as potassium, calcium and iron, magnesium, vitamin K, vitamin C, vitamin E and B vitamins. They also don’t add many carbohydrates to the meal and are packed with fiber which has a minimal effect on blood sugar.
65. Hana Klimczak

A1: In my experience, people newly diagnosed with diabetes are overwhelmed and scared and tend to avoid all foods containing carbohydrates out of fear that their blood sugars will go up. The truth is that people with diabetes can enjoy a variety of foods including complex carbohydrates, fruits and vegetables, lean protein and healthy fat. Eating mindfully, utilizing the plate model (½ pale filled with dark colored vegetables, ¼ plate whole grains and starches, ¼ plate protein) and keeping portion sizes in mind is a great way to help control blood sugars.
A2: When going out with friends be mindful of caloric beverages (alcoholic and non-alcoholic), sugar filled desserts and portion sizes of meals and appetizers. Try to order foods that have more fibre such as whole grains, fruits and vegetables, beans and lentils, as it can slow down the rise in blood sugars. If portion sizes at the restaurant are big, opt for family style dining and share the meals you order. Look for foods that are made using healthier cooking options such as baking, broiling and steaming, and avoid foods that have been deep fried. Be mindful: limit the amount of bread you eat while waiting for the food to arrive, stop eating (and ask the waiter to either take away the food or pack it to go) when you are no longer hungry. If you do want to treat yourself occasionally choose smaller portions (some desserts offer sample portions of their desserts) or share a treat with a friend.
A3: I like simple swaps that can make a standard meal healthier and more diabetic friendly. For example, instead of opting for a mac and cheese, exchange it for whole wheat pasta with a cheesy cauliflower sauce. This way you are reducing the amount of cheese you are using, are adding vegetables to the meal and making it more balanced, and adding fibre by using whole wheat pasta. These simple changes will help control your blood sugars and help you eat healthier one small step at a time.
66. Steve Parker

A1: A. Failure to understand that a radical change in diet is likely needed.
B. Failure to comprehend those highly-processed starches can be just as detrimental as concentrated sugars.
A2: Several options:
- Eat before or after the get-together.
- Bring your own food and beverages.
- Discretely inquire of the host what's on the menu to see if it's going to be compatible with your needs. (I personally would not ask the host to change their planned menu just to satisfy me, whether for diabetes, celiac disease, veganism, or pescatarianism)
- If you're the host, provide only (or predominantly) diabetes-friendly food and beverages. These are good for everybody!
A3: AMD vinaigrette, a recipe my wife and I put together. Vinaigrettes are easy to make and have more and better flavor than many commercial salad dressings. Too many commercial dressings contain unnecessary sugar. Plus, you can use healthful olive oil, not the usual industrial seed oils (e.g. canola, soy). The icing on the cake is that vinegar (in all vinaigrettes) tends to prevent excessive increases blood sugar levels after meals, according to research from Arizona State University published in 2010.
The recipe with more comments:
Classic vinaigrettes are very low in carbohydrate content. On the other hand, many commercial salad dressings are “enhanced” with added sugar, which you don’t need if you have diabetes.
Try AMD vinaigrette on salads, fresh vegetables, or as a marinade for chicken, fish, or beef. If using as a marinade, keep the entree/marinade combo in the refrigerator for 4–24 hours. Seasoned vinaigrettes taste even better if you let them sit for several hours after preparation.
I’ll warn you, this is pretty spicy. If you prefer less tang, either use less of the vinaigrette, or reduce these particular ingredients by half: lemon juice, salt, pepper, paprika, and mustard.
Ingredients:
2 garlic cloves (6 g), minced
juice from 1 lemon (40–50 ml)
⅔ cup (160 ml) extra virgin oil olive
4 tbsp (16 g or 60 ml) fresh parsley, finely chopped
1 tsp (5 ml) salt
1 tsp (5 ml) yellow mustard
1 tsp (5 ml) paprika
4 tbsp (60 ml) red wine or apple cider vinegar
Preparation:
In a bowl, combine all ingredients and whisk together. Alternatively, you can put all ingredients in a jar with a lid and shake vigorously—my preferred method. Let sit at room temperature for an hour, for flavors to meld. Then refrigerate. It should “keep” for at least 5 days in refrigerator. The olive oil will solidify, so take it out and set at room temperature for an hour before using. Shake before using.
Number of Servings: 6 servings of 2 tbsp (30 ml).
Nutritional Analysis:
98 % fat
2 % carbohydrate
0 % protein
220 calories
1.4 g carbohydrate
0.3 g fiber
1 g digestible carbohydrate
400 mg sodium
41 mg potassium
67. Rosie Schwartz, RD

A1: One very common mistake I see those with newly diagnosed diabetes make is to focus on only what they should cut out of the diets - what they should not be eating. Instead they should be looking at the foods to include in addition to eating more frequently through the day. For example instead of cutting out carbohydrates at meals, they should be including those foods that offer an assortment of health benefits along with the carbohydrate but also are more slowly digested and released more gradually into the bloodstream. Examples would be pulses such as lentils, chickpeas and dried beans, or whole grains such as barley or quinoa. Eating more often also helps to control blood sugar rather than going long periods without food.
A2: A tip for going out and enjoying the social situations is to not go out hungry. It's hard to be discriminating when you're starving. Having a bowl of broth-based soup with low calorie vegetables for example can help to tame a hearty appetite. Then it's easier to pick and choose and go for only small amounts of those decadent delights which could have a negative effect on blood sugar readings.
A3: Not only is this soup, from my book The Enlightened Eater’s Whole Foods Guide (Penguin USA), packed with nutrition but it’s also a perfect starter for any meal or an appetite tamer before heading out with family and friends. Keep some individual portions in labeled containers in your freezer for those times.
Mediterranean Vegetable Soup
Makes 6-8 servings
Ingredients:
1 tablespoon extra virgin olive oil
1 cup chopped onions
4 cloves garlic, finely chopped
1 cup diced carrots
2 stalks celery, diced
2 medium zucchinis, diced
5 cups low-sodium or sodium-reduced vegetable or chicken broth
1 28-oz can no-salt-added plum tomatoes with juices, pureed
2 tablespoons chopped fresh basil
2 tablespoons chopped fresh parsley
2 cups baby spinach or coarsely chopped Swiss chard
Salt and freshly ground pepper, to taste
Directions:
Heat the oil in a large heavy pot over medium heat. Add the onions and garlic; sauté until soft, about 5 minutes. Add carrot, celery and zucchini; cook until soft, about 10 minutes. Add vegetable or chicken broth, canned tomatoes, 2 tablespoons each chopped fresh basil and parsley, salt and freshly ground pepper. Bring to a boil; reduce heat and simmer, covered, for 30 minutes; stirring occasionally. Stir in chopped spinach or Swiss chard and continue to cook another 20 minutes. Season with salt and freshly ground pepper, to taste.
Per serving nutritional information:
Calories: 76
Protein: 4 grams
Fat: 3 grams
Saturated Fat: less than 1 gram
Carbohydrate: 12 grams
Fibre: 3 grams
Sodium: 300 milligrams
68. Emily Holdorf

A1: One common misconception I see is that people who are newly diagnosed with diabetes get hyper-focused on only looking at the amount of carbohydrates in a food and glaze over the rest of the nutrients. Just because a food may be low in carbohydrates and good for your blood sugar doesn’t mean it still doesn’t affect your health. When looking at a food, still take into consideration the amount of fat and protein, along with carbohydrates, to ensure you are choosing a nutritious item.
A2: Don’t fall into the trap of “saving up” your carbohydrate choices for a night out with family and friends. This will only lead to unbalanced blood sugars and dangerous side effects due to these changes in blood glucose levels. Keep your carbohydrate choices consistent throughout the day, as you would any other day of the week. Plan ahead for your night out by looking up the menu ahead of time to see what the restaurant offers. This way you can plan the rest of your meal choices accordingly. Also, if you’re going to drink alcohol make sure to eat a snack while drinking, use moderation, and don’t count the alcohol as a carbohydrate choice, if you practice carb counting. Be sure to check your blood sugars before, during, and after drinking since alcohol can cause hypoglycemia.
A3: My favorite diabetes friendly recipe is a snack that is super easy to make!
PB&B Rollups
Ingredients:
1 whole-wheat tortilla
1 banana
Peanut butter or your favorite nut butter
Directions:
Take peanut butter and spread a thin layer over the tortilla. Place banana on one edge of tortilla and roll it up. Cut rollup in half, tightly wrap one half and keep in refrigerator. Take your half & snack on-the-go!
I love this snack because it takes about 1 minute to prepare, it’s easy to take with you on the run, and it satisfies your sweet tooth while filling you up. Plus the fats and protein from the peanut butter help keep your blood sugars steady!
69. Allyson Krause

A1: When it comes to learning how to count carbohydrates, most newly diabetic individuals do not realize fruits and vegetables also are carbohydrates. Vegetables are easier to measure compared to fruits and learning each serving size of fruit can really make a difference.
A2: Going off the most common mistake, when it comes to maintaining your blood sugar levels it becomes essential to measure out your foods. You will be shocked at how much your normal serving sizes are compared to the recommended serving sizes. Becoming aware of your serving sizes can make a huge impact on your blood sugars. Fruits are always something I see individuals struggling with since blood sugar can spike easily with the average serving size. Also, I always recommend pairing a fruit with a protein to help have a steady blood sugar.
A3: We love chicken pot pies in my family and when my dad was diagnosed with diabetes, I started to look for ways to make our favorite dishes healthier for not just my dad but everyone. I found this chicken pot pie casserole and it is now a favorite in my family. I always add in more vegetables than what is recommended. Plus with having the biscuits on top, you can make the decision yourself about how much of the biscuits do you want or none at all.
70. Dan Keller
A1: The biggest mistake I see for diabetics who have just been diagnosed is trying to see how much sugar they are consuming. They need to realize that sugar itself is not the true culprit, although a big one.
A2: They suddenly cut off all sugar and add artificial sweeteners by the pound only to find out they have not done anything to lower their A1C. Tip is to cut carbs. Carbs, aka starch, are the biggest culprit in my opinion as it translates to sugars in the blood system. Cut out cold drinks, cut out fries, potato chips, most fried foods, and seriously cut back on carbs. Do an iodine test on a piece of food to see if it is starch. You might be surprised what is starchy.
A3: As far as a favorite recipe; a good salad containing spinach and chunks of your favorite protein and also I love adding slices of mandarin oranges.
71. Charmaine Jones

A1: The common mistake that individuals make who are newly diagnosed with diabetes is to stop eating carbohydrates, especially fruits! This is a huge misconception. For some reason, the number one foods item tossed are fruits. I don’t know why.
As a registered dietitian, I always have to explain to my clients that they can enjoy fruits, but in smaller portions. That is when I whip out my nutrition tools and start my lesson by using great resources such as MyPlate, food portion models, and carbohydrate counting, a simple system that helps my clients keep track of their daily intake of carbohydrates.
Once my clients realized that they can enjoy fruits and other carbohydrates and still live healthy with diabetes, they no longer feel deprived of eating foods they love.
A2: Enjoy your dinner outing with friends/family! You should. Don’t forget to stick to your diet regimen by:
- Planning your meal beforehand. Try to review the restaurant menu to see what items are available. Always stick with leaner options such as salmon and baked meats. Avoid entrée that are topped with creamy sauces. These entrees usually come loaded with calories.
- Sharing appetizers with your party.
- Asking for a small plate (A salad plate is ideal). Asking for small plates keep you in control of your food intake, especially with carbs! Eating with smaller plates will help you stay within your daily calorie recommendations without having you to count your calories.
- Having a chef or garden salad instead of warm bread and butter. Green leafy and non-starchy vegetables are typically free foods that people with comprised blood sugar can enjoy without worrying about spiking their blood sugar. Don’t forget to ask for dressings on the side.
- Requesting if the chef can serve you half of your entrée and place the other half in a take-home container. And, when your waiter raises his/her eyebrow, just say my registered dietitian said so.
- Ordering two sides of vegetables steamed with olive oil instead of butter.
- Ordering a plain baked sweet potato with condiments on the side. (If available)
And, if you drink, have one glass of wine (5 ounces), one lite beer (women) or two for men, and 1-2 ounces of spirit.
A3: My ultimate favorite diabetes friendly recipe is our Vanilla Poached Pear with Apricot Sauce with chocolate mousse made from avocado.
People living with diabetes refuse desserts because of the notion that desserts can make their condition worse, leading to food deprivation. This is not true! In fact, people living with diabetes can enjoy desserts and live a normal healthy life.
The most important thing when enjoying desserts is portion control. Having ½ cup of low-fat ice cream, 1 ounce of dark chocolate, 5 pieces of chocolate kisses, or even a small cupcake (about 1 ¾ ounce) will not send your blood sugar hay wild.
Following the general guidelines for controlling food portion prevents chronic illnesses such as diabetes, cancer, especially obesity. These guidelines were not only established for individuals living with diabetes but for all of us to follow.
My strongest recommendation is to always speak with your registered dietitian about how to incorporate healthy desserts/snacks into your daily meal plan.
72. Julie Perks

A1: I think the most common diet mistake newly diagnosed diabetic patients make is to assume that all their food needs to be bland and boring and mostly boiled tasteless food. Also, that there meals expenses are going to be much higher as they need to purchase “special” food. And also to assume their meals will be vastly different from others in their family. It is almost a defeat and sadness assuming a lifelong diet of boring food awaits them. I really enjoy discussing the diet with these clients and to assure them this doesn’t have to be the case.
A2: As with most “special” diets, preparation is always key. So if they are attending a braai (BBQ) or dinner and are asked to bring along something, always make sure this is something they can enjoy – so even if nothing else on the table is really suitable, they have brought along something they can enjoy. Also, educating family and friends that a diabetic diet is not too different from what most people should be enjoying in terms of a healthy diet so making sure they create delicious meal options and show family or friends that tasty foods can still be enjoyed.
Beverages are important as to what they choose to bring along – so no fizzy drinks and limited (if any) alcohol due to the risk of hypoglycaemia (raised blood sugar levels).
Pack healthy snacks when out and about and also something to raise sugar levels if they feel them going slow (this might be 2-3 sweets for example).
Choose restaurants that offer more balanced meals and avoid takeaways – often their “healthy” option actually will still not be suitable. Basically they are looking for an option with lots of fresh veggies or salad, with a lean protein and a healthy starch. If the client is well controlled and they are planning on attending a celebration (party or wedding) I often suggest they can indulge in dessert but ensure the rest of their day is well controlled and they reduce their starch portion at the main meal. These instances are special occasions and unfortunately cannot be all the time but there are delicious recipe books and recipes available on the internet where they will detail low GI desserts and puddings that the whole family can still enjoy. It really is just about mindfulness about food.
A3: I love pulses/legumes and they are amazing at lowering and controlling blood sugar levels because they contain such a wonderful amount of fibre and a little protein as well as being a healthy carb. In our home we eat a lot of meat free meals and this is one of my favourites – high in fibre and super tasty. The recipe is on my website: http://www.juliethedietitian.com/lentil-chickpea-coconut-milk-curry/
73. Michele Wroblewski, RDN

A1: A new diagnosis of diabetes can be very overwhelming, especially with misconceptions that you may hear from media, unreliable sources, etc. A couple of mistakes that I typically see involve completely eliminating carbohydrates or sugar, as well as overcompensating when hypoglycemia (low blood sugar) occurs. While it is important to monitor portion sizes, and include adequate amounts of protein and fiber in the patient’s intake to help keep blood sugars steady, it is far from necessary to completely eliminate carbohydrates. In addition, patients overcompensate with carbohydrates and simple sugars, such as orange juice, candy, and candy high in fat, which can either lead to heightened blood sugars, or no raise in blood sugar due to the presence of fat not allowing a quick rise in sugar. This is why a credible source, a Registered Dietitian Nutritionist, is important to consult in matters of nutrition and diabetes control.
A2: When it comes to blood sugar control, a huge factor in maintaining a normal blood sugar range is portion sizes, as well as the grams of carbohydrates consumed at one sitting. Planning ahead is very important so the patient is able to enjoy an occasional treat in moderation, such as a glass of wine or beer or a dessert. Typically, I will suggest to our patients to keep the balance by omitting the carbohydrate at dinner and choose a low carbohydrate vegetable in order to compensate for alcohol or a dessert, or I will recommend adding seltzer to any drink high in carbohydrates. We teach our patients how to incorporate the foods they love in moderation while still being able to control blood sugars and stay on the path to health! However, I always remind the patient that enjoying time with friends and family isn’t solely about the food; it’s about the people you are with! Focus on the people, not mindlessly snacking on chips and the loaf of bread served before dinner. However, if the patient felt that they wanted to have bread or pasta at dinner for the occasional trip out to the restaurant, we would discuss portion sizes (estimating a handful of pasta) and asking for the to go container immediately to bring the rest of the portion home.
A3: Here is a great recipe to try:
Slow Cooker Cilantro Lime Chicken
4 h 10 min Preparation Time
6 servings
272 calories per serving
Ingredients:
1 (16 ounce) jar salsa
1 (1.25 ounce) package dry taco seasoning mix
o OR Make your own taco seasoning with the following ingredients:
1 Tbsp. chili powder
1 tsp. ground cumin
1 tsp. garlic powder
1 tsp. paprika
½ tsp. oregano
½ tsp. onion powder
¼ tsp. salt
¼ tsp. black pepper
¼ tsp. crushed red pepper flakes
1 lime, juiced
3 tablespoons chopped fresh cilantro
3 pounds skinless, boneless chicken breast halves
Directions:
Place the salsa, taco seasoning, lime juice, and cilantro into a slow cooker, and stir to combine. Add the chicken breasts, and stir to coat with the salsa mixture. Cover the cooker, set to High, and cook until the chicken is very tender, about 4 hours. If desired, set cooker to Low and cook 6 to 8 hours. Shred chicken with 2 forks to serve.
This is one of my favorite recipes to share with our patients because it’s simple, requires few ingredients (or ingredients they already have in their cabinet), and is easy to make! Crock pots are a great way to cook food in bulk, especially in today’s world, due to lack of time to prepare a meal that is low in calories, carbohydrates, and that tastes good! I have yet to come across a patient that does not rave about this recipe! It was taken from http://allrecipes.com/recipe/218863/slow-cooker-cilantro-lime-chicken/
74. Lisa Musician, RD LDN

A1: Many newly diagnosed diabetics only look at sugar on a food label and don’t realize it’s the total carbohydrate that needs to be reviewed.
A2: One of the keys to maintaining controlled blood sugars is to eat consistently. I recommend eating the same amount of carbohydrates at each meal spaced evenly apart. Pack foods just in case a meal isn’t served on time and always carry glucose tabs to take if experiencing a low blood sugar.
A3: I don’t really have favorite diabetic friendly recipe because I believe any food can be incorporated into the meal plan.
75. EA Stewart, MBA, RD

A1: The biggest mistake I see newly diagnosed people with diabetes make, is thinking they need to completely overhaul their diets, and give up all of their favorite foods. Instead, my approach is to get a detailed food journal from my clients, along with their favorite foods, cooking knowledge, etc., and come up with a realistic meal plan that not only fits their lifestyle, but one that is sustainable, AND delicious.
A2: Educating my clients on how to cook or assemble a healthy, diabetes friendly meals, is the first step, so they feel comfortable with the food choices they make-both at, and away from home. This enables them to enjoy a special treat, but now they've learned to swap a whole plate of cookies, for a plate with 1 or 2 cookies, some veggies and hummus, and a handful of nuts-a meal that is much more blood sugar friendly!
A3: This recipe for Low Carb Rosemary Pecan Chicken Salad on Zucchini Chips is a favorite of mine because it's easy to make, it's naturally low in carbohydrates (but easily adaptable for non-diabetics who might want to eat this on bread instead of zucchini chips), it contains mostly heart healthy unsaturated fats, along with a little fiber, and it's absolutely delicious-my kids even love it too!
76. Brianna Elliott

A1: Not eating enough healthy fats and protein along with their meals (this is also a ‘diet mistake’ among those not diagnosed with diabetes as well!). Both protein and fat help to stabilize blood sugar levels, so that they don’t spike too quickly after eating. A key is to include a source of carbohydrate, fat and protein at every meal. Here is an example of a balanced meal: Chicken breast (protein) with brown rice and broccoli (carbohydrates), topped with olive oil (fat). Another mistake: missing sources of added sugar in their diets. Most newly diagnosed diabetics are pretty familiar with the fact that soda, candy, baked goods, etc. are high in sugar. However, not all of them are educated on the amount of added sugar in other common products, like salad dressings, yogurt and sauces. The sugar that is added to these foods can throw off blood sugar levels if you don’t take them into account. So I recommend for everyone to check food labels on everything to ensure they aren’t eating an excess amount of added sugar.
A2: Plan ahead! Those with diabetes can lead completely normal lives: it’s definitely not necessary to avoid social situations. If you are going out to eat, or to another gathering that involves food, think about what you can do to make it easier for you to make healthy choices. Can you look up the menu and nutrition information online, and decide what you’re going to order before you’re at the restaurant? Can you bring your own dish to share at a holiday get-together? Can you eat a healthy snack before you arrive, so that you’re not starving and tempted to eat anything and everything that’s available? Preparing yourself for the situation that’s to come will set you up for success.
A3: Spinach Quinoa Lasagna Casserole: http://fitfoodiefinds.com/2016/09/naked-spinach-quinoa-lasagna-casserole/
This recipe is great for everyone! I especially like it for diabetics because it’s high in fiber (6 grams per serving) and protein (22 grams per serving). I already talked about why protein is helpful for diabetes, but fiber is also great because it slows digestion and also prevents blood sugar levels from rising too quickly. It’s a vegetarian dish, with most of its protein coming from the quinoa and cheese. It’s also versatile, so if you’d like to some extra protein, like chicken, it is simple enough to do so!
Honestly my advice for diabetics isn’t much different than my advice for non-diabetics. It’s all about balance and being mindful of your food choices!
77. Elissa Lueckemeyer

A1: Being diagnosed with diabetes can be overwhelming at first, and I often see clients become fearful of eating any carbohydrates. Another misconception is that they have to give up their favorite foods forever, which understandably leaves them feeling very depressed. After educating on proper portion control, clients are able to find a balance that is right for them and learn how to still enjoy some of their favorites in a healthy way.
A2: A great way to stick to a diabetic eating plan when enjoying time out with friends and family is planning ahead. Know how many carbohydrate grams you can have each meal, and practice portion control. Even if the meal selections aren’t ideal, you can still keep your blood sugar in check by consuming the right portions. A registered dietitian can help you determine how much is right for you and teach you proper portion sizes. Also, whenever possible, take advantage of any physical activity on your outings. Even if it is just walking through a park or mall, or taking the stairs instead of the elevator, physical activity can help keep your blood sugar in check.
A3: There are so many delicious diabetes-friendly recipes out there. This chicken-garlic stir-fry recipe is quick to throw together, packed with flavor, low-carb, and a great source of lean protein.
Chicken-Garlic Stir Fry (adapted from Better Homes and Gardens Cookbook)
Ingredients:
1 package chicken breasts
1 cup water
3 Tablespoons low-sodium soy sauce
1 Tablespoon rice vinegar (can also substitute white wine vinegar)
1 Tablespoon corn starch
2 Tablespoons olive oil
1 package frozen stir-fry vegetables (This is where you can really get creative. I was in a hurry, but you can definitely go fresh instead. I love mine with water chestnuts and mushrooms.)
6 teaspoons minced garlic (sounds like a lot, but hey, it’s yummy, plus it’s is good for you. I use jarred, minced garlic because again, I’m usually in a hurry)
OPTIONAL: ½ tsp crushed red pepper (to add to marinade)
OPTIONAL: 1 cup cashews
2 cups hot cooked white, brown, jasmine, or basmati rice
Directions:
1. Cut chicken into ½ inch pieces and put into a Ziploc bag. For marinade, mix water, soy sauce, vinegar, and crushed red pepper if you want some spice.
2. Pour over chicken, seal, and refrigerate for at least 30 minutes. Drain chicken, but SAVE THE MARINADE. Don’t toss it.
3. Stir cornstarch into the marinade, set aside.
4. Heat olive oil in large skillet (or wok if you have one) over medium-high heat. Add vegetables and garlic, cook and stir until tender. Remove veggies from the pan.
5. Add chicken to the pan. Cook 2-3 minutes or until no longer pink. Stir the marinade mixture a bit more then add to the pan. Cook and stir until thickened and bubbly.
6. Return veggies to the pan. Add cashews if you’d fancy. Cook and stir until mixed well and all heated through.
7. Serve over rice. Remember that ⅓ cup of rice is about 15 grams of carbohydrate.
78. Rebecca Kourmouzi

A1: I see many diabetic patients skipping their meals or having inconsistent meal times. Also, there is a strong assumption among newly diagnosed patients who receive limited or no scientific dietary advice from a registered dietitian that they should cut all carbohydrates out from their diet. Both of these mistakes can be very dangerous for human health because if no carbohydrate-containing foods are consumed or when meals are skipped, hypoglycaemia occurs and consequently the human cells are not able to utilise glucose from food to produce energy. Due to the resulting hypoglycaemia, adrenaline is released causing symptoms of sweating, shaking, nausea, increased heart rate, irritability, tiredness and headache.
As hypoglycaemia progresses the organism starts synthesizing ketone bodies to provide energy to vital organs including the brain. Ketone bodies are toxic compounds and excess amount of them in the blood can cause confusion, lack of coordination, slurred speech, drowsiness and aggressions, and can eventually lead to convulsions, diabetic coma and death. It should be made clear to all diabetes patients that meals should be consistent throughout the day, and that the 50-55% of their total daily energy intake should be made of carbohydrates. Things that matter for blood glucose control are the amount (carbohydrate counting) and the types of carbohydrates consumed. Diabetic patients should mostly consume complex carbohydrates including wholegrain cereals and pulses, and try to avoid sugary foods and drinks as much as possible.
Low glycaemic index (GI) diets can significantly improve glycaemic control as they cause smaller fluctuations in glucose and insulin concentrations in the blood. Low GI foods include multigrain, granary and rye breads, muesli and porridge made with stone ground oats, sweet potatoes, al dente pasta, pulses, beans, legumes, peas, milk and yoghurt, apples, stone and citrus fruits, berries, plain sponge cake, and maize or corn chips. Other things that should be considered to achieve glycaemic control are the type of medication that is taken by each patient, the amount of insulin injected (carbohydrate counting and insulin adjustment) if any, as well as the patient’s daily physical activity levels.
A2: Many people become frustrated when they get diagnosed with diabetes because they believe that they will no longer be able to live a normal life. Living with such a condition should become easy if patients acquire healthy lifestyle habits on time. My tips for living a healthy and happy life with diabetes include:
- Eating regular meals throughout the day and managing portion sizes of each meal. A simple way to assess whether a main meal is balanced is to check that the ¼ of the plate contains complex carbohydrates, the ¼ lean meat or lean meat substitutes, and the ½ non-starchy vegetables.
- Swapping meat for beans, lentils and pulses is a good choice to reduce fat and increase fiber content of meals. Fiber helps manage cholesterol levels and prevent certain forms of cancer. When eating out, patients can choose meals containing beans and lentils, such as soups, stews, burgers etc. Fish is also an alternative choice to meat, as it is good source of low fat protein (white fish) and heart-protecting omega-3 fatty acids (oily fish).
- Reducing intake of all fats but especially saturated fats e.g. butter, cheese, processed meat and pastry, since these are linked with increasing cholesterol.
- Keeping foods containing sugar to an occasional treat and whenever possible choosing sugar free drinks. Artificial sweeteners are safe to use.
- Familiarizing one’s self with carbohydrate counting, as this can be a useful tool to help manage blood glucose levels. To get good blood glucose control patients need to be able to balance on a daily basis the amount of insulin with the amount of carbohydrates they eat. Each patient’s diabetes team will guide them towards achieving this.
- There is no reason why people with diabetes cannot have alcohol, unless they have been advised not to or are under age. The safe limits for alcohol are 14 units per week for either males or females, spread across at least three days a week. Alcohol can lower blood glucose and hypoglycaemia may develop up to 16 hours after the patient has stopped drinking. Therefore, it is essential not to drink on an empty stomach and if drinking in the evening, patients should have a small carbohydrate snack before going to bed. Also, the following day patients should not miss breakfast and make sure it contains carbohydrates e.g. cereal or toast.
- . Being more active and spending less time on sedentary behaviours(30 minutes of moderate physical activity undertaken at least for five days a week).
A3: One of the recipes that I always suggest to my diabetic patients is the butternut and borlotti bean stew. It is one of my favourites simply because it is very low in calories (217kcal per 454gr serving), salt (0.5g per 454gr serving),and sugar (14.6gr per 454gr serving) and at the same time it is full of nutritious ingredients such as lentils, beans, butternut squash, parsley, garlic etc. Each of its servings provides an appreciable amount of dietary fiber (11.4gr per 454gr serving) and protein (11.7gr per 454gr serving). It is also suitable for vegetarians and vegans as it contains no animal ingredients and it is very simple and quick to make. It takes approximately 15 minutes to prepare the ingredients and 30-35 minutes to cook the stew. Finally, apart from being highly nutritious it is also very tasty due to the addition of herbs (oregano, chilli, pepper and garlic) that give it a spicy, unique and delicious taste!
Ingredients:
1 tsp rapeseed oil
2 red onions, chopped
1 medium butternut squash, deseeded and peeled then chopped into cubes
1 green pepper, chopped
1 vegetable stock cube dissolved in 500ml water
2 x 400g cans tomatoes
50g dried red lentils
1 heaped tsp dried oregano
Good pinch of chili flakes
4 cloves garlic, crushed
2 x 400g cans borlotti beans, drained
Good grind of black pepper
1 tbsp. chopped parsley, to garnish
Instructions:
1. Heat the oil in a pan and add the onions, squash and green pepper. Stir regularly for 5 minutes until starting to brown.
2. Add the stock, tomatoes, red lentils, oregano, chilli and garlic. Bring to the boil, reduce the heat, add a lid and simmer for 10 minutes.
3. Add the beans and heat for a further 10 minutes, check the squash is cooked through (until tender). Serve with a good grind of black pepper and a sprinkle of parsley.
79. Jennifer McDaniel

A1: The number one mistake or misconception I see is the total avoidance of carbohydrates. Due to the fact that carbohydrates are converted into sugar, it can be understood why one would fear/demonize foods that contain carbs. However, one, not all carbs are created equally and two individuals with diabetes NEED carbohydrates as part of a well balanced diet to manage diabetes. The emphasis should be on high-quality, whole-food carbs, which contain blood-stabilizing fibers such as fruits, vegetables, whole-grains, dairy, and beans. In addition, meals should balance how MUCH carbohydrate is eaten at each meal.
A2: Diabetes should not be a barrier to life’s activities, but preparation should be prioritized. First, they might consider keeping a healthy carbohydrate snack on hand in case he/she needs to avoid a low blood sugar. If eating out, they might review the menu of where they will be eating. Most restaurants have online menus, and they could mentally prepare for a healthy order.
A3: I love any recipe that contains beans for diabetes. Beans are an affordable source of plant-based proteins that pack in lots of blood stabilizing fibers. In one study, people with Type 1 diabetes were able to use less insulin by 38% by eating beans.
To combat the cold winter weather, I recommend a vegetarian chili – here is one of my favorites: https://mcdanielnutrition.com/posts/pumpkin-chicken-chili
In addition to the beans, canned pumpkin is rich in vitamin A, C, and potassium. These nutrients promote healthy vision and blood pressure.
80. Katherine Mattox, RDN

A1: When I work with patients newly diagnosed with diabetes or pre-diabetes they usually feel overwhelmed with the diagnosis and the lifestyle changes recommended to manage their blood sugars. Without knowledge, support and accountability feeling overwhelmed can result in no action. I recommend that everyone seek the help of a registered dietitian and spend at least 5 to 6 hours face-to-face (or online) working to address their individual health goals and food preferences. As with mastering any new task it takes an appropriate amount of time to receive the necessary valuable education and support.
It is normal for a newly diagnosed diabetic to think about what they should avoid in their diet. Having an “attitude of gratitude” and thinking about all the delicious foods that help manage blood sugar and insulin levels will help a patient to make healthier decisions. One step further, I recommend working with a registered dietitian and learning about healthy foods that help insulin sensitivity. If you have the knowledge that eating more of the delicious high-antioxidant and high-fiber Cajun black bean soup with hot sauce is helpful for diabetes this is more motivating than thinking about having to limit the high sugar restaurant corn bread.
A2: I am a huge advocate of cooking and preparing meals at home. Cooking gives you control of the quality and ratios of ingredients and minimizes unhealthy fats, sugars, sodium and simply the temptation of less healthy food triggered by the restaurant environment. If you lack confidence in the kitchen, just following one new recipe a week will help introduce cooking techniques, flavor combinations and how to use new spices. If you eat at home 18-19 of your 21 meals per week this provides flexibility to enjoy restaurant foods socially on the weekends.
I like to talk about a “rule of 3” for restaurant meals. I have patients ideally choose 2 of these 3 items: alcohol, starchy carbohydrates (breads, rolls, fries, potatoes, rice) or dessert. If you enjoy a glass of wine and want to split a dessert with a friend forgo a baked potato and order vegetables instead or remove the bun from your burger and choose coleslaw instead of French fries. If you love French fries, still remove the bun, drink water or unsweetened ice tea. This rule of 3 doesn’t practice total restriction but helps patients to prioritize which higher sugar foods a patient may enjoy the most.
Another tip is to try to schedule exercise before or ideally after a big meal out. If you can choose to socialize with friends over lunch or brunch, invite everyone to take a walk after eating to help bring down your blood sugar. Also most restaurants have their menus available online and picking out what you want to eat ahead of time helps avoid unhealthy impulse decisions.
A3: My choice is both a recipe and a product. I like introducing my patients to 100% bean pastas. Made from organic black beans, green peas, chickpeas, soybeans, these pastas can be used in healthy high vegetable meals with a minimal impact on blood sugar thanks to an increased protein and fiber content compared to traditional pastas.
Try mixing in a can of unsweetened pumpkin to a jar of low sugar tomato sauce. Heat sauce in a skillet and serve this over cooked bean pasta for a fast high fiber diabetic friendly dinner option. Adding ground turkey or grass-fed ground beef is an option.
Similar idea: http://pinchofyum.com/creamy-pumpkin-spaghetti-with-garlic-kale. (use organic 100% bean, chickpea, green pea, lentil pastas).
81. Miechelle O'Brien, MD,PhD

A1: I often see patients in my office presenting with new symptoms of abdominal cramping, bloating and gas or a change in their bowel habits. This can be a to changes they’ve made to their diet, usually adding fiber, motivated by a desire to better control their diabetes, heart disease, or just general “healthier eating.” For most patients, the body adjusts to these dietary changes, and they do well. For those with irritable bowel syndrome (IBS) however, this can really make them miserable with pain, bloating or diarrhea.
I encourage these patients to continue eating a higher fiber diet; however educate them that some sources of fiber can be harder to tolerate than others in IBS. When this is the case, I review foods that are known to contain higher amounts of fermentable carbohydrates, known as FODMAPs (F= fermentable O=oligosaccharide D=disaccharide M=monosaccharides and P=polyols). FODMAPs cause symptoms when the enzymes in your intestines are not able to break down these carbohydrates and they continue traveling through the gut and are fermented into gas by bacteria or cause water to be drawn into the intestines.
This can lead to extreme discomfort and diarrhea or constipation. High FODMAP ingredients are often added to prepared or packaged foods to provide added fiber (inulin, or chicory root are common additives). It’s also the case that many artificial sweeteners such as those used in diabetic candies are FODMAPs (polyols). Examples include mannitol, sorbitol and xylitol. Polyols occur in nature as well, and can be found in apples, pears and avocados, among other foods.
A2: This information can at first seem very complicated and challenging to a patient who is newly diagnosed with diabetes and is just trying to do the right thing with his or her diet. I reassure my patients that after they learn to identify the foods/ingredients that bother them or make a few substitutions, they will feel much better. I encourage them to meet with a registered dietitian who is knowledgeable about GI-specific needs and the low-FODMAP diet so that they can help them with grocery lists and meal planning. It may take only one or two visits. It is possible to ‘have it all’- healthful diet and happy tummies!
A3: One of my favorite Diabetic Low-FODMAP snacks:
Lower-FODMAP Hummus
Hummus tastes great and is a healthy choice for managing blood sugars, but commercial hummus can sometimes be hard to digest. Enjoy flavorful hummus again with this IBS-friendly homemade version. Canned, drained chickpeas are lower in FODMAPs than those that are cooked from scratch or used in commercial hummus.
Ingredients:
1 (14.5 ounce) can chickpeas, drained and rinsed
2 tablespoons water
4 tablespoons fresh lemon juice
2 tablespoons peanut butter
2 tablespoons garlic-infused oil
1 teaspoon sesame oil, dark or spicy
½ teaspoon salt
Procedure:
Measure ingredients into the bowl of a blender or food processor in the order shown. Process until smooth and creamy. Transfer to a serving bowl and drizzle a little extra sesame oil on top to garnish. Serve immediately with fresh vegetables such as carrot sticks and sliced cucumbers.
Serves: 8
Nutrition (per serving): 141 calories, 7.5g total fat, 369.2mg sodium, 15.4g carbohydrates, 3g fiber, 4.2g protein
From IBS-Free Recipes for the Whole Family (2015, Pond Cove Press), by Lisa Rothstein, Patsy Catsos and Karen Warman.
82. Kristina LaRue

A1: Skipping meals or trying to eliminate carbohydrate foods are two biggest mistakes I see made by people newly diagnosed with diabetes. The key to diabetes control is balance of blood sugar. When you skip meals, you increase the risk for low blood sugar which makes you feel hungry and crave high simple carbohydrate foods (sugar). These foods spike blood sugar, causing a vicious cycle of highs and lows. The key to blood sugar control is eating a balanced diet based on your calorie needs. You are encouraged to eat carbohydrates for a balanced diet, not avoid them. The type of carbohydrate is important to maintain blood sugar control. Choose high fiber or whole grain carbohydrates, portions based on your personal calorie needs along with your balanced diet.
A2: This does not mean that you are not able to enjoy a snack high in sugar or simple carbohydrates in moderation. If you are out with friends and family its ok to choose a dessert. Be conscious of your portion size and pairings. It’s best to eat dessert with a meal rich in lean protein such as fish or chicken, and skip other carb sources at that meal like the bread basket or wine. This will help reduce the dramatic spike in blood sugar if you’d like to enjoy something sweet. Exercising after a meal is an excellent tool to avoid the spike and plummet by allowing your body to use the excess energy (sugar). Exercise is not only an important component of a healthy lifestyle but essential for weight loss and diabetes control.
A3: My favorite diabetes friendly recipe is: Turkey Taco Soup. This recipe is so delicious and easy. Best of all it is packed with high fiber vegetables and lean turkey to keep you full and energized without the blood sugar spike.
83. Sarah Schlichter

A1: The thing I most often hear from clients is the idea that they have to avoid carbohydrates all together, which isn’t the case. Sometimes they don’t hear the whole story from the doctor, or the doctor isn’t explaining the relationship between carbohydrates and blood sugar, and clients often walk away confused.
A2: I would give the same tips as I would to any ordinary person. Eat regularly to prevent blood sugar drops, and eat balanced meals and snacks. There should always be a source of protein and fiber in what you’re eating. There is room for sweets and social snacks, but it’s important to make sure there is some source of fiber and protein as well.
A3: I love recommending my Wild Blueberry Sweet Potato Bread to patients. It’s full of antioxidants, nutrients and heart healthy fiber from the blueberries, sweet potatoes and whole wheat flour. The protein and fiber in the bread both help to stabilize blood sugar, making it a great choice for those with diabetes to feel good about eating.
84. Andrea Miller

A1: One of the most common mistakes I see when someone is newly diagnosed is that they think they need to cut all sources of carbohydrates from their diet. Many people do not understand that a diagnosis of diabetes does not mean no carbs, but that it means healthy, higher fiber carbs spread out over all meals and snacks. They also do not realize that they can still enjoy small amounts of their favorite jam on their toast, or a little maple syrup in their yogurt.
A2: I encourage people to develop a consistent eating and activity routine that works for them. Consistency is one of the most important things in diabetes management. Eating at similar times of the day, and eating about the same amount of food at meals can really help with blood sugar management. Making time to socialize is important, but don’t make it all about the food. Enjoy time with friends and family, while eating healthy, well balanced meals is key. When eating out in restaurants, I encourage my clients to manage portions by bringing some food home for a lunch or dinner the next day.
A3: Here is a link to the recipe: http://www.cookspiration.com/recipe.aspx?perma=1p3lVA7mKgk&g=5
I like one pot meals, as they can be prepared ahead and used for more than one meal. This recipe is high in fiber and low in fat. It is made from ingredients that most of us might have in our fridge and pantry, all the time. It can be made ahead and frozen, and it can be seasoned to each individuals taste preferences. Chili is a ‘comfort food’ and often feels like good homemade food. I think it is important that people with diabetes understand that they can enjoy most of their favorite foods.
85. Jenna Obeid

A1: Avoiding carbohydrate foods all together. This is just not necessary.
Complex, low-GI carbohydrates are recommended in small serves at main meals throughout the day to sustain blood glucose levels. Think a serve of carbohydrate the size of your fist – for example basmati rice with dinner, or a piece of wholegrain bread with lunch.
Carbohydrates provide a range of nutrients as well as dietary fiber, which helps to keep us fuller for longer.
Also a common misconception is that patients cannot eat bananas. I am not too sure why people believe this! Bananas are more of a starchy piece of fruit, and when ripe do contain natural sugars, but there is definitely a place for bananas as part of a balanced diet – even if you do have diabetes!
A2: In order to keep blood sugars within an optimal range, I usually recommend eating certain serve sizes of the main food groups at each meal.
Aim for ½ of your lunch or dinner plate to be taken up with non-starchy vegetables or salad. This provides you with a range of micronutrients and fiber, and helps to fill your tummy up with light foods that promote a healthy body weight.
Then ¼ of your plate should be taken up with a small serve of lean protein (e.g. meat with the fat trimmed off, fish, poultry, tofu or eggs).
The last ¼ of your plate is where carbohydrates come into the mix. Include a low GI, complex carbohydrate such as basmati rice, whole meal couscous, noodles or pasta, a piece of grainy bread, or a starchy vegetable like potato or corn.
High sugar, discretionary foods are not recommended as part of a daily diet. But on special or social occasions they can be enjoyed from time to time.
Just keep in mind that if you require insulin, you are accounting for this when eating some higher carbohydrate based foods that aren’t usually part of your daily diet.
A3: I recommend to my patients to head over to the Diabetes Australia website for some healthy, diabetes-friendly recipes.
86. Katherine Ancona & Courtney Yablonsky

A1: There are a few common mistakes that we see newly diagnosed diabetics make. Many individuals assume now that all carbohydrates are off limits and try to avoid them completely. However, it is important for diabetics to consume them in order to keep their blood sugar balanced. Also, they start to skip meals thinking that it will balance their blood sugar; it is actually important to eat smaller meals throughout the day that will help to keep blood sugar under control. Lastly, these individuals do not seem to pair their carbs and protein foods; these should be consumed together because the protein helps to keep sugars steady, while carbs eaten alone can quickly spike sugars.
A2: Here are some tips:
- Just eat it
This might sound obvious, but majority of people are guilty of skipping meals at some point. The mindset behind skipping meals in order to save calories or cut carbs and fat, before consuming a calorically dense meal, can actually do more harm than good. Be sure to eat consistent meals throughout the day to maintain steady blood sugar levels, even if you plan on an outing with family or friends.
- Practice portion control
You can have your cake and eat it too, as long as it’s the proper portion size. Avoid wreaking havoc on your sugar levels by practicing portion control. Eating the proper serving size allows you to enjoy the food you want while balancing your blood sugar.
- Think before you drink
Foods are not the only carb-containing culprits to look out for. Before ordering that sweetened cocktail or sugary drink, think twice and opt for an option lower in sugar-laden calories that is more diabetic friendly.
A3: One of my favorite diabetic recipe is a turkey and vegetable chili. This is not only a budget-friendly and easy recipe, but also is full of nutrients as well! The lean turkey present provides healthy protein, the variety of beans give a healthy source of carbohydrates, and the vegetables (carrots, zucchini, onion, and tomatoes) add flavor. Plus, it can be enjoyed throughout the year; especially during these cold winter months!
Turkey and Veggie Chili
Ingredients:
Cooking spray
1 small onion, diced
2 medium carrots, diced
1 medium zucchini (6 ounces), diced
1 clove garlic, minced
16 oz lean ground turkey
1 (14.5 oz) can, no-salt-added diced tomatoes
1 (28 oz) can, no-salt-added crushed tomatoes
1 (15.8 oz) can great Northern beans, rinsed and drained
1 (15.25 oz) can no-salt-added kidney beans, rinsed and drained
½ tsp ground black pepper
1 Tbsp chili powder
1 tsp cumin
1 tsp garlic powder
Instructions:
1. Spray a large soup pot with cooking spray. Add the onions, carrots, and zucchini, and sauté over medium-high heat for 3-4 minutes or until the onions turn clear. Add the garlic and sauté 30 more seconds.
2. Add the ground turkey and cook until brown. Add the remaining ingredients; mix well and bring the chili to a boil. Reduce the heat and simmer for 15-20 minutes.
Note-References for questions 1 and 3 are:
http://www.diabetes.org/mfa-recipes/recipes/2015-03-turkey-and-veggiechili.html#sthash.NdadxH1v.dpuf
http://www.webmd.com/diabetes/features/overcoming-diabetes-diet-mistakes#1
87. Emily Kyle

A1: The biggest mistake I see people who are newly diagnosed with diabetes make is the immediate adaptation of 'food fear' and the thought that they may never be able to enjoy their favorite food and food groups again. A diagnosis of diabetes is most certainly overwhelming, but that does not mean you will never get to enjoy your favorite fruit or dessert again. It just takes some work with a qualified health care practitioner, like a registered dietitian, to figure out how you can still enjoy your favorite items in a way that works best with your individual needs and lifestyle.
A2: The best tip I have for enjoying times with family and friends when trying to keep your blood sugar under control is to adapt the practice of mindfulness. Mindful eating can help us to slow down, appreciate our food, our friends, the experience and our surroundings. This will in turn help you choose foods that are right for your body and your diabetes management.
A3: My sister is a Type 1 Diabetic and our most favorite meal to enjoy together is my Greens & Beans Stuffed Portabella Mushrooms (link to recipe: https://emilykylenutrition.com/greens-beans-stuffed-portabella-mushrooms/). This hearty and filling entree is plant-based and full of powerful plant-based phytonutrients, as well as complex carbohydrates from the beans to keep blood sugars steady and even after the meal has ended.
88. Julieanna Hever

A1: Because of the confusion brought about in the healthcare setting and in the media, many people quickly become afraid of foods containing carbohydrates. Yet, the most health-promoting foods tend to be high in carbohydrates. Foods such as vegetables, legumes, and whole grains, which are not only safe for diabetes, but incredibly beneficial for improving blood sugar control. Until the term "carbohydrates" ceases to be used as a food group, this dangerous mistake will persist. Though nobody can argue that a sugary cereal is metabolically equivalent to a lentil stew, lumping these foods into the haphazard category of carbohydrates is the norm. Instead, with a new diagnosis of diabetes (or to avoid the diagnosis or to gain control over blood sugar after a diagnosis), it is optimal to focus on constructing your diet on whole plant foods.
A2: Food is the centerpiece of celebration, whether it is merely a meal out, a birthday or anniversary, a holiday, a sporting event, or myriad other endless opportunities. Further, these occasions tend to highlight highly processed, rich foods that are dangerous to diabetes and overall long-term health. Unless the experience is truly unusual and a "special" special occasion, indulging on a regular basis will not help you reach your goals. To avoid setting yourself up for a difficult outing, where friends or family are feasting on foods you need to avoid, prepare ahead. Eat a healthy meal before going and then order something very light and healthful or sip on a sparkling water or tea while you are there. Remember that you do not actually have to eat to celebrate. You can connect with your company without food. It may feel awkward the first few times, but it soon becomes natural and is rather empowering. You can also bring along your meal and explain to anyone who asks that you are choosing to eat to support your health. Either way, if you arrive hungry without a healthy option, you are setting yourself up for a precarious situation that your natural biology will encourage you to make less than ideal decisions. Preparation is everything for optimal health.
A3: This is one of my favorite all-time recipes, and it is from my last book, The Vegiterranean Diet. It is wonderfully nutritious and delicious for anyone because it is rich in fiber (which helps temper blood glucose) and phytonutrients (to protect cardiovascular health and immune function) plus it is satisfying and filled with vitamins, minerals, and antioxidants:
Hearty Red Lentil Stew
My favorite one pot wonder, a hearty, earthy, chunky stew exploding with flavor and texture. Enjoy with a piece of Stoneground Cornbread and a sprinkle of Parma Shake. This is the perfect meal for entertaining guests or for just feeding a hungry home.
Makes 6 to 8 servings
Ingredients:
1 ½ cups chopped onion
1 ½ cups chopped (red) bell pepper
1 to 2 minced garlic cloves
4 cups vegetable broth or water, divided
1 ½ tablespoons chili powder
1 teaspoon ground cumin
1 teaspoon smoked paprika
½ teaspoon ground chipotle powder
¼ teaspoon crushed red chili flakes
2 cups red lentils, rinsed
1 (28-ounce) can fire-roasted crushed tomatoes (plain is fine, too)
1 (15-ounce) can chickpeas, drained and rinsed
1 (8-ounce) package of tempeh, cubed
2 tablespoons freshly squeezed lemon (or lime) juice and zest
¼ cup chopped fresh cilantro (or Italian parsley), as garnish
Directions:
1. In a large soup pot, sauté onion, bell pepper, and garlic in ½ cup vegetable broth over medium-high heat, until onions are translucent, approximately 5 minutes. Add chili powder, cumin, paprika, chipotle powder, and red chili flakes, and cook for an additional minute.
2. Add lentils, crushed tomatoes, remaining 3 ½ cups vegetable broth, chickpeas, and tempeh and lower heat. Cover slightly and bring to a boil. Once boiling, reduce heat and simmer until lentils are soft, approximately 30 minutes, stirring occasionally.
3. Pour in lemon juice, zest, and sprinkle with cilantro leaves. Add salt or pepper, to taste. Serve warm.
Please reference me as Julieanna Hever, MS, RD, CPT, author of The Vegiterranean Diet, The Complete Idiot's Guide to Plant-Based Nutrition, and host of Z Living's What Would Julieanna Do?
89. Cara Harbstreet

A1: Some newly diagnosed patients dive right into diabetes management - they’re highly motivated and ready to change right from the start. But they can sometimes try to change too much at once. While they’re overhauling their diet, adding new exercise, creating new habits, and juggling life in general, it can become overwhelming. Small changes spread over time add up so I encourage patients to focus on just one or two things at a time. Once they’ve mastered a new skill or become comfortable with a lifestyle change, we move on to the next one. This allows time to truly learn what it means to live with diabetes and prevent burnout.
A2: Life is about compromises and enjoying life with diabetes is no different. Instead of going to the extremes (complete avoidance and deprivation, or saying “who cares?” and going overboard), try to strike a balance. I frame this as Either/Or.
When presented with food choices, we can still enjoy the things we love without giving them up completely. By giving ourselves the option of choosing either THIS or THAT, we retain a sense of normalcy and inclusion in these social events. We can be more present and enjoy the time spent with people we care about rather than agonizing over what we can’t have.
A3: My Slow Cooker Sweet Potato Chili has been a hit with many of my clients. It’s simple to make but packed with balanced nutrition. It provides fiber, plant-based and animal protein, several types of veggies, and a low-sugar/protein packed replacement for sour cream. It’s satisfying and filling so a little goes a long way! Find the full recipe HERE.
90. Marcia Pell

A1: The most common diabetes diet mistake I see is trying to keep carbohydrate as low as possible in order to keep the glucose low. When this happens the diet is not balanced and generally has too much protein, saturated fat and not enough fiber and heart healthy plant based foods. Some people have even thought pork rinds were a free food because they had no carbohydrate! That is really missing the mark on a healthy diet. Lastly, some people think carbohydrate is limited to white potatoes, white rice, white bread and pasta.
A2: It's important that your diabetes doesn't stop you from doing the important things in life. Often planning ahead keeps you feeling your best. If you have a meal schedule that works well for you, try to stay with it as much as possible. You may need to take a snack if you are more active or meal time is delayed. If you take mealtime insulin, remember to have it with you. You may be able to go online to see the carb content of what you plan to eat later to make dosing easier. Consider splitting a meal or taking half home.
OR you can take a short “diabetes vacation" and ignore your diabetes for a little while. Decide if this is worth it to you, tell someone and have an ending time to your "vacation". For instance, just for tonight I'm going to ignore my diabetes and I will get back on track in the morning. Some people find short occasional vacations helpful in dealing with relentless diabetes care.
A3: This recipe by Chef and RD Michelle Dudash is one of my favorites. It's quick to make and keeps in the refrigerator for up to a month. They are convenient for snacks and contain only "real foods".
91. Dina Garcia

A1: Here are mistakes.
- They try to cut out all carbs instead of learning how to choose better carbs and how to balance them with the rest of their diet. Carbohydrates from high fiber whole foods --such as legumes, quinoa, sweet potato, whole grains, fruits and veggies-- help to feed the beneficial bacteria in the digestive tract. As the good bacteria in your colon ferment different fibers the bi-product is short-chain fatty acids which can actually help regulate blood sugar levels long term.
- They instantly switch the diet or sugar-free version of everything. When we consume food or beverage that is sweet we stimulate the brain to desire more sugar and refined carbs. So whether you're stimulating the "sweet spot" in your brain by consuming diet soda vs regular soda, you’re still stimulating it. Now when you go to have a "treat" you will need more of it to satisfy your sweet tooth. So instead of working to cut out the sugar work to cut out the sweet. Rather than swap jelly for sugar-free jelly consider smashing avocado on your toast or spreading almond butter on it. Then when you do want to indulge in a sweet treat in moderation you'll be more likely to find that a small portion more than satisfies your sweet tooth.
A2: Practicing mindful eating can play a big role in helping you to maintain a sense of normalcy when it comes to enjoying life (parties, vacations, weekends, etc). Mindful eating is about so much more than slowing down and enjoying your food. It also increases self awareness around how much food you need to feel satisfied and helps you work on the mental self-talk that drives your decisions on when, what, why and how much to eat.
A3: Recipe
PF3 Pancakes
Ingredients:
2 eggs
1 banana (if it's still a little green even better)
⅓ uncooked oatmeal
2 tbsp of chia seeds
1 pinch of light salt
Cinnamon and vanilla extract as desired
Topping- almond butter
Directions:
Put all ingredients in a blender and blend until smooth. Prepare on a griddle or in a skillet as you would normally prepare pancakes. Top with almond butter.
I love this recipe because it is PF3 balanced. PF3 is a term I coined that stands for protein, fat, fiber and fluid. When we combine these nutrients into our meals it helps to control our blood sugar levels. As a former pre-diabetic I am very conscious to consume foods that leave me satiated and with stable blood sugar levels. This recipe gives you protein from the egg, healthy fat from the chia seeds and almond butter and fiber from the banana, oatmeal and also the chia seeds. Chia seeds and oatmeal both contain soluble fiber which has been shown to improve blood sugar levels. If you use a slightly green banana you are also getting some resistant starch which helps the beneficial bacteria in gut produce short-chain fatty acids and create longer lasting satiety. When I eat these on Saturday mornings with my kids sometimes I forget about lunch until late afternoon because I don't get hungry until then.
92. Janice Cohen

A1: Many of my patients will eliminate grains, cereals and starchy vegetables completely.
A2: I tell my patients to have a roster of restaurants and menu items from each restaurant that they can depend as healthy options. This takes the guess work out of having to make on the spot decisions.
I also tell them to "keep their plate clean." No drippy or goopy sauces slushing around the plate. This would be indicative of a sauce that is starchy or sweetened.
I let them know that food that is compartmentalized is often the best option, brochette, rice, salad for example...with sauces and dressings on the side and maybe fruit and cheese for dessert.
A3: So I truly believe that the cooking methods dictate whether a recipe is appropriate or not as well as portion size. To keep it simple I like the idea of soups that serve as a meal: beef and barley soup, chicken noodle soup, vegetable, lentil soup...This way you know that you have a good balance of protein to carbohydrate ratio and you know exactly what and how much of each item you are consuming per meal. It is also warm and comforting on a cold winter night.
Easy Breezy Chicken and Noodle/Rice soup
Ingredients:
6 cups of low sodium chicken broth (with surface fat removed if homemade)
1.5 cup shredded cooked chicken
2 cup favourite boiled vegetables
1 cup of cooked rice or noodles
serves 1 extra large portion or 2 regular portions
Heat through and there you go, a meal in a bowl. Finish with fruit.
93. Whitney English

A1: The biggest mistake I see people with newly diagnosed diabetes make is cutting out all carbohydrates. Many people receive incorrect information that controlling blood sugar means getting rid of all sources of carbohydrates, including healthy sources like whole grains. This is completely untrue. While patients are advised to cut back on simple carbohydrates like soda, candy, and processed foods, a balanced and consistent carbohydrate intake, full of nutritious sources of carbs like vegetables, whole fruit, whole grains, and legumes is the goal - not complete avoidance of an important food group.
A2: I would advise them to learn to use a diabetic exchange list to estimate how many carb servings they can have each meal. That way when they go out to eat they can easily figure out the best choices for their plan. I would also advise them to plan ahead. Look at a menu before you go out to eat and make a game plan of what you want to order so it’s easier when you get there.
A3: I love this recipe because it has a nice balance of whole grains, lean protein, and healthy fat. It's full of fiber to support stable blood sugar levels and increase satiety. It also shows people that eating healthy doesn't mean giving up their favorite cuisine - like Mexican food in this instance!
94. Amanda K. Foti

A1: Often when individuals get diagnosed with diabetes they start to think “sugar-free” everything will help me manage my diabetes. They might continue eating the same foods they used to but opt for the sugar free version. Reducing and limiting sugar intake certainly helps but healthy diabetes management requires adjustments in diet, exercise and weight loss. The thought process is that sugar intake causes glucose spikes and drops, so take away the sugar and you’ll be good. However, research is now starting to show that artificial sweeteners may affect blood glucose levels like regular sugar. Another mistake I’ve seen is thinking that medication is the only thing that can manage diabetes. Although medications can help, diabetes is in fact a lifestyle disease that can be managed alone by diet, exercise and maintaining a healthy weight.
A2: Managing diabetes with diet and exercise requires mindfulness about what and how much you are eating. Self-monitoring is incredibly powerful when it comes to being in tune with your diet and health. I would recommending food tracking with an app (or journal) and weigh themselves regularly. Check out Healthie, where you can take pictures of your meals rather than log calories. When you start to be the one in control and are mindful of your choices you can then start to make changes. In addition to being mindful, eating smaller portions will go a long way. For example you don’t have to give up chocolate altogether because it has sugar, or avoid pasta- you just have to make sure you’re not doing too much. For most diabetics you want to limit carb intake to 45g for meals and 15 for snacks. If you’re used to having a whole chocolate bar opt to have 1-2 Hershey kisses instead. Or if you love having a big bowl of pasta- pull it back to 1 small scoop to get the satisfaction and load up on other protein and veggie options. If you really feel lost, working with an expert like a dietitian can have tremendous benefits.
A3: Protein pancakes! Who doesn’t love pancakes on a lazy Saturday morning? Managing diabetes does not have to mean giving up all the stuff you love. Instead, scramble up 2 eggs, ½ mashed banana, and ¼ cup of quinoa. Cook like a regular pancake on a skillet. I usually top it with a little nut butter spread- delish! Less than 30g carbs.
95. Micah Lacerte

A1: Common mistakes I see with people newly diagnosed with diabetes is not making the nutrition changes needed to help reverse the issue (type 2). Type 2 is a controllable issue so if you start eating right and eliminate the bad foods from everyday life your health will progress in a positive way and you will eliminate diabetes.
A2: You need to be conscious of the choices you’re making, if you know that super heavy sugar meals are going to spike your blood sugar levels then you need to opt for healthy low sugar alternatives. You can still have fun and be healthy on the weekends. Diabetes is a very serious matter and if not taken care of can cause permanent issues.
A3: 4 Ounces of Grilled Chicken with Your Favorite Non Sugar Seasoning, 4 Ounces of Sweet potato with sprinkle cinnamon and a cup of green beans!!
Healthy and Tasty!!
96. Katrina Pace

A1: Often people who have just been diagnosed with both Type 1 and Type 2 diabetes just freeze and get so overwhelmed with information (and contradictory information) that they don't know what to do or where to begin with making changes to their diet. With the recent discussions on carbohydrates I see clients who are really confused about whether they can or can't eat carbohydrates - everyone seems to have an opinion and there has been a growing distrust of what health care professionals say. My clients find it really reassuring to see a registered health professional who is able to tailor dietary advice to their needs. I would recommend that everyone try and find a trusted health professional who is able to answer their questions about all the current dietary choices. One size dietary advice doesn't fit all and it's not appropriate to make it fit everyone. Luckily the ADA acknowledges this. The biggest mistake I see is people trying to make ten different dietary changes at once. They end up doing none of them well, getting confused and disheartened and going back to their old habits really quickly. Make one change at a time and get the help of a registered dietitian or nutritionist to help you prioritize dietary changes.
A2: Stress can put your blood sugars up more than food sometimes! So as hard as it might seem, don't stress the blood sugars. Realize it is all about what happens 80% of the time and that special occasions do happen. Having said this it is important - for everyone, not just people with all kinds of diabetes, to not over indulge. Practical tips that help include choosing a smaller plate to fill. No diet drinks? Water is best. Social gatherings don't need to be around food - get everyone active instead. Enlist the help of friends and family in keeping your motivation up.
A3: All recipes can be "diabetic friendly". Some of my old-time diabetic recipes have now become family favorites and everyone has forgotten they came out of a diabetes cook book! I love this bean salad recipe for summer. The fiber in the beans is really filling and helps stabilize blood sugar levels. Also, the fiber is really good for the bacteria in your gut, and growing the right bacteria in your gut is very important for people with type 1 and especially type 2 diabetes.
Bean Salad
Ingredients:
1 x 400g tin of mixed beans - drained (in brine, not flavoured sauce). Or you can soak and boil 1 cup of dried mixed beans
½ cup chopped corriander leaves
1 cup chopped baby spinach
2 chopped tomatoes
1 small cucumber, chopped in to cubes
½ cup chopped feta cheese
Instructions:
Mix all ingredients together. Mix through 1 tsp balsamic vinegar and serve. Mix through 2 tbsp sauerkraut for even more good bacteria
97. Andy De Santis

A1: I think one of the more common mistakes or misconceptions that I encounter when it comes to diabetes is an overwhelming fear of carbohydrate consumption. Carbohydrate avoidance is not a treatment for diabetes, but choosing the right carbohydrates in the right amounts at the right time is. It is important for people to recognize that the consumption of high fibre, nutrient dense carbohydrates such as fruits, veggies and whole grains is absolutely critical to their health and longevity. With that being said, a dietitian with the certified diabetes educator designation will be best be able to help individuals learn how to incorporate these foods into their routine in the most appropriate manner possible.
A2: Although it is easier said than done, people living with diabetes should try to maintain the same healthy eating habits they do at home when they go out.
Here are a few of my suggestions on how to do this:
- If you are going to a restaurant, look up the menu and nutrition information ahead of time to help you make informed choices.
- Work on your portion estimation skills; this is especially important for those living with diabetes requiring insulin. The better you are at visually estimating the amount of carbohydrate in foods, the more versatile you will be when going out.
- Understand how alcohol can impact your blood glucose levels. This cannot be understated, especially in those using insulin. I highly recommend reviewing the following resource as well as speaking with the practitioners responsible for your diabetes care.
- Don’t be afraid to pre-eat or pre-snack if you feel uncomfortable about the food being served at the event or venue you are going to be. Just be sure to adjust your insulin accordingly as required and avoid skipping meals or snacks.
A3: I have one particular recipe in my mind that is featured on my website. It happens to be an excellent healthy choice for just about anyone. You can check it out by clicking here.
98. Jodi Robinson

A1: Here is my list:
- Thinking that carbs are the enemy and need to be avoided
- Looking at food labels only for sugar (and not total carbohydrates)
- Not establishing a consistent eating schedule
- Not testing blood sugars to check how they’re responding to their diet
A2: Allow yourself to eat what everyone else is but use the Plate Model (½ plate veggies, ¼ plate whole grain or starchy veg, ¼ plate meat or protein alternative) to guide your meal choices. This offers flexibility to include your favorite foods during any family outings or celebrations. For instance, if everyone is having pizza, have 1-2 slices (instead of 3-4) and pair with a large garden salad.
A3: White Chicken Chlii - http://www.cravinghealth.ca/recipe/white-chicken-chili
It’s high in fiber and rich in protein to offer a filling effect while helping control blood sugar levels.
99. Dr Megan Rossi
A1: People fearing carbohydrates. Complex carbohydrates such as those found in wholegrains, fruit and vegetables are an important source of dietary fiber which is not only good for gut health but helps control blood sugars. On the other end of the carbohydrate spectrum, the highly processed foods such as sweet biscuits and cakes should only be consumed occasionally and in moderation (but that goes for everyone- not just people with diabetes!). Even still no food or food group should be feared.
A2: When we go out for a meal we are more likely to over eat. Here are my four tips on ways to stay in control:
- Enjoy a high fiber snack before you go out- we tend to over order and over indulge when we are ravenous.
- Try to avoid all you can eat buffets- studies show we eat more when faced with too many options
- Order a side of steam vegetables or salad with your meal- fill up on the lighter stuff
- If you can’t say no to the dessert menu, share with a friend or get it takeaway and enjoy it the next day.
A3: This Gut-Busting Bircher Muesli is all about gut health, loaded with prebiotics this breakfast is the ideal meal to feed your good gut bacteria. Why is this important for diabetes? Did you know the health of your gut can impact your blood glucose control? In fact emerging research suggests your gut health may hold the answer to new diabetic treatments…stay tuned!
100. Caroline Susie

A1: The biggest mistake I see is the complete elimination of ALL carbs. It breaks my heart when I see someone who loves whole wheat pasta or potatoes think they can never have that food again. It brings me such joy to educate folks on how to incorporate carbs into their meal plan. (I too am a carb lover, so I get it!)
A2: Not having a plan is a plan to fail. If you know you have a birthday party tonight or a gathering Sunday after church, plan ahead! Can you bring a healthy dish? Can you go for a 10 minute walk before the meal? Be sure you exercise the day of your event and stick to your meal plan recommended by your CDE and or dietitian. Most diabetics have 30-60 grams of carb at each meal. Treat that like money! Once you have spent your carb money, you are out. No I.O.Us! Be extremely mindful of your serving sizes and if you have over done it, follow your treatment plan. Check your blood sugar; go for a 10 minute walk, etc.
A3: Chicken fajitas! I'm from Dallas so we love all things Tex mex. Working full time, I am no fuss dietitian. Is it easy and tasty? Sign me up! I love this super simple chicken fajitas recipe. You can serve this chicken in tortillas, alone, or over a salad. Very versatile! It's diabetic friendly as the only carb is the tortilla. So patients are in control as to what tortilla they want to choose (corn, whole wheat, carb balance, etc).
Ingredients:
Boneless skinless chicken breasts (3-4)
Whole wheat tortillas or corn tortillas
Sliced bell peppers and onions (I use ½ an onion and 2 bell peppers)
EVOO
1 package low sodium taco seasoning
Optional avocado slice (⅛ an avocado is a serving)
Toss chicken breast with ½ -¾ packet of taco seasoning (more = more spice so watch out if you have a more bland palate). Place on a foil lined baking sheet and bake at 350 for 45 minutes until juices run clear.
With 15 minutes left on the chicken, sauté peppers and onion with EVOO and S&P in skillet.
Build your fajita with chicken, peppers and 1 slice of avocado. Serve with side salad and enjoy!
101. Amanda Leendertse

A1: There are two types of mistakes I see people with diabetes make in the beginning, and they exist on opposite ends of the spectrum. On one side you have the person who makes drastic, unsustainable lifestyle changes (such as the complete elimination of carbohydrates), whereas on the other hand you have the person who chooses to ignore the diagnosis all together. Motivation to make lifestyle changes is fantastic, but in order to control diabetes over the long term, it is important the changes are maintained. Choosing to not make any lifestyle changes at all can also greatly increase the risk of life altering diabetes complications that are irreversible in the future.
A2: My biggest tip is that people educate themselves regarding carbohydrate-containing foods, and which of these foods are higher in fiber/raise blood sugars slower. I would also suggest that the person be familiar with the place they may be dining at, and if there are healthy options available. Diabetes shouldn’t isolate people from social gatherings or time with friends, but it is still important to make informed decisions. Following The Healthy Plate when dining out is also a simple and helpful tool.
A3: My favorite recipe is my Make-Ahead Breakfast Burritos recipe. This recipe’s high fiber and protein content helps to control blood sugars, as well as provides a tasty and satisfying breakfast. These can also be made ahead of time, so they are the perfect option for busy people on the go. The link to this recipe can be found here: http://www.fueledfork.com/single-post/2017/01/18/Time-Saving-Breakfast-Burritos
Hope you enjoyed these recipes.
TheDiabetesCouncil Article | Reviewed by Dr. Christine Traxler MD on June 2, 2020